Podcast
Questions and Answers
What is the main immunohistochemical marker used for identifying neuroendocrine tumors like carcinoid tumors?
What is the main immunohistochemical marker used for identifying neuroendocrine tumors like carcinoid tumors?
- Chromogranin (correct)
- CD56
- Ki67
- Vimentin
Which of the following clinical features is specifically associated with carcinoid syndrome?
Which of the following clinical features is specifically associated with carcinoid syndrome?
- Gastrin secretion
- Skin flushing (correct)
- Hypoglycemia
- Obstruction
What determines the grading of carcinoid tumors?
What determines the grading of carcinoid tumors?
- Size of the tumor
- Number of mitoses and Ki67 percentage (correct)
- Presence of liver metastasis
- Level of serotonin production
Which tissue response is associated with neuroendocrine tumors (carcinoid tumors) in the body?
Which tissue response is associated with neuroendocrine tumors (carcinoid tumors) in the body?
Where do most gastrointestinal stromal tumors (GISTS) primarily arise?
Where do most gastrointestinal stromal tumors (GISTS) primarily arise?
Which type of polyp is most commonly associated with an increased risk of developing gastrointestinal and non-gastrointestinal cancers?
Which type of polyp is most commonly associated with an increased risk of developing gastrointestinal and non-gastrointestinal cancers?
What is the primary characteristic of adenomatous polyps?
What is the primary characteristic of adenomatous polyps?
What is the most significant risk factor for malignant transformation of adenomatous polyps?
What is the most significant risk factor for malignant transformation of adenomatous polyps?
Which type of polyp is characterized by cystically dilated glands within an inflamed stroma?
Which type of polyp is characterized by cystically dilated glands within an inflamed stroma?
In patients with longstanding inflammatory bowel disease, which type of polyp is commonly observed?
In patients with longstanding inflammatory bowel disease, which type of polyp is commonly observed?
What differentiates sessile serrated lesions from hyperplastic polyps?
What differentiates sessile serrated lesions from hyperplastic polyps?
How are non-neoplastic polyps primarily classified?
How are non-neoplastic polyps primarily classified?
Which syndrome is associated with multiple hamartomatous polyps and an increased risk of breast and thyroid cancers?
Which syndrome is associated with multiple hamartomatous polyps and an increased risk of breast and thyroid cancers?
What is the typical clinical presentation of sessile serrated lesions?
What is the typical clinical presentation of sessile serrated lesions?
Which of the following polyps is most likely to be asymptomatic?
Which of the following polyps is most likely to be asymptomatic?
What is the primary genetic alteration linked to Familial Adenomatous Polyposis (FAP)?
What is the primary genetic alteration linked to Familial Adenomatous Polyposis (FAP)?
Which syndrome specifically includes a higher risk of brain tumors along with colorectal adenomatous polyps?
Which syndrome specifically includes a higher risk of brain tumors along with colorectal adenomatous polyps?
What is the significance of the adenoma-carcinoma sequence in colorectal cancer development?
What is the significance of the adenoma-carcinoma sequence in colorectal cancer development?
Which hereditary syndrome is characterized by a defect in mismatch DNA repair genes and primarily affects the right side of the colon?
Which hereditary syndrome is characterized by a defect in mismatch DNA repair genes and primarily affects the right side of the colon?
Which population is primarily targeted for bowel screening using the Faecal Immunochemical Test (FIT)?
Which population is primarily targeted for bowel screening using the Faecal Immunochemical Test (FIT)?
What type of lesion is most commonly associated with the development of colorectal cancer in the adenoma-carcinoma sequence?
What type of lesion is most commonly associated with the development of colorectal cancer in the adenoma-carcinoma sequence?
What specific diagnostic tool is most effective for the visual assessment and biopsy of suspected colorectal cancer?
What specific diagnostic tool is most effective for the visual assessment and biopsy of suspected colorectal cancer?
Which genetic mutation is commonly associated with resistance to anti-EGFR therapy in metastatic colon cancer treatment?
Which genetic mutation is commonly associated with resistance to anti-EGFR therapy in metastatic colon cancer treatment?
Which of the following factors is NOT considered a risk factor for colorectal carcinoma?
Which of the following factors is NOT considered a risk factor for colorectal carcinoma?
What is a characteristic clinical presentation of left-sided colorectal cancer?
What is a characteristic clinical presentation of left-sided colorectal cancer?
What type of biopsy is typically conducted to assess the adequacy of resection in colorectal cancer?
What type of biopsy is typically conducted to assess the adequacy of resection in colorectal cancer?
Which test is frequently used as a surrogate marker for monitoring colorectal cancer recurrence after treatment?
Which test is frequently used as a surrogate marker for monitoring colorectal cancer recurrence after treatment?
What is a characteristic of tumors located in the proximal colon?
What is a characteristic of tumors located in the proximal colon?
What is the most critical prognostic factor in colorectal cancer staging?
What is the most critical prognostic factor in colorectal cancer staging?
Which of the following is a non-neoplastic polyp found in the bowel?
Which of the following is a non-neoplastic polyp found in the bowel?
Which of the following tumours of the bowel is classified as a mesenchymal neoplasm?
Which of the following tumours of the bowel is classified as a mesenchymal neoplasm?
Which polyp type is considered premalignant and most likely to progress to adenocarcinoma?
Which polyp type is considered premalignant and most likely to progress to adenocarcinoma?
What is the characteristic histology of juvenile polyps?
What is the characteristic histology of juvenile polyps?
Peutz-Jeghers syndrome is associated with which of the following? (Select all that apply)
Peutz-Jeghers syndrome is associated with which of the following? (Select all that apply)
Which syndrome is associated with the PTEN gene mutation?
Which syndrome is associated with the PTEN gene mutation?
In which of the following locations are hyperplastic polyps most commonly found?
In which of the following locations are hyperplastic polyps most commonly found?
Which of the following polyps is associated with an increased risk of non-GI cancers?
Which of the following polyps is associated with an increased risk of non-GI cancers?
Which of the following is a feature of Cronkhite-Canada syndrome?
