Podcast
Questions and Answers
Within the hierarchy of blood vessel structure, which transition accurately depicts the diminishing luminal diameter observed as blood moves away from the heart?
Within the hierarchy of blood vessel structure, which transition accurately depicts the diminishing luminal diameter observed as blood moves away from the heart?
- Arteries → arterioles → capillaries → venules (correct)
- Arterioles → arteries → venules → capillaries
- Arterioles → arteries → capillaries → venules
- Arteries → arterioles → venules → capillaries
The pulmonary artery carries oxygenated blood from the lungs to the left atrium.
The pulmonary artery carries oxygenated blood from the lungs to the left atrium.
False (B)
Describe the role of the hepatic portal vein in maintaining metabolic homeostasis, and name a specific class of molecules it transports.
Describe the role of the hepatic portal vein in maintaining metabolic homeostasis, and name a specific class of molecules it transports.
The hepatic portal vein transports blood rich in nutrients and other molecules absorbed from the gastrointestinal tract directly to the liver. Examples of molecules transported by the hepatic portal vein include glucose, amino acids and lipids.
In cardiac myocytes, the influx of calcium ions into the cell during the plateau phase of the action potential is balanced primarily by the efflux of ______ ions to maintain electrical neutrality.
In cardiac myocytes, the influx of calcium ions into the cell during the plateau phase of the action potential is balanced primarily by the efflux of ______ ions to maintain electrical neutrality.
Match the following components of the cardiac conduction system with their corresponding intrinsic firing rates:
Match the following components of the cardiac conduction system with their corresponding intrinsic firing rates:
What is the functional implication of the disparity in muscle thickness between the left and right ventricles?
What is the functional implication of the disparity in muscle thickness between the left and right ventricles?
The primary function of leukocytes within the cardiovascular system is to facilitate the transport of oxygen and carbon dioxide.
The primary function of leukocytes within the cardiovascular system is to facilitate the transport of oxygen and carbon dioxide.
Describe the biophysical mechanism underlying the plateau phase observed in ventricular myocyte action potentials, explicitly detailing the ion channels involved and their temporal dynamics.
Describe the biophysical mechanism underlying the plateau phase observed in ventricular myocyte action potentials, explicitly detailing the ion channels involved and their temporal dynamics.
The Frank-Starling mechanism dictates that an increase in venous return leads to a corresponding increase in ______, thereby augmenting stroke volume.
The Frank-Starling mechanism dictates that an increase in venous return leads to a corresponding increase in ______, thereby augmenting stroke volume.
A patient presents with a stenotic aortic valve, increasing afterload on the left ventricle. Which compensatory mechanism is most likely to occur initially to maintain cardiac output?
A patient presents with a stenotic aortic valve, increasing afterload on the left ventricle. Which compensatory mechanism is most likely to occur initially to maintain cardiac output?
In parallel blood flow arrangements, alterations in the vascular resistance of one organ will invariably affect blood flow to all other organs.
In parallel blood flow arrangements, alterations in the vascular resistance of one organ will invariably affect blood flow to all other organs.
Outline the steps involved in excitation-contraction coupling in cardiac muscle cells, focusing on the roles of calcium ions, ryanodine receptors (RyR), and the sarcoplasmic reticulum.
Outline the steps involved in excitation-contraction coupling in cardiac muscle cells, focusing on the roles of calcium ions, ryanodine receptors (RyR), and the sarcoplasmic reticulum.
The AV valves are open when atrial pressure is ______ than ventricular pressure, which allows blood to flow from the atria into the ventricles.
The AV valves are open when atrial pressure is ______ than ventricular pressure, which allows blood to flow from the atria into the ventricles.
Match each numbered phase of the cardiac contractile cell action potential with its corresponding ionic event:
Match each numbered phase of the cardiac contractile cell action potential with its corresponding ionic event:
During isovolumetric ventricular relaxation, which statement accurately describes the state of the heart valves?
During isovolumetric ventricular relaxation, which statement accurately describes the state of the heart valves?
The sinoatrial (SA) node is located in the interventricular septum near the tricuspid valve.
The sinoatrial (SA) node is located in the interventricular septum near the tricuspid valve.
