Podcast
Questions and Answers
Which feature distinguishes secondary osteoarthritis from primary osteoarthritis in terms of joint involvement?
Which feature distinguishes secondary osteoarthritis from primary osteoarthritis in terms of joint involvement?
- Secondary osteoarthritis is limited to the hip and spine.
- Primary osteoarthritis affects only certain joints, while secondary osteoarthritis can affect any joint. (correct)
- Secondary osteoarthritis exclusively affects the knee joint.
- Primary osteoarthritis always affects multiple joints, while secondary osteoarthritis is limited to a single joint.
What is the primary underlying process in the pathology of osteoarthritis affecting the articular cartilage?
What is the primary underlying process in the pathology of osteoarthritis affecting the articular cartilage?
- Increased deposition of collagen fibers, thickening the cartilage
- Fibrillation, leading to clefts and eventual loss of cartilage (correct)
- Calcification of the cartilage matrix
- Rapid regeneration of chondrocytes, causing cartilage overgrowth
In osteoarthritis, what changes are typically observed in the synovial membrane?
In osteoarthritis, what changes are typically observed in the synovial membrane?
- Calcification and hardening of the membrane
- Atrophy and decreased vascularity
- Increased thickness due to hypertrophy and fibrosis, potentially leading to contracture (correct)
- Increased production of synovial fluid, causing significant swelling
Which of the following is a typical radiographic finding in a patient diagnosed with osteoarthritis?
Which of the following is a typical radiographic finding in a patient diagnosed with osteoarthritis?
Which statement accurately describes the pattern of joint pain associated with osteoarthritis as the disease progresses?
Which statement accurately describes the pattern of joint pain associated with osteoarthritis as the disease progresses?
What is the significance of Heberden's nodes in the clinical presentation of osteoarthritis?
What is the significance of Heberden's nodes in the clinical presentation of osteoarthritis?
What is the typical characteristic of morning stiffness in osteoarthritis, compared to other arthritic conditions?
What is the typical characteristic of morning stiffness in osteoarthritis, compared to other arthritic conditions?
Why is weight reduction often recommended as part of the management for individuals with osteoarthritis?
Why is weight reduction often recommended as part of the management for individuals with osteoarthritis?
Which of the following represents an appropriate initial non-pharmacological intervention for managing osteoarthritis-related pain?
Which of the following represents an appropriate initial non-pharmacological intervention for managing osteoarthritis-related pain?
What is the primary goal of using simple analgesics in the management of osteoarthritis?
What is the primary goal of using simple analgesics in the management of osteoarthritis?
What is the rationale behind using assistive devices, such as a cane or a brace, in managing osteoarthritis?
What is the rationale behind using assistive devices, such as a cane or a brace, in managing osteoarthritis?
In the context of physiotherapy for osteoarthritis, what benefit does electrical stimulation provide?
In the context of physiotherapy for osteoarthritis, what benefit does electrical stimulation provide?
Besides joint pain and cartilage degeneration, which of the following is a key component in the definition of osteoarthritis?
Besides joint pain and cartilage degeneration, which of the following is a key component in the definition of osteoarthritis?
Which of the following joint distributions is most commonly affected in osteoarthritis?
Which of the following joint distributions is most commonly affected in osteoarthritis?
What is the primary purpose of Osteotomy in the surgical management of osteoarthritis?
What is the primary purpose of Osteotomy in the surgical management of osteoarthritis?
Which of the following scenarios best illustrates the pathophysiology of osteoarthritis at the molecular level?
Which of the following scenarios best illustrates the pathophysiology of osteoarthritis at the molecular level?
A 70-year-old patient presents with joint pain. Considering the classification of osteoarthritis, which of the following factors would most strongly suggest a diagnosis of secondary osteoarthritis rather than primary osteoarthritis?
A 70-year-old patient presents with joint pain. Considering the classification of osteoarthritis, which of the following factors would most strongly suggest a diagnosis of secondary osteoarthritis rather than primary osteoarthritis?
In the context of osteoarthritis pathology, what is the most accurate interpretation of subchondral bone sclerosis's role in the disease progression?
In the context of osteoarthritis pathology, what is the most accurate interpretation of subchondral bone sclerosis's role in the disease progression?
Which of the following is the most likely sequence of pathological events, starting from the initial insult, that leads to the development of osteoarthritis?
Which of the following is the most likely sequence of pathological events, starting from the initial insult, that leads to the development of osteoarthritis?
Considering the biomechanical factors involved in osteoarthritis, which statement best explains how obesity exacerbates knee osteoarthritis?
Considering the biomechanical factors involved in osteoarthritis, which statement best explains how obesity exacerbates knee osteoarthritis?
Why might lateral MTP joint involvement be considered atypical in osteoarthritis, compared to other joints like the knee and hip?
Why might lateral MTP joint involvement be considered atypical in osteoarthritis, compared to other joints like the knee and hip?
In a patient presenting with osteoarthritis, which clinical finding would suggest a more advanced stage of the disease?
In a patient presenting with osteoarthritis, which clinical finding would suggest a more advanced stage of the disease?