Which of the following is a feature of Cronkhite-Canada syndrome?
Which of the following is a characteristic of inflammatory polyps?
Which of the following is a characteristic of inflammatory polyps?
How does a hyperplastic polyp differ from an adenomatous polyp?
How does a hyperplastic polyp differ from an adenomatous polyp?
Which of the following distinguishes Cowden syndrome from Cronkhite-Canada syndrome?
Which of the following distinguishes Cowden syndrome from Cronkhite-Canada syndrome?
Inflammatory (pseudo) polyps differ from lymphoid polyps in that inflammatory polyps are:
Inflammatory (pseudo) polyps differ from lymphoid polyps in that inflammatory polyps are:
Peutz-Jeghers syndrome and juvenile polyposis syndrome both involve hamartomatous polyps, but Peutz-Jeghers syndrome is also associated with:
Peutz-Jeghers syndrome and juvenile polyposis syndrome both involve hamartomatous polyps, but Peutz-Jeghers syndrome is also associated with:
Which of the following is a key difference between juvenile polyps and hyperplastic polyps?
Which of the following is a key difference between juvenile polyps and hyperplastic polyps?
How does Peutz-Jeghers syndrome differ from juvenile polyposis syndrome?
How does Peutz-Jeghers syndrome differ from juvenile polyposis syndrome?
Both Peutz-Jeghers and Cowden syndromes are associated with hamartomatous polyps, but Cowden syndrome also has:
Both Peutz-Jeghers and Cowden syndromes are associated with hamartomatous polyps, but Cowden syndrome also has:
Juvenile polyps are usually seen in which age group?
Juvenile polyps are usually seen in which age group?
What is the main histological feature of a hyperplastic polyp?
What is the main histological feature of a hyperplastic polyp?
In which condition do patients have an increased risk of thyroid and breast cancer along with multiple hamartomatous polyps?
In which condition do patients have an increased risk of thyroid and breast cancer along with multiple hamartomatous polyps?
Which of the following has no malignant potential but increases the risk of other cancers such as pancreas, breast, and lung?
Which of the following has no malignant potential but increases the risk of other cancers such as pancreas, breast, and lung?
Lymphoid polyps are composed of which of the following?
Lymphoid polyps are composed of which of the following?
Which syndrome is characterized by hamartomatous polyps, nail atrophy, and skin pigmentation?
Which syndrome is characterized by hamartomatous polyps, nail atrophy, and skin pigmentation?
What is the primary risk factor for malignancy in adenomatous polyps?
What is the primary risk factor for malignancy in adenomatous polyps?
Which of the following is considered a pre-malignant polyp and a precursor to carcinoma?
Which of the following is considered a pre-malignant polyp and a precursor to carcinoma?
Which type of adenomatous polyp is most commonly pedunculated?
Which type of adenomatous polyp is most commonly pedunculated?
Which type of adenomatous polyp has the highest risk of malignant transformation?
Which type of adenomatous polyp has the highest risk of malignant transformation?
What distinguishes sessile serrated lesions from hyperplastic polyps?
What distinguishes sessile serrated lesions from hyperplastic polyps?
Adenomatous polyps with mild dysplasia typically present with which of the following symptoms?
Adenomatous polyps with mild dysplasia typically present with which of the following symptoms?
What is the treatment for adenomatous polyps?
What is the treatment for adenomatous polyps?
Which factor correlates with the risk of malignancy in adenomatous polyps?
Which factor correlates with the risk of malignancy in adenomatous polyps?
Which of the following conditions is associated with an almost 100% risk of developing colorectal carcinoma?
Which of the following conditions is associated with an almost 100% risk of developing colorectal carcinoma?
What is the minimum number of adenomatous polyps required for a diagnosis of Familial Adenomatous Polyposis (FAP)?
What is the minimum number of adenomatous polyps required for a diagnosis of Familial Adenomatous Polyposis (FAP)?
Which gene mutation is associated with Familial Adenomatous Polyposis (FAP)?
Which gene mutation is associated with Familial Adenomatous Polyposis (FAP)?
On which chromosome is the APC gene located?
On which chromosome is the APC gene located?
At what average age do patients typically begin to develop adenomatous polyps in Familial Adenomatous Polyposis (FAP)?
At what average age do patients typically begin to develop adenomatous polyps in Familial Adenomatous Polyposis (FAP)?
Which of the following is a common complication associated with Familial Adenomatous Polyposis (FAP) due to polyp formation?
Which of the following is a common complication associated with Familial Adenomatous Polyposis (FAP) due to polyp formation?
Sessile serrated lesions are commonly found in which part of the gastrointestinal tract?
Sessile serrated lesions are commonly found in which part of the gastrointestinal tract?
What histological feature is absent in sessile serrated lesions compared to adenomatous polyps?
What histological feature is absent in sessile serrated lesions compared to adenomatous polyps?
Which of the following is a characteristic feature of sessile serrated lesions?
Which of the following is a characteristic feature of sessile serrated lesions?
What gene is mutated in Gardner's syndrome?
What gene is mutated in Gardner's syndrome?
What type of inheritance pattern does Gardner's syndrome follow?
What type of inheritance pattern does Gardner's syndrome follow?
Which of the following is NOT a clinical feature of Gardner's syndrome?
Which of the following is NOT a clinical feature of Gardner's syndrome?
Patients with Gardner's syndrome have an increased risk of which type of cancer?
Patients with Gardner's syndrome have an increased risk of which type of cancer?
What type of tumors are primarily associated with Turcot's syndrome?
What type of tumors are primarily associated with Turcot's syndrome?
What is the genetic cause of Turcot's syndrome?
What is the genetic cause of Turcot's syndrome?
Which of the following brain tumors is commonly associated with Turcot's syndrome?
Which of the following brain tumors is commonly associated with Turcot's syndrome?
What is the adenoma-carcinoma sequence?
What is the adenoma-carcinoma sequence?
Which statement about adenomatous polyps is true?
Which statement about adenomatous polyps is true?
What type of mutation is primarily associated with familial adenomatous polyposis (FAP)?
What type of mutation is primarily associated with familial adenomatous polyposis (FAP)?