Explain how the unique biophysical properties of pacemaker cells, including the If 'funny' channels and T-type calcium channels, contribute to their autorhythmicity and the spontaneous generation of action potentials.
Explain how the unique biophysical properties of pacemaker cells, including the If 'funny' channels and T-type calcium channels, contribute to their autorhythmicity and the spontaneous generation of action potentials.
The QRS complex on an electrocardiogram (ECG) corresponds to the ______ of the ventricles.
The QRS complex on an electrocardiogram (ECG) corresponds to the ______ of the ventricles.
Match the following structural components of cardiac muscle cells with their respective functions:
Match the following structural components of cardiac muscle cells with their respective functions:
Under conditions of extended strenuous exercise, what adaptation best enables the heart to maintain cardiac output despite a decrease in stroke volume due to reduced filling time during diastole?
Under conditions of extended strenuous exercise, what adaptation best enables the heart to maintain cardiac output despite a decrease in stroke volume due to reduced filling time during diastole?
Flashcards
What is the heart?
What is the heart?
A muscle-driven pump for blood movement throughout the body (7,200L/day).
What is the atria/atrium?
What is the atria/atrium?
Receives blood from the vasculature.
What are the ventricles?
What are the ventricles?
Receives blood from the atria and generate force for blood to leave the heart.
What are the blood vessels?
What are the blood vessels?
Signup and view all the flashcards
What is vasculature?
What is vasculature?
Signup and view all the flashcards
What are arteries?
What are arteries?
Signup and view all the flashcards
What are veins?
What are veins?
Signup and view all the flashcards
What is blood?
What is blood?
Signup and view all the flashcards
What is Pulmonary circulation?
What is Pulmonary circulation?
Signup and view all the flashcards
What is Systemic Circulation?
What is Systemic Circulation?
Signup and view all the flashcards
What is the tricuspid valve?
What is the tricuspid valve?
Signup and view all the flashcards
What is the Bicuspid valve?
What is the Bicuspid valve?
Signup and view all the flashcards
What are the Semilunar valves?
What are the Semilunar valves?
Signup and view all the flashcards
What are Pacemaker cells?
What are Pacemaker cells?
Signup and view all the flashcards
What are Conduction fibers?
What are Conduction fibers?
Signup and view all the flashcards
What is the Sinoatrial node?
What is the Sinoatrial node?
Signup and view all the flashcards
What is the Atrioventricular node?
What is the Atrioventricular node?
Signup and view all the flashcards
What are Internodal pathway?
What are Internodal pathway?
Signup and view all the flashcards
What is Bundle of His (AV bundle)?
What is Bundle of His (AV bundle)?
Signup and view all the flashcards
What are Purkinje fibers?
What are Purkinje fibers?
Signup and view all the flashcards
Study Notes
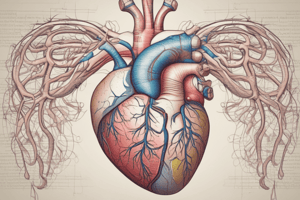
Cardiac Function Overview
- Focuses on the cardiovascular system
- Covers blood flow, heart anatomy, electrical activity, and the cardiac cycle.