Which of the following statements best captures the rationale for prioritizing joint protection strategies in the comprehensive management plan for osteoarthritis?
Which of the following statements best captures the rationale for prioritizing joint protection strategies in the comprehensive management plan for osteoarthritis?
When considering physiotherapy as an intervention for osteoarthritis, which approach would be most appropriate for improving joint stability in a patient with noticeable muscle wasting around the affected joint?
When considering physiotherapy as an intervention for osteoarthritis, which approach would be most appropriate for improving joint stability in a patient with noticeable muscle wasting around the affected joint?
While simple analgesics are often used in the initial management of osteoarthritis, what is their primary limitation in addressing the underlying pathology of the disease?
While simple analgesics are often used in the initial management of osteoarthritis, what is their primary limitation in addressing the underlying pathology of the disease?
What is the most compelling rationale for recommending weight reduction as a key management strategy for overweight or obese individuals diagnosed with osteoarthritis?
What is the most compelling rationale for recommending weight reduction as a key management strategy for overweight or obese individuals diagnosed with osteoarthritis?
What is the primary biomechanical principle behind the use of a cane in the management of hip or knee osteoarthritis?
What is the primary biomechanical principle behind the use of a cane in the management of hip or knee osteoarthritis?
In the surgical management of osteoarthritis, what is the most critical factor in determining whether a patient is a suitable candidate for osteotomy rather than arthroplasty?
In the surgical management of osteoarthritis, what is the most critical factor in determining whether a patient is a suitable candidate for osteotomy rather than arthroplasty?
Which statement offers the most insightful comparison between the roles of arthroscopic debridement and joint arthroplasty in managing osteoarthritis?
Which statement offers the most insightful comparison between the roles of arthroscopic debridement and joint arthroplasty in managing osteoarthritis?
When assessing a patient with suspected osteoarthritis of the knee, which combination of clinical findings would most strongly support the diagnosis, according to established diagnostic criteria?
When assessing a patient with suspected osteoarthritis of the knee, which combination of clinical findings would most strongly support the diagnosis, according to established diagnostic criteria?
Flashcards
Osteoarthritis Definition
Osteoarthritis Definition
Joint symptoms and signs of articular cartilage degeneration, with changes in bone and joint margin.
Primary Osteoarthritis
Primary Osteoarthritis
Affects specific joints, often related to age and unknown causes.
Secondary Osteoarthritis
Secondary Osteoarthritis
Can affect any joint, occurring at any age due to local or systemic factors.
Age-related OA Risk
Age-related OA Risk
Signup and view all the flashcards
Cartilage Pathology in OA
Cartilage Pathology in OA
Signup and view all the flashcards
Synovial Membrane Changes
Synovial Membrane Changes
Signup and view all the flashcards
Bone Changes in OA
Bone Changes in OA
Signup and view all the flashcards
Commonly Affected Joints
Commonly Affected Joints
Signup and view all the flashcards
OA in Hand Joints
OA in Hand Joints
Signup and view all the flashcards
Inactivity stiffness in OA
Inactivity stiffness in OA
Signup and view all the flashcards
X-Ray Findings in OA
X-Ray Findings in OA
Signup and view all the flashcards
Synovial Fluid Analysis in OA
Synovial Fluid Analysis in OA
Signup and view all the flashcards
Treatment Options for OA
Treatment Options for OA
Signup and view all the flashcards
Types of physiotherapy for OA
Types of physiotherapy for OA
Signup and view all the flashcards
Medications for OA
Medications for OA
Signup and view all the flashcards
Primary Osteoarthritis Joints
Primary Osteoarthritis Joints
Signup and view all the flashcards
Genetic influence in OA
Genetic influence in OA
Signup and view all the flashcards
Sex-related OA Risk
Sex-related OA Risk
Signup and view all the flashcards
Obesity and Knee OA
Obesity and Knee OA
Signup and view all the flashcards
Overload and OA
Overload and OA
Signup and view all the flashcards
Pain in OA
Pain in OA
Signup and view all the flashcards
Characteristics of OA Pain
Characteristics of OA Pain
Signup and view all the flashcards
Joint Swelling in OA
Joint Swelling in OA
Signup and view all the flashcards
Heberden's and Bouchard's Nodes
Heberden's and Bouchard's Nodes
Signup and view all the flashcards
Wasting of Muscles in OA
Wasting of Muscles in OA
Signup and view all the flashcards
Joint Deformities in OA
Joint Deformities in OA
Signup and view all the flashcards
Joint Tenderness in OA
Joint Tenderness in OA
Signup and view all the flashcards
Joint Crepitus in OA
Joint Crepitus in OA
Signup and view all the flashcards
Joint protection (OA)
Joint protection (OA)
Signup and view all the flashcards
Physiotherapy Benefits
Physiotherapy Benefits
Signup and view all the flashcards
Study Notes
Osteoarthritis Definition
- Joint symptoms and signs occur due to articular cartilage degeneration.
- These symptoms are related to changes in the underlying bone and the joint margin.