Which of the following mutations leads to the activation of K-ras in the adenoma-carcinoma sequence?
Which of the following mutations leads to the activation of K-ras in the adenoma-carcinoma sequence?
What is the consequence of losing the DCC gene (located on chromosome 18q) in the adenoma-carcinoma sequence?
What is the consequence of losing the DCC gene (located on chromosome 18q) in the adenoma-carcinoma sequence?
Which gene is associated with the loss of cell cycle regulation and is often mutated in colorectal cancer?
Which gene is associated with the loss of cell cycle regulation and is often mutated in colorectal cancer?
Which of the following is true regarding the activation of telomerase in the adenoma-carcinoma sequence?
Which of the following is true regarding the activation of telomerase in the adenoma-carcinoma sequence?
Which chromosome is the K-ras gene located on? A) 5q B) 12p C) 17p D) 18q
Which chromosome is the K-ras gene located on? A) 5q B) 12p C) 17p D) 18q
The loss of which gene is associated with further progression from adenomatous polyps to colorectal carcinoma?
The loss of which gene is associated with further progression from adenomatous polyps to colorectal carcinoma?
Which mutation typically occurs in the later stages of the adenoma-carcinoma sequence, often associated with invasive carcinoma?
Which mutation typically occurs in the later stages of the adenoma-carcinoma sequence, often associated with invasive carcinoma?
Which of the following statements is true regarding the adenoma-carcinoma sequence?
Which of the following statements is true regarding the adenoma-carcinoma sequence?
What is the target population for bowel screening using the Faecal Immunochemical Test (FIT)?
What is the target population for bowel screening using the Faecal Immunochemical Test (FIT)?
How often are individuals in the target population offered bowel screening?
How often are individuals in the target population offered bowel screening?
What is the main aim of bowel screening programs?
What is the main aim of bowel screening programs?
What type of cancer is colon adenocarcinoma primarily associated with?
What type of cancer is colon adenocarcinoma primarily associated with?
Which of the following is a significant risk factor for colon adenocarcinoma?
Which of the following is a significant risk factor for colon adenocarcinoma?
Which hereditary syndrome is characterized by numerous adenomatous polyps throughout the gastrointestinal tract?
Which hereditary syndrome is characterized by numerous adenomatous polyps throughout the gastrointestinal tract?
Which condition is most commonly associated with an increased risk of colon adenocarcinoma?
Which condition is most commonly associated with an increased risk of colon adenocarcinoma?
What is the 'multi-hit' hypothesis in the context of colon adenocarcinoma?
What is the 'multi-hit' hypothesis in the context of colon adenocarcinoma?
Which genetic syndrome is primarily associated with germline mutations of the APC gene?
Which genetic syndrome is primarily associated with germline mutations of the APC gene?
In the adenoma-carcinoma sequence, which mutation typically occurs first?
In the adenoma-carcinoma sequence, which mutation typically occurs first?
Which of the following pathways is associated with microsatellite instability?
Which of the following pathways is associated with microsatellite instability?
What type of genetic alteration is primarily observed in hereditary nonpolyposis colorectal cancer (HNPCC)?
What type of genetic alteration is primarily observed in hereditary nonpolyposis colorectal cancer (HNPCC)?
Which of the following best describes the relationship between adenomatous polyps and colon cancer in the adenoma-carcinoma sequence?
Which of the following best describes the relationship between adenomatous polyps and colon cancer in the adenoma-carcinoma sequence?
What type of inheritance pattern does Lynch syndrome (HNPCC) follow?
What type of inheritance pattern does Lynch syndrome (HNPCC) follow?
Which of the following is a key characteristic of colon cancer associated with Lynch syndrome?
Which of the following is a key characteristic of colon cancer associated with Lynch syndrome?
In Lynch syndrome type 1, what is the main associated cancer?
In Lynch syndrome type 1, what is the main associated cancer?
In Lynch syndrome type 2, which cancers have an increased risk along with colorectal cancer?
In Lynch syndrome type 2, which cancers have an increased risk along with colorectal cancer?
Which of the following genes is associated with Lynch syndrome?
Which of the following genes is associated with Lynch syndrome?
Patients with Lynch syndrome typically have:
Patients with Lynch syndrome typically have:
Which of the following statements regarding Lynch syndrome is true?
Which of the following statements regarding Lynch syndrome is true?
A mutation in which of the following genes is most frequently associated with Lynch Syndrome?
A mutation in which of the following genes is most frequently associated with Lynch Syndrome?
Which of the following genes is part of the mismatch repair system and has an important role in Lynch Syndrome?
Which of the following genes is part of the mismatch repair system and has an important role in Lynch Syndrome?
Which of the following describes the typical growth pattern of tumors in the proximal colon?
Which of the following describes the typical growth pattern of tumors in the proximal colon?
What is a common clinical presentation associated with tumors in the proximal colon?
What is a common clinical presentation associated with tumors in the proximal colon?
Which of the following statements is true regarding colorectal carcinoma in adults, especially males?
Which of the following statements is true regarding colorectal carcinoma in adults, especially males?
In the distal colon, tumors tend to present as:
In the distal colon, tumors tend to present as:
What type of anemia is particularly associated with colorectal carcinoma in adults?
What type of anemia is particularly associated with colorectal carcinoma in adults?
Why do tumors of the left side of the colon often present with obstruction?
Why do tumors of the left side of the colon often present with obstruction?
Which of the following is NOT a common symptom of colorectal cancer?
Which of the following is NOT a common symptom of colorectal cancer?
Which symptom is typically associated with left-sided colorectal carcinoma?
Which symptom is typically associated with left-sided colorectal carcinoma?
Right-sided colorectal carcinoma is commonly associated with which of the following symptoms?
Right-sided colorectal carcinoma is commonly associated with which of the following symptoms?
Which of the following is a noted complication associated with colonic carcinoma?
Which of the following is a noted complication associated with colonic carcinoma?
What symptom might indicate a potential obstruction in left-sided colorectal cancer?
What symptom might indicate a potential obstruction in left-sided colorectal cancer?