Cardiovascular System Components
- The heart is a muscle pump that circulates 7,200L of blood per day
- Four chambers: atria and ventricles
- Atria receive blood from the vasculature
- Ventricles generate force to pump blood out of the heart
- The interventricular and interatrial septa divide the heart
- The septa ensures oxygenated and deoxygenated blood do not mix
Blood Vessels
- Function as conduits for blood movement
- The vasculature constitutes a system of blood vessels
- Vessels branching from the heart decrease in cross-sectional diameter
- Arteries carry blood away from the heart
- Veins carry blood to the heart
- The circulation flow is heart to arteries to arterioles to capillaries to venules to veins and back to the heart
Blood Components
- Transports cells and material to cells, and carries circulating fluid
- Includes plasma (water, dissolved proteins, ions, solutes, gases)
- Contains cells like red blood cells/erythrocytes (O2/CO2 carrier)
- Immune response driven by leukocytes and platelets are for clotting
Path of Blood Flow: Pulmonary Circulation
- Blood moves from the right ventricle to lungs, then lungs to left atrium
- Results in oxygenation and carbon dioxide removal
Path of Blood Flow: Systemic Circulation
- Blood flows from the left ventricle to tissues then returns to the right atrium
- Blood leaving the left ventricle is oxygenated via arteries
- Blood entering the right atrium is deoxygenated via the veins
- Results in oxygen delivery to tissues and carbon dioxide removal
Path of Blood Flow: Coronary Circulation
- Blood is ejected from the left ventricle via the coronary artery
- Supplies the heart surface
- Arteries branch to arterioles to deliver oxygen to the myocardium
- Deoxygenated blood returns to the right atrium via cardiac veins
- The heart removes ~70-80% of oxygen; double the amount of other cells
General Blood Flow Rule
- Blood in arteries and arterioles is oxygenated (leaving heart)
- Blood in veins and venules is deoxygenated (returning to heart)
- Blood leaving the right ventricle via the pulmonary artery is deoxygenated (exception)
- Blood entering the left atria via the pulmonary vein is oxygenated (exception)
Circulatory System Pathway
- A closed loop system
- Deoxygenated blood enters the right atrium and then the right ventricle
- From the right ventricle, blood moves to the pulmonary artery and then to the lungs
- Oxygenated blood then leaves the lungs through the pulmonary veins, and enters the left atrium
- Blood leaves the left ventricle via the aorta and takes one of three paths:
Aorta Blood Paths
- Ascending arteries goes to the arms, head, and brain (systemic circulation)
- Abdominal and descending arteries goes to the trunk, legs, internal organs (systemic)
- Coronary arteries nourishes the heart
- Moves from arteries to capillaries to cardiac veins, back to the right atrium (coronary circulation)
Pulmonary and Systemic Systems Working Together
- Systems work together in series
- Systemic organs work in parallel
- Meaning blood flows in parallel in individual systemic organs
Parallel Blood Flow Benefits
- Each organ gets fully oxygenated blood
- Blood flow is independently regulated in each organ
Exceptions to Parallel Blood Flow
- Portal vein involves two organs in series
- Blood from colon/small intestine is transported to the liver
- The hepatic portal vein transports water, ions, and nutrients from the GI tract to the liver, and then the general circulation
Heart Anatomy Location
- Situated in the chest/thoracic cavity, above the diaphragm
- Fist-sized, weighing 250-350g
- Surrounded by the pericardium (membranous sac with pericardial fluid)
- Located between the lungs
- The apex is at the bottom, resting on the diaphragm and angled down/left
- Major arteries and veins emerge from the top (base)
- Left and right chambers are separated by a septum
Heart Structure
- Ventricles = bulk of the heart
- Primarily cardiac cells
- Ventricular muscle is thicker than atrial
- Left ventricular wall is thicker, needing more pressure for the systemic system
- Blood moves by contraction (systole) and relaxation (diastole) of the myocardium
Heart Valves Overview
- Four valves maintain unidirectional blood flow
- Atrioventricular valves sit between atria/ventricles allowing flow from the atrium into the ventricle
- Valves open when atrial pressure > ventricle pressure
- Valves close when atrial pressure < ventricle pressure
- The tricuspid valve (right chambers) has three flaps (cusps)
- The bicuspid/mitral valve (left chambers) has two flaps
Semilunar Valves
- Located between the ventricles and arteries
- Open when ventricular pressure exceeds arterial pressure
- Closed when ventricular pressure is less than arterial pressure
- Aortic valve: between left ventricle and aorta
- Pulmonary valve: between right ventricle and pulmonary trunk
Cardiac Muscle Contraction
- Signals come from the cardiac cells (myogenic)
- Autorhythmic cells include pacemaker and conduction fibers
- Pacemaker cells initiates action potentials that sets the heart rhythm
