Podcast
Questions and Answers
What characterizes Type I diabetes in relation to insulin production?
What characterizes Type I diabetes in relation to insulin production?
- Insulin levels remain constant throughout the patient's life.
- Insulin is produced in varying amounts.
- There is a complete or almost complete absence of insulin. (correct)
- Insulin production typically increases with age.
Which of the following complications is most commonly associated with chronic uncontrolled diabetes?
Which of the following complications is most commonly associated with chronic uncontrolled diabetes?
- Nephropathy (correct)
- Diabetic foot ulcers
- Coronary heart disease
- Retinal hemorrhages
What is a key physiological effect of chronic uncontrolled diabetes on metabolism?
What is a key physiological effect of chronic uncontrolled diabetes on metabolism?
- Decreased fat oxidation
- Preservation of protein stores
- Shifting to fat metabolism (correct)
- Increased reliance on carbohydrate metabolism
Which statement about Type II diabetes is true?
Which statement about Type II diabetes is true?
What is a common symptom of diabetic neuropathy?
What is a common symptom of diabetic neuropathy?
Which factor is a significant environmental trigger for Type I diabetes?
Which factor is a significant environmental trigger for Type I diabetes?
During diabetic ketoacidosis, which electrolyte is typically monitored due to its changes from insulin treatment?
During diabetic ketoacidosis, which electrolyte is typically monitored due to its changes from insulin treatment?
What is a primary management strategy for diabetic ketoacidosis?
What is a primary management strategy for diabetic ketoacidosis?
What is a serious complication associated with diabetic ketoacidosis (DKA)?
What is a serious complication associated with diabetic ketoacidosis (DKA)?
What distinguishes Hyperosmolar Hyperglycemic State (HHS) from diabetic ketoacidosis (DKA)?
What distinguishes Hyperosmolar Hyperglycemic State (HHS) from diabetic ketoacidosis (DKA)?
What is the recommended treatment for hyperglycemia when glucose levels exceed 13.5 mmol/l?
What is the recommended treatment for hyperglycemia when glucose levels exceed 13.5 mmol/l?
Which tissue type can utilize glucose without requiring insulin?
Which tissue type can utilize glucose without requiring insulin?
Which chronic complication of diabetes is often linked to prolonged hyperglycemia and results in impaired vision?
Which chronic complication of diabetes is often linked to prolonged hyperglycemia and results in impaired vision?
Which symptom is NOT commonly associated with diabetic ketoacidosis (DKA)?
Which symptom is NOT commonly associated with diabetic ketoacidosis (DKA)?
Which of the following symptoms indicates mild hypoglycemia?
Which of the following symptoms indicates mild hypoglycemia?
In the case of Addison's disease, what leads to the impairment of glucose metabolism?
In the case of Addison's disease, what leads to the impairment of glucose metabolism?
What treatment method is essential for managing diabetic ketoacidosis?
What treatment method is essential for managing diabetic ketoacidosis?
What plays a key role in impaired wound healing in diabetic patients?
What plays a key role in impaired wound healing in diabetic patients?
What is a common consequence when Addison’s disease is stressed?
What is a common consequence when Addison’s disease is stressed?
Which symptom is primarily characteristic of nonketotic hyperosmolar hyperglycemia?
Which symptom is primarily characteristic of nonketotic hyperosmolar hyperglycemia?
Which of the following is NOT a symptom of severe hypoglycemia?
Which of the following is NOT a symptom of severe hypoglycemia?
What is a common oral complication of uncontrolled diabetes mellitus?
What is a common oral complication of uncontrolled diabetes mellitus?
After surgery, when should a patient ideally start consuming calories orally?
After surgery, when should a patient ideally start consuming calories orally?
Which condition is indicated by high levels of cortisol that alter metabolism?
Which condition is indicated by high levels of cortisol that alter metabolism?
In which patient population is nonketotic hyperosmolar hyperglycemia most commonly seen?
In which patient population is nonketotic hyperosmolar hyperglycemia most commonly seen?
What signifies an adrenal crisis in individuals with Addison’s disease?
What signifies an adrenal crisis in individuals with Addison’s disease?
Flashcards are hidden until you start studying
Study Notes
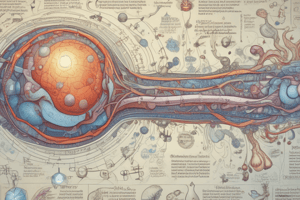
Type I Diabetes Mellitus (IDDM)
- Accounts for approximately 10% of diabetic patients, typically diagnosed in childhood or young adulthood.