Which of the following is a common symptom of left-sided colorectal carcinoma?
Which of the following is a common symptom of left-sided colorectal carcinoma?
What are the microscopic features of colorectal carcinoma?
What are the microscopic features of colorectal carcinoma?
Which of the following diagnostic methods is commonly used for colorectal carcinoma?
Which of the following diagnostic methods is commonly used for colorectal carcinoma?
Which tumor marker is used in the management of colorectal cancer?
Which tumor marker is used in the management of colorectal cancer?
What does a low sensitivity and specificity of the CEA marker indicate?
What does a low sensitivity and specificity of the CEA marker indicate?
Which of the following factors is associated with a poorer prognosis in colorectal carcinoma?
Which of the following factors is associated with a poorer prognosis in colorectal carcinoma?
What is a common site for metastasis in colorectal carcinoma?
What is a common site for metastasis in colorectal carcinoma?
What factors can influence the prognosis of colorectal cancer?
What factors can influence the prognosis of colorectal cancer?
Which microscopic feature is commonly associated with colorectal carcinoma?
Which microscopic feature is commonly associated with colorectal carcinoma?
What does it indicate when colorectal carcinoma invades through the bowel wall?
What does it indicate when colorectal carcinoma invades through the bowel wall?
What is the primary purpose of measuring carcinoembryonic antigen (CEA) levels in colorectal cancer patients?
What is the primary purpose of measuring carcinoembryonic antigen (CEA) levels in colorectal cancer patients?
What is a notable limitation of the CEA tumor marker?
What is a notable limitation of the CEA tumor marker?
Which imaging technique is commonly used for staging colorectal cancer?
Which imaging technique is commonly used for staging colorectal cancer?
What does the 'T' in the TNM staging system for colorectal carcinoma primarily assess?
What does the 'T' in the TNM staging system for colorectal carcinoma primarily assess?
Which of the following is NOT included in the TNM classification for colorectal cancer?
Which of the following is NOT included in the TNM classification for colorectal cancer?
What is the most common site for distant metastasis in colorectal carcinoma?
What is the most common site for distant metastasis in colorectal carcinoma?
Which of the following tests is used to assess mismatch repair proteins in colorectal cancer?
Which of the following tests is used to assess mismatch repair proteins in colorectal cancer?
What is the purpose of BRAF testing in colorectal carcinoma?
What is the purpose of BRAF testing in colorectal carcinoma?
Which monoclonal antibody works by blocking the EGFR signaling pathway in metastatic colon cancer?
Which monoclonal antibody works by blocking the EGFR signaling pathway in metastatic colon cancer?
What type of tumors do neuroendocrine tumors (carcinoids) primarily arise from?
What type of tumors do neuroendocrine tumors (carcinoids) primarily arise from?
Which of the following is a common site for carcinoid tumors?
Which of the following is a common site for carcinoid tumors?
What is a characteristic feature of carcinoid tumors when examined histologically?
What is a characteristic feature of carcinoid tumors when examined histologically?
Which immunohistochemical marker is NOT associated with carcinoid tumors?
Which immunohistochemical marker is NOT associated with carcinoid tumors?
What is the primary purpose of performing immunohistochemistry in colorectal cancer?
A) To assess tumor staging
B) To detect mismatch repair protein deficiencies
C) To identify distant metastasis
D) To measure tumor grade
What is the primary purpose of performing immunohistochemistry in colorectal cancer? A) To assess tumor staging B) To detect mismatch repair protein deficiencies C) To identify distant metastasis D) To measure tumor grade
Which of the following mismatch repair proteins are commonly tested for using immunohistochemistry in colorectal cancer?
Which of the following mismatch repair proteins are commonly tested for using immunohistochemistry in colorectal cancer?
Microsatellite instability (MSI) in colorectal cancer is commonly detected using which method?
Microsatellite instability (MSI) in colorectal cancer is commonly detected using which method?
BRAF mutation testing is particularly important in colorectal cancer when:
BRAF mutation testing is particularly important in colorectal cancer when:
MLH1 promoter methylation is specifically tested when:
MLH1 promoter methylation is specifically tested when:
Microsatellite instability (MSI) in colorectal cancer is commonly detected using which method?
Microsatellite instability (MSI) in colorectal cancer is commonly detected using which method?
BRAF mutation testing is particularly important in colorectal cancer when:
BRAF mutation testing is particularly important in colorectal cancer when:
MLH1 promoter methylation is specifically tested when:
MLH1 promoter methylation is specifically tested when:
Which of the following monoclonal antibodies is used to block the EGFR signaling pathway in metastatic colon cancer?
Which of the following monoclonal antibodies is used to block the EGFR signaling pathway in metastatic colon cancer?
Panitumumab and cetuximab are effective in treating metastatic colon cancer by inhibiting which signaling pathway?
Panitumumab and cetuximab are effective in treating metastatic colon cancer by inhibiting which signaling pathway?
Which of the following mutations is associated with resistance to anti-EGFR therapy in metastatic colon cancer?
Which of the following mutations is associated with resistance to anti-EGFR therapy in metastatic colon cancer?
The effectiveness of anti-EGFR monoclonal antibodies such as cetuximab and panitumumab depends on the mutation status of which of the following genes?
The effectiveness of anti-EGFR monoclonal antibodies such as cetuximab and panitumumab depends on the mutation status of which of the following genes?
Which monoclonal antibody is used to block the growth of blood vessels in metastatic colon cancer by inhibiting VEGF?
Which monoclonal antibody is used to block the growth of blood vessels in metastatic colon cancer by inhibiting VEGF?
Which mechanism of action is associated with the drug bevacizumab in metastatic colon cancer treatment?
Which mechanism of action is associated with the drug bevacizumab in metastatic colon cancer treatment?
In patients with metastatic colon cancer, mutations in which gene predict resistance to treatment with cetuximab and panitumumab?
In patients with metastatic colon cancer, mutations in which gene predict resistance to treatment with cetuximab and panitumumab?
Cetuximab and panitumumab are NOT effective in patients with metastatic colon cancer who have mutations in which of the following genes?