- Conduction fibres, transmits/coordinate the action potential
- Electrical stimulation (action potential) in one cardiac muscle cell is transferred to an adjacent cell through gap junctions
- Intercalated disks physically link adjacent cells for mechanical stress resistance
Pacemaker Cells
- Generates action potentials spontaneously
- Sets the pace of cardiac contraction, with high concentrations in the sinoatrial (SA) node and atrioventricular (AV) node
- SA node: in the right atrium, near the superior vena cava
- AV node: in the septum between the right atrium/ventricle, near the tricuspid valve
Conduction Fibers
- These are noncontractile specialized cells
- Larger diameter for faster action potential transmission
- Transmission is ~10X faster than typical cardiac muscle cells (4m/sec versus 0.3-0.5m/sec)
- The internodal pathway connects the SA and AV nodes
- Bundle of His is in the interventricular septum
- Right and left bundles split from the AV bundle
- The Purkinje fibers network branches throughout the ventricular myocardium starting from the apex
Contraction Signals
- Electrical signals do not pass directly from the atria to the ventricles
- Signalling is transmitted only through the AV node
- Delay ensures complete atrial contraction before ventricular contraction begins
Heart Contraction Path
- The bundled of His splits into the right and left bundles and then to the purkinje fibers
- Transmitting the electrical signal only happen through the ventricles
- Purkinje fibres spreads through the mycardium and moves from the apex upwards which initiates contraction from the apex towards the valves
- Both ventricles are contracting together from apex upwards
Cardiac Cycle Overview
- Systole is contraction, and diastole is relaxation
- Lub change occur when the AV valves close
- Dub change occur when the semilunar valves close
Ventricular Volume
- This is the volume of blood in the left ventricle during the cardiac cycle
- The maximum blood volume in the left ventricle is 135ml
- After ventricular systole, ~65ml remains (~52%)
- During exercise, a larger volume can be ejected (100ml/135ml, ~70%)
Cardiac Muscle Cell Types
- Cardiac muscle (myocardium) contain two major cell types
- Contractile cells makeup majority of heart cells
- They are uninuclear, branch cell morphologies linked by gap junctions/intercalated disks, striated, contain sarcomeres
- Abundant mitochondria for aerobic metabolism
- Calcium contributes to contraction
- Are under hormonal, sympathetic, and parasympathetic control
- Conducting cells makeup 1% of heart cells
- These have special muscle cells
- Includes internodal, interatrial, SA node, AV node, Bundle of His, right/left bundles, Purkinje fibers
Pacemaker Cells Overview
- Can fire action potential without external signal
- Have spontaneous action potential (regular)
- No stable/constant resting membrane potential
- No organized sarcomeres, and are noncontractile
- Depolarize slowly until membrane reaches threshold which triggers action potential
- Cell repolarizes to -60 to -70mV
- Changes in sodium, potassium, and calcium ion movement results in action potential
- Potential becomes less negative until it reaches a threshold which is triggered by the action potential
Electrical Base
- When the membrane potential reaches -60mV, If channels ('funny' channels) open
- Na+ enters/ K+ leaves the cell. The membrane potential becomes less negative (depolarizes).
- If channels close when the membrane potential reaches -55mV
- T-type voltage-gated Ca2+ channels open and calcium enters into the cell, depolarizing the cell to the threshold potential of -40mV. T-type voltage-gated Ca2+ channels close.
- L-type voltage-gated calcium channels open and even more Ca2+ enters into the cell, depolarizing the cell.
- Voltage-gated K+ channels open and K+ leaves the cell. L-type voltage-gated Ca2+ channels close. This results in repolarization of the cell.
- Voltage-gated K+ channels close when the cell reaches -60mV
SA Node
- The action potential moves from the SA node by pacemaker cells
- This causes it to spread to surround myocardial cells with gap junctions and intercalated disks
- Also through the conduction system
- Transport through the conduction system is faster than through myocardial cells in the atria
Action Potential
- Begins at -90mV
- Depolarization moves into cardiac cells through gap junctions
- K+ channels open and K+ leaves the cell
- L-type calcium channels open
- Sodium channels become inactivated; decrease in sodium entry
- K+ leaving is counterbalanced by Ca2+ entering the cell which creates a plateau
Cardiac Muscle Contraction Control
- Action potential enters from adjacent cell.
- Voltage-gated Ca2+ channels open, and Ca2+ enters cell.
- Ca2+ induces Ca2+ release through ryanodine receptor-channels (RyR).
- Local release causes Ca2+ spark, then the summed signal is released.
- Relaxation occurs when Ca2+ unbinds from troponin, and Ca2+ is pumped back into the sarcoplasmic reticulum for storage, Ca2+ is exchanged with Na+ by the NCX antiporter
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.