- Characterized by symptoms such as polyuria, polydipsia, polyphagia, weight loss, and incontinence.
- Results from complete or almost complete lack of insulin, leading to ketoacidosis if untreated.
- Associated with a weak genetic link and autoimmune response targeting pancreatic beta cells.
- Environmental triggers include infections like congenital rubella, CMV, mumps, hepatitis, and coxsackie virus.
Type II Diabetes Mellitus (NIDDM)
- Primarily occurs in adults over the age of 40, often with slight weight fluctuations and nocturnal awakenings to urinate.
- Insulin production occurs, but ketoacidosis is rare; hyperosmolar hyperglycemic state (HHS) is more common.
- Strong genetic predisposition with factors such as increased insulin resistance and decreased receptor activity.
- Progresses to decreased insulin secretion over time, leading to excess glucagon release due to changes in alpha/beta cell ratios.
- Strongly linked to obesity.
Complications of Chronic Uncontrolled DM
- Cortisol secretion due to uncontrolled diabetes leads to protein breakdown and loss through urine.
- Body metabolizes fat, resulting in increased levels of acetoacetic acid and beta-hydroxybutyric acid, which may result in ketoacidosis.
- Failure of respiratory and renal regulators leads to acidotic states.
Chronic Complications of Type I Diabetes
- Retinopathy results in retinal hemorrhages due to hypertension.
- Neuropathy manifests as a stocking-glove distribution, causing impotence and neurogenic bladder issues.
- Nephropathy is linked to 25% of new cases of end-stage renal disease (ESRD).
- Vascular complications manifest as non-healing foot ulcers and increased risk of lower extremity amputations.
- Coronary disease primarily due to atherosclerosis and hypertension.
- Enteropathy leads to decreased gastrointestinal motility.
Micro/Macro-Angiopathy
- Ketoacidosis in Type I leads to hyperglycemia (>27), metabolic acidosis, and ketonemia.
- Type II can cause hyperosmolar hyperglycemic nonketotic coma.
- Long-term complications include diabetic retinopathy leading to blindness, cataracts, diabetic nephropathy, and renal failure.
- Accelerated atherosclerosis increases risks of coronary heart disease, stroke, and foot ulcerations.
Management of Diabetic Ketoacidosis (DKA)
- Requires aggressive IV fluid replacement with isotonic solutions, alongside insulin administration.
- Potassium monitoring is crucial since levels drop after insulin therapy.
- Bicarbonate therapy is used for severe acidosis.
- Physical examination is essential to identify underlying causes.
Symptoms of Diabetic Ketoacidosis
- Rapidly evolving symptoms over 24 hours include N/V, polyuria, altered mental status, dehydration, and Kussmaul respiration.
- A pH below 7.0 risks acidotic coma and death.
Nonketotic Hyperosmolar Hyperglycemia
- Predominantly seen in older Type II diabetes patients with high mortality rates.
- Symptoms include severe dehydration and neurological signs without anion-gap metabolic acidosis.
Oral Complications of Uncontrolled Diabetes
- Commonly results in xerostomia, poor healing, increased infections, and periodontal disease.
- Oral fungal infections and enamel hypoplasia may occur.
Infection and Wound Healing
- Hyperglycemia impairs immune response, decreasing chemotaxis and phagocytosis.
- Impaired wound healing can arise from ketoacidosis, vascular changes, and reduced blood flow.
Tissues Utilizing Glucose Independently of Insulin
- Brain, intestinal mucosa, renal cortex, lens, and red blood cells can utilize glucose without insulin.
- Muscle, fat, and liver tissues require insulin for glucose uptake.
Insulin Types and Administration
- Rapid-acting insulins cover immediate meal needs; regular insulin is used for meals consumed shortly after injection.
- Intermediate insulins cover daily needs; long-acting insulins provide coverage for an entire day.
Hypoglycemia
- Mild symptoms include hunger, pallor, weakness, sweating, and tachycardia.
- Severe cases can lead to unconsciousness, hypotension, and seizures, requiring immediate attention.
Addison's Disease
- Involves adrenal insufficiency due to cortex destruction, leading to multiple hormonal deficiencies.
- Symptoms may include nausea, dehydration, hypotension, and cardiac instability, especially during stress.
- Untreated adrenal crises can lead to severe health complications, including potential death.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.