Cetuximab and panitumumab are NOT effective in patients with metastatic colon cancer who have mutations in which of the following genes?
Which of the following monoclonal antibodies is specifically designed to inhibit VEGF and block angiogenesis in metastatic colon cancer?
Which of the following monoclonal antibodies is specifically designed to inhibit VEGF and block angiogenesis in metastatic colon cancer?
Which of the following is TRUE about the use of monoclonal antibodies in colorectal cancer treatment?
Which of the following is TRUE about the use of monoclonal antibodies in colorectal cancer treatment?
Which of the following is the most common site for neuroendocrine (carcinoid) tumors in the gastrointestinal tract?
Which of the following is the most common site for neuroendocrine (carcinoid) tumors in the gastrointestinal tract?
Carcinoid syndrome is most likely to occur when neuroendocrine tumors have metastasized to which of the following organs?
Carcinoid syndrome is most likely to occur when neuroendocrine tumors have metastasized to which of the following organs?
Which of the following hormones is most commonly secreted by neuroendocrine (carcinoid) tumors?
Which of the following hormones is most commonly secreted by neuroendocrine (carcinoid) tumors?
What is the histological feature commonly observed in neuroendocrine (carcinoid) tumors?
What is the histological feature commonly observed in neuroendocrine (carcinoid) tumors?
Which of the following immunohistochemical markers is most commonly positive in neuroendocrine (carcinoid) tumors?
Which of the following immunohistochemical markers is most commonly positive in neuroendocrine (carcinoid) tumors?
Which of the following is a common symptom of carcinoid syndrome?
Which of the following is a common symptom of carcinoid syndrome?
Carcinoid syndrome is associated with elevated levels of which substance in the urine?
Carcinoid syndrome is associated with elevated levels of which substance in the urine?
Which clinical feature is NOT typically associated with carcinoid syndrome?
Which clinical feature is NOT typically associated with carcinoid syndrome?
What pathological feature is commonly seen in neuroendocrine (carcinoid) tumors?
What pathological feature is commonly seen in neuroendocrine (carcinoid) tumors?
Which of the following is TRUE regarding the grading of neuroendocrine (carcinoid) tumors?
Which of the following is TRUE regarding the grading of neuroendocrine (carcinoid) tumors?
Which of the following is TRUE regarding the grading of neuroendocrine (carcinoid) tumors?
Which of the following is TRUE regarding the grading of neuroendocrine (carcinoid) tumors?
Which of the following conditions can be caused by neuroendocrine tumors releasing excessive gastrin?
Which of the following conditions can be caused by neuroendocrine tumors releasing excessive gastrin?
Which of the following triggers symptoms of carcinoid syndrome?
Which of the following triggers symptoms of carcinoid syndrome?
Which of the following growth patterns is NOT typically seen in neuroendocrine (carcinoid) tumors?
Which of the following growth patterns is NOT typically seen in neuroendocrine (carcinoid) tumors?
What is the significance of the dense-core granules seen in neuroendocrine tumors?
What is the significance of the dense-core granules seen in neuroendocrine tumors?
Which of the following is a common microscopic reaction seen in response to neuroendocrine (carcinoid) tumors?
Which of the following is a common microscopic reaction seen in response to neuroendocrine (carcinoid) tumors?
Which staining technique is commonly used to identify neuroendocrine (carcinoid) tumors?
Which staining technique is commonly used to identify neuroendocrine (carcinoid) tumors?
Which of the following is the most common site for neuroendocrine (carcinoid) tumors in the gastrointestinal (GI) tract?
Which of the following is the most common site for neuroendocrine (carcinoid) tumors in the gastrointestinal (GI) tract?
Neuroendocrine (carcinoid) tumors are associated with the secretion of which bioactive hormone, particularly contributing to carcinoid syndrome?
Neuroendocrine (carcinoid) tumors are associated with the secretion of which bioactive hormone, particularly contributing to carcinoid syndrome?
What is a key factor that correlates with the behavior and malignancy potential of neuroendocrine (carcinoid) tumors?
What is a key factor that correlates with the behavior and malignancy potential of neuroendocrine (carcinoid) tumors?
Which of the following best describes the malignant potential of neuroendocrine (carcinoid) tumors?
Which of the following best describes the malignant potential of neuroendocrine (carcinoid) tumors?
Which of the following GI sites has the least likelihood of developing neuroendocrine (carcinoid) tumors?
Which of the following GI sites has the least likelihood of developing neuroendocrine (carcinoid) tumors?
Which of the following is a requirement for the development of carcinoid syndrome in gastrointestinal (GI) carcinoid tumors?
Which of the following is a requirement for the development of carcinoid syndrome in gastrointestinal (GI) carcinoid tumors?
Carcinoid syndrome is characterized by the excess elaboration of which substance?
Carcinoid syndrome is characterized by the excess elaboration of which substance?
Which of the following is NOT a symptom of carcinoid syndrome?
Which of the following is NOT a symptom of carcinoid syndrome?
Carcinoid syndrome leads to systemic fibrosis, particularly affecting which cardiac structures?
Carcinoid syndrome leads to systemic fibrosis, particularly affecting which cardiac structures?
Which of the following can trigger the symptoms of carcinoid syndrome?
Which of the following can trigger the symptoms of carcinoid syndrome?
In carcinoid syndrome, where is serotonin primarily degraded, preventing the syndrome from developing in the absence of liver metastasis?
In carcinoid syndrome, where is serotonin primarily degraded, preventing the syndrome from developing in the absence of liver metastasis?
A patient with carcinoid syndrome presents with hepatomegaly. What is the most likely cause of the enlarged liver?
A patient with carcinoid syndrome presents with hepatomegaly. What is the most likely cause of the enlarged liver?
Gastrointestinal stromal tumors (GISTs) arise from which type of cells in the gastrointestinal tract?
Gastrointestinal stromal tumors (GISTs) arise from which type of cells in the gastrointestinal tract?
Which of the following genetic mutations is commonly associated with gastrointestinal stromal tumors (GISTs)?
Which of the following genetic mutations is commonly associated with gastrointestinal stromal tumors (GISTs)?