Classification
- Primary osteoarthritis affects certain joints and is related to old age.
- The cause of primary osteoarthritis is unknown.
- Secondary osteoarthritis can affect any joint at any age.
- Local mechanical factors like trauma or menisectomy can cause secondary OA.
- Joint diseases like RA or septic arthritis can cause secondary OA.
- Systemic diseases like hyperparathyroidism can cause secondary OA.
Primary Osteoarthritis Risk Factors
- Advancing age leads to a loss of glycosamino-glycan.
- This loss leaves unsupported cartilage collagen fibers.
- Genetics may be present, especially in generalized OA.
- Both sexes are affected, but generalized OA is more common in females, especially after menopause.
- Obesity predisposes individuals to knee OA.
- Repeated overload is another risk factor.
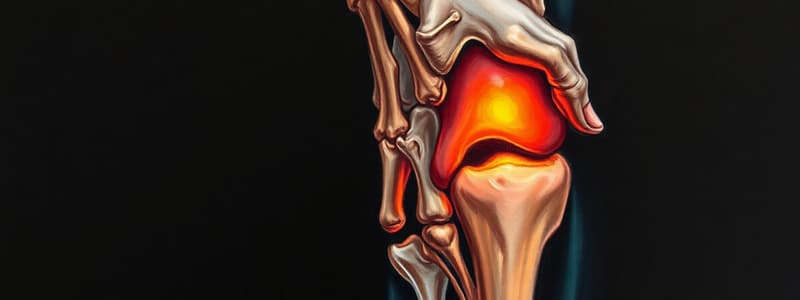
Pathology of Osteoarthritis
- Fibrillation occurs on the cartilage articular surface.
- This leads to clefts in the cartilage surface and subsequent loss of cartilage.
- Hypertrophy is observed in the synovial membrane.
- Fibrosis and contracture of the capsule occur.
- Subchondral sclerosis occurs in the bone.
- Marginal osteophytes are observed in bone changes.
Clinical Picture - Distribution of Joints
- Common joints affected include:
- Knee joint
- Lumbar and cervical vertebrae
- Hand (PIP joints/Bouchard's nodes, DIP joints/Heberden's nodes, 1st CMC joint)
- Feet (1st MTP joint)
- Hip joint.
- Rarely affected joints include:
- Ankle
- Shoulders
- Lateral MTP joints of the feet.
- Heberden's nodes are located on the distal interphalangeal joint.
- Bouchard's nodes are located on the proximal interphalangeal joint.
Symptoms of Osteoarthritis
- Pain sources include Bone, Synovium, Ligaments, Capsules and Muscle.
- Pain is worsened by exercise and weight bearing.
- The character of the pain is aching.
- Pain is poorly localized.
- As the disease progresses, pain occurs during rest.
- Inactivity stiffness is present for a few minutes.
- Morning stiffness is not a prominent feature and lasts no more than 1/4 hour.
- There is a limitation of movement and activity.
Signs of Osteoarthritis
- Swelling is due to Synovial thickening, Effusion, or Bony swelling.
- Heberden's nodes over distal interphalangeal joints
- Bouchard's nodes over proximal interphalangeal joints
- Wasting of muscles acting on the affected joints.
- Deformity:
- Flexion deformity of the knee
- Genu varum
- Genu valgum
- Joint tenderness occurs.
- Joint crepitus is coarse.
Investigations - Plain X-ray
- Plain X-ray is the most useful showing:
- Joint space narrowing
- Subchondral bone sclerosis
- Subchondral bone cysts
- Osteophytes (bone spurs)
- Central bone erosions in erosive OA
- Black arrows point to subchondral sclerosis.
- White arrows point to osteophytes.
- Black arrowheads point to joint narrowing in the medial compartment.
Investigations - Laboratory & Synovial Fluid
- Laboratory features are normal.
- Synovial fluid:
- Good viscosity
- Normal mucin clot
- Slight increase in cell count
Treatment - Joint Protection and Physiotherapy
- Instructions for joint protection to avoid overstressing the affected joints.
- Do not lie or sit too long in one position.
- Do not use low chairs.
- Do not stand in the same position or walk for long periods.
- Do not over exercise the affected joints.
- Do not use faulty postures that place stress on affected joints.
- Do not load the joint when it is very painful.
- Reduction of body weight in obese patients.
- Physiotherapy types:
- Heat
- Cold
- Electric stimulation
- Laser
- Massage
- Exercise
- Physiotherapy benefits:
- Reduce pain, stiffness, and muscle spasm
- Improve joint range of motion
- Strengthen peri-articular structures to improve joint support
- Improve blood supply and metabolism.
Treatment - Medication and Assistive Devices
- Medication:
- Use simple analgesics for pain.
- Use short courses of NSAIDS to control symptoms.
- Use chondro-protective drugs and visco-supplements.
- Assistive devices:
- Knee brace
- Stick
- Benefit: Partially unload the joint
Treatment - Surgical
- Osteotomy corrects deformity.
- Arthroplasty is a partial or total joint replacement.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.