What is the first-line targeted therapy for gastrointestinal stromal tumors (GISTs) with c-kit or PDGFRA mutations?
What is the first-line targeted therapy for gastrointestinal stromal tumors (GISTs) with c-kit or PDGFRA mutations?
Which of the following immunohistochemistry markers is positive in gastrointestinal stromal tumors (GISTs)?
Which of the following immunohistochemistry markers is positive in gastrointestinal stromal tumors (GISTs)?
Which of the following is a risk factor for B-cell gastric lymphoma (MALTOMA)?
Which of the following is a risk factor for B-cell gastric lymphoma (MALTOMA)?
In the context of gastrointestinal lymphoma, what is the immunohistochemistry marker commonly associated with B-cell lymphoma?
In the context of gastrointestinal lymphoma, what is the immunohistochemistry marker commonly associated with B-cell lymphoma?
Coeliac disease is a known risk factor for which type of gastrointestinal lymphoma?
Coeliac disease is a known risk factor for which type of gastrointestinal lymphoma?
Which of the following secondary tumors can metastasize to the gastrointestinal tract? (Select all that apply)
Which of the following secondary tumors can metastasize to the gastrointestinal tract? (Select all that apply)
Which of the following features is used to classify gastrointestinal stromal tumors (GISTs) as benign or malignant?
Which of the following features is used to classify gastrointestinal stromal tumors (GISTs) as benign or malignant?
Which of the following is NOT commonly a location for gastrointestinal stromal tumors (GISTs)?
Which of the following is NOT commonly a location for gastrointestinal stromal tumors (GISTs)?
Gastrointestinal lymphoma associated with coeliac disease primarily involves which part of the bowel?
Gastrointestinal lymphoma associated with coeliac disease primarily involves which part of the bowel?
Which of the following is true regarding mesenchymal tumors of the gastrointestinal tract?
Which of the following is true regarding mesenchymal tumors of the gastrointestinal tract?
Which of the following immunohistochemistry markers would confirm a diagnosis of lymphoma?
Which of the following immunohistochemistry markers would confirm a diagnosis of lymphoma?
Which type of gastrointestinal lymphoma is most commonly associated with Helicobacter pylori infection?
Which type of gastrointestinal lymphoma is most commonly associated with Helicobacter pylori infection?
What is the most common primary extranodal site for lymphoma?
What is the most common primary extranodal site for lymphoma?
Immunohistochemistry for gastrointestinal lymphomas shows CD3 positivity. Which type of lymphoma does this indicate?
Immunohistochemistry for gastrointestinal lymphomas shows CD3 positivity. Which type of lymphoma does this indicate?
Which of the following is a monoclonal antibody that targets vascular endothelial growth factor (VEGF) to inhibit angiogenesis in metastatic colon cancer?
Which of the following is a monoclonal antibody that targets vascular endothelial growth factor (VEGF) to inhibit angiogenesis in metastatic colon cancer?
What is the key role of KRAS, BRAF, and NRAS mutation testing in metastatic colon cancer treatment?
What is the key role of KRAS, BRAF, and NRAS mutation testing in metastatic colon cancer treatment?
Which of the following is NOT a common secondary tumor that metastasizes to the gastrointestinal tract?
Which of the following is NOT a common secondary tumor that metastasizes to the gastrointestinal tract?
Which of the following markers is most commonly associated with B-cell lymphomas?
Which of the following markers is most commonly associated with B-cell lymphomas?
CD3 is a specific marker for which type of lymphoma?
CD3 is a specific marker for which type of lymphoma?
CD79 is a marker for which type of lymphocytes?
CD79 is a marker for which type of lymphocytes?
Which of the following immunohistochemical markers distinguishes B-cell lymphoma from T-cell lymphoma?
Which of the following immunohistochemical markers distinguishes B-cell lymphoma from T-cell lymphoma?
Which of the following mutations is commonly associated with Gastrointestinal Stromal Tumors (GISTs)?
Which of the following mutations is commonly associated with Gastrointestinal Stromal Tumors (GISTs)?
Which of the following drugs is used to inhibit tyrosine kinase activity in GIST patients with c-kit or PDGFRA mutations?
Which of the following drugs is used to inhibit tyrosine kinase activity in GIST patients with c-kit or PDGFRA mutations?
Which of the following immunohistochemistry markers is commonly positive in Gastrointestinal Stromal Tumors (GISTs)?
Which of the following immunohistochemistry markers is commonly positive in Gastrointestinal Stromal Tumors (GISTs)?
DOG1 is a diagnostic marker for which type of tumor?
DOG1 is a diagnostic marker for which type of tumor?
Which of the following mutations is often associated with resistance to Gleevec (imatinib) in GIST treatment?
Which of the following mutations is often associated with resistance to Gleevec (imatinib) in GIST treatment?
What is the function of the drug Gleevec (imatinib) in the treatment of GISTs?
What is the function of the drug Gleevec (imatinib) in the treatment of GISTs?
Which two mutations are commonly implicated in the pathogenesis of GISTs?
Which two mutations are commonly implicated in the pathogenesis of GISTs?
Which gene mutation is most commonly associated with Gastrointestinal Stromal Tumors (GISTs)?
Which gene mutation is most commonly associated with Gastrointestinal Stromal Tumors (GISTs)?
Which immunohistochemical marker is used for diagnosing GISTs?
Which immunohistochemical marker is used for diagnosing GISTs?
Flashcards are hidden until you start studying
Study Notes
Tumours of Small & Large Bowel
- Tumours of the large bowel are more common than tumours of the small bowel.
- Primary tumours include non-neoplastic polyps, epithelial neoplasms, mesenchymal neoplasms and lymphoma.
- Secondary tumours are rare.
Polyps
- Polyps are masses arising from the mucosal epithelium or from the submucosal connective tissue protruding into the lumen of the gut.
- Polyps can be non-neoplastic or neoplastic (adenomas).
- Polyps can be pedunculated (with a stalk) or sessile (flat).
Non-Neoplastic Polyps
- Non-neoplastic polyps include hyperplastic polyps, hamartomatous polyps (juvenile, Peutz-Jeghers), inflammatory polyps and lymphoid polyps.
Hyperplastic Polyps
- Common lesions, found in over 50% of people over 60 years.
- Often found in the recto-sigmoid.
- Less than 5 mm in size.
- Can be single or multiple.
- Usually asymptomatic.
- Composed of non-neoplastic glands, with goblet cell differentiation and serrated appearance.
- Result from delayed shedding of surface epithelial cells.
- Virtually no malignant potential.
Juvenile Polyps
- Hamartomatous malformations of bowel mucosa.
- Common in children under 5 years but can be found in adults.
- Usually located in the rectum.
- Can be large (1-3 cm).
- Contain cystically dilated glands in an inflamed stroma.
- No malignant potential.
- Juvenile polyposis is characterized by multiple juvenile polyps and adenomas.
Peutz-Jeghers Polyps
- Hamartomatous polyps of the small intestine and colon.
- Can be single or multiple (Peutz-Jeghers syndrome).
- Characterized by mucocutaneous pigmentation (around lips, oral mucosa, genitalia and palmar surfaces of the hand).
- Multiple hamartomatous polyps throughout the gastrointestinal tract.
- No malignant potential.
- Increased risk of developing GI and non-GI cancers (pancreas, breast, lung, ovary and uterus).
- Autosomal dominant syndrome.
- Comprise glands and connective tissue with smooth muscle.
Hamartomatous Syndromes
- Cowden syndrome: Autosomal dominant syndrome (PTEN). Characterized by multiple hamartomatous polyps, trichoepitheliomas and increased risk of thyroid and breast cancer.
- Cronkhite-Canada syndrome: Characterized by hamartomatous polyps, nail atrophy, skin pigmentation and increased risk of GI cancers.
Inflammatory and Lymphoid Polyps
- Inflammatory (pseudo) polyps: Inflamed regenerative mucosa surrounded by ulcerated tissue, seen in patients with long-standing inflammatory bowel disease.
- Lymphoid polyps: Intramucosal lymphoid tissue.
Adenomatous Polyps = Neoplastic Polyps
- Common lesions (prevalence 50% at age of 60).
- Proliferation of dysplastic epithelium (ranging from mild to severe).
- Precursors of carcinoma.
- Benign but may progress to adenocarcinoma via the adenoma-carcinoma sequence.
Adenomatous Polyps
- Three types: tubular, villous and tubulovillous.
- Can be pedunculated or sessile.
- All adenomatous polyps are covered by dysplastic epithelium.
- Risk of malignancy correlates with size (>2cm), histologic type (villous component) and degree of dysplasia.
- All adenomatous polyps should be removed.
- May be asymptomatic.
- May present with occult bleeding, anaemia, protein loss and obstruction.
- Treatment involves complete excision.
Sessile Serrated Lesions
- Overlap with hyperplastic polyps, but have serrated architecture in the crypt base.
- Lack cytologic features of dysplasia.
- Found in the right colon.
- May be asymptomatic.
- May present with occult bleeding, anaemia, protein loss and obstruction.
- Treatment involves complete excision.
Familial Adenomatous Polyposis (FAP)
- Autosomal dominant inheritance.
- Mutations of APC gene on 5q21.
- Numerous adenomatous polyps throughout the gastrointestinal tract, especially in the large bowel (minimum 100, may be >2000).
- Average age of onset of polyps is teens to twenties, presenting with bleeding and anaemia.
- Virtually 100% risk of carcinoma within 10 to 15 years.
- Indication for prophylactic total colectomy.
Gardner’s Syndrome
- A variation of FAP.
- Mutations of APC gene.
- Autosomal dominant.
- Characterized by multiple adenomas, epidermoid cysts (skin), fibromatosis (soft tissue), osteomas (bone) and abnormal dentition (teeth).
- Increased risk of duodenal cancer and thyroid cancer.
Turcot’s Syndrome
- A variation of FAP.
- Mutations of APC gene.
- Autosomal dominant.
- Characterized by colorectal adenomatous polyps and brain tumours (gliomas, medulloblastoma).
Adenoma-Carcinoma Sequence
- Describes the development of carcinoma from adenomatous lesions.
- Populations with a high prevalence of adenomas also have a high prevalence of colorectal cancer.
- Distribution of adenomas is comparable to that of colorectal cancer.
- Peak incidence of adenomatous polyps precedes the peak for cancer by some years.
- Risk of cancer is related to the number of adenomas.
- Adenomatous lesions are often seen in association with invasive carcinoma.
- Involves APC mutations (FAP-germline, Adenoma-sporadic), inactivation/mutation of other allele of APC, activation of K-ras (12p), loss of DCC gene (18q), loss of p53 (17p), increase expression of COX and activation of telomerase.
Bowel Screen
- Target population: 59 to 69 years.
- Screened every 2 years.
- Screening conducted using a home testing kit (Faecal Immunochemical Test- FIT).
- Polyps are usually clinically silent, but can bleed.
- Aim is to remove adenomatous polyps before progression to carcinoma (colonoscopy).
- All polyps are removed and examined microscopically.
Colon Adenocarcinoma
- Disease of the Western world.
- Peak incidence is in the seventh decade.
- Carcinoma in a young person is associated with genetic predisposition or ulcerative colitis.
Risk Factors for Colon Carcinoma
- Increasing age
- Adenomatous polyps
- Hereditary syndromes
- Inflammatory bowel disease (especially ulcerative colitis)
- Diet (low fibre, high fat, high carbohydrates, high intake of red meat and decreased intake of micronutrients, vitamins A,C & E)
- Obesity
- Physical inactivity
Hereditary Colon Cancer Syndromes
- Familial adenomatous polyposis
- Hereditary nonpolyposis colorectal cancer (HNPCC)
Colon Adenocarcinoma-Cumulative Genetic Alterations or “Multi-Hit” Hypothesis
- Two pathways:
- Adenoma-carcinoma sequence: APC mutations (FAP-germline, Adenoma-sporadic).
- Microsatellite instability (HNPCC, serrated lesions).
Lynch Syndrome
- HNPCC (Lynch syndrome).
- Autosomal dominant familial syndrome.
- Colonic cancer is not associated with pre-existing adenomas and is usually right-sided.
- Lower number of polyps than FAP.
- Defect in the mismatch DNA repair genes (MSH2, MLH1, MLH6, PMS1, MPS2).
- Lynch syndrome 1: Increased risk of colon cancer.
- Lynch syndrome 2: Increased risk of colon cancer and non-GI cancers (endometrial, ovarian).
Colorectal Carcinoma
- Tumours in the proximal colon tend to grow as polypoid lesions ("cauliflower"), may ulcerate resulting in occult bleeding.
- Iron deficiency anaemia in an adult (especially a male) should be considered colon cancer until proven otherwise.
- In the distal colon, tumours tend to be annular, encircling lesions ("napkin-ring") causing constriction with symptoms and signs of obstruction (rectal bleeding and changing bowel habits).
Why Do Tumours of the Left Side Present with Obstruction?
- Annular tumours.
- Lumen is narrower than the right side.
- Solid faecal material.
Symptoms of Colorectal Cancer
-
Change in bowel habits.
-
Blood in stool.
-
Iron deficiency anaemia.
-
Abdominal discomfort/pain.
-
Colonic carcinoma is associated with an increased risk of Streptococcus bovis endocarditis.
Clinical Presentation of Colorectal Cancer
- Left-sided carcinoma: Decreased stool calibre, left lower quadrant pain, blood-streaked stool.
- Right-sided carcinoma: Iron deficiency anaemia and vague pain.
Microscopic Features of Colorectal Carcinoma
- Adenocarcinoma: Well, moderately or poorly differentiated.
- May produce mucin.
- Invade through the bowel wall.
- Metastasise to lymph nodes and then to liver and lungs.
Diagnosis of Colorectal Carcinoma
- Colonoscopy and biopsy.
- Barium enema.
- Occult blood.
- Digital rectal examination.
- CEA (carcinoembryonic antigen- tumour marker).
- Low sensitivity and specificity.
- Used to assess the adequacy of resection and detect early recurrence.
- Radiology-staging.
Prognosis of Colorectal Carcinoma
- Stage of the tumour.
- Tumour grade (degree of differentiation).
- Tumour location:
- Left sided lesions have a poorer prognosis because they tend to be more invasive.
- Adequacy of excision (margins).
- Genetic mutations and MSI.
Staging- Most Important Prognostic Factor-TNM
- T: Depth of invasion; tumours limited to the mucosa generally do not spread due to a lack of lymphatics in the mucosa.
- N: Spread to regional nodes.
- M: Distant spread; most commonly involves the liver.
Ancillary Tests
- Immunohistochemistry for mismatch repair proteins (MSH2, MLH1, PMS1, MPS2).
- MSI by PCR.
- Gene mutation testing: KRAS, NRAS, BRAF.
- BRAF testing (if IHC deficient or MSI-High).
- MLH1 promoter methylation (if MSI high or deficient MLH1).
Monoclonal Antibodies Approved to Treat Metastatic Colon Cancer
- Erbitux® (cetuximab) and Vectibix® (panitumumab): Block the EGFR signalling pathway.
- Effectiveness of EGFR inhibition depends on downstream mutations.
- KRAS, BRAF, NRAS mutations are associated with resistance to anti-EGFR therapy.
- Avastin® (bevacizumab): Blocks the growth of blood vessels to the tumour.
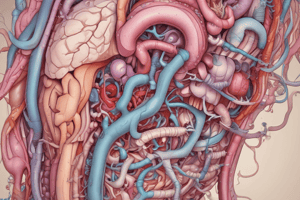
Neuroendocrine Tumours (Carcinoid)
- Tumours of neuroendocrine cells.
- Present throughout the gastrointestinal tract.
- Most common sites: appendix, small bowel, rectum, stomach, colon.
- May secrete numerous bioactive hormones (especially serotonin).
- Low grade malignant tumours.
- Behaviour correlates with size, location and depth of penetration.
Neuroendocrine Tumours (Carcinoid)- Pathology
- Solitary or multicentric firm, yellow-tan nodules.
- Usually submucosal masses, sometimes with ulceration.
- Cause striking desmoplastic response.
- Form islands, trabeculae, glands or sheets.
- Monotonous, speckled nuclei and abundant pink cytoplasm.
- Contain cytoplasmic secretory dense-core granules.
Immunohistochemistry Carcinoid Tumours
- Chromogranin
- Synaptophysin
- CD56
- Proliferation index Ki67
Grade Carcinoid Tumours (Neuroendocrine Tumours)
- Grade 1, 2, 3 - depending on number of mitoses and Ki67%.
Clinical Features of Carcinoid Tumours
-
Asymptomatic.
-
Obstruction.
-
Bleeding.
-
May release their products into circulation.
- Zollinger-Ellison syndrome (Gastrin).
- Cushing syndrome (adrenocorticotropic hormone).
- Hypoglycemia (insulin).
-
Carcinoid syndrome: Production of serotonin.
Carcinoid Syndrome
-
Seen only with massive liver metastases (5-HT is degraded in the liver).
-
Hepatic metastasis not required for extra-GI carcinoids.
-
Excess elaboration of serotonin, detected in blood and urine.
-
Symptoms:
- Vasomotor disturbances (skin flushing).
- Intestinal hypermotility (diarrhoea/cramps).
- Bronchospasm (wheezing, cough).
- Systemic fibrosis (with cardiac involvement, right ventricular subendocardial fibrosis, pulmonary and tricuspid valve).
- Hepatomegaly (metastasis).
-
Symptoms can be triggered by alcohol or emotional stress.
Mesenchymal Tumours
- Benign: lipoma, leiomyoma, schwannoma.
- Gastrointestinal stromal tumours (GISTs).
Gastrointestinal Stromal Tumours (GISTS)
- Mesenchymal neoplasms of the gastrointestinal tract.
- Arise from the pacemaker cells of the GIT (Interstitial cells of Cajal - ICC).
- 2/3 in the stomach.
- 25% in the small intestine.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.