Podcast
Questions and Answers
What is the primary target of the recipient's antibodies in Host-Versus-Graft Disease?
What is the primary target of the recipient's antibodies in Host-Versus-Graft Disease?
- Graft interstitium
- Graft stroma
- Graft vasculature (correct)
- Graft parenchyma
Which type of transplant rejection occurs immediately after transplantation?
Which type of transplant rejection occurs immediately after transplantation?
- Acute reaction
- Delayed reaction
- Hyperacute reaction (correct)
- Chronic reaction
In which of the following transplants is Graft-Versus-Host Disease most likely to occur?
In which of the following transplants is Graft-Versus-Host Disease most likely to occur?
- Bone marrow transplant (correct)
- Kidney transplant
- Heart transplant
- Liver transplant
What is the main characteristic of Chronic Host-Versus-Graft Disease?
What is the main characteristic of Chronic Host-Versus-Graft Disease?
What is the primary mechanism of Antibody-Mediated Diseases?
What is the primary mechanism of Antibody-Mediated Diseases?
What is the primary cause of Autoimmune disorders?
What is the primary cause of Autoimmune disorders?
Which of the following is a characteristic of Chronic Rejection?
Which of the following is a characteristic of Chronic Rejection?
Which of the following is NOT a type of transplant rejection?
Which of the following is NOT a type of transplant rejection?
What is the primary reason for the development of transplantation immunopathology?
What is the primary reason for the development of transplantation immunopathology?
What type of transplantation occurs when the donor and recipient are identical twins?
What type of transplantation occurs when the donor and recipient are identical twins?
What is the primary mechanism by which the host immune system recognizes and responds to allografts?
What is the primary mechanism by which the host immune system recognizes and responds to allografts?
What type of immune response is triggered by the recognition of foreign MHC molecules by host CD4+ helper T cells?
What type of immune response is triggered by the recognition of foreign MHC molecules by host CD4+ helper T cells?
What is the role of dendritic cells (DCs) in direct recognition of allografts?
What is the role of dendritic cells (DCs) in direct recognition of allografts?
What is the function of CD8+ T cells in direct recognition of allografts?
What is the function of CD8+ T cells in direct recognition of allografts?
What is the mechanism of indirect recognition of allografts?
What is the mechanism of indirect recognition of allografts?
What is the outcome of indirect recognition of allografts?
What is the outcome of indirect recognition of allografts?
What is the outcome when circulating cells are coated with autoantibodies and complement proteins?
What is the outcome when circulating cells are coated with autoantibodies and complement proteins?
What is the result of antibodies binding to cellular or tissue antigens?
What is the result of antibodies binding to cellular or tissue antigens?
What is the effect of antibodies against acetylcholine receptors in myasthenia gravis?
What is the effect of antibodies against acetylcholine receptors in myasthenia gravis?
What is the outcome of antibodies stimulating thyroid epithelial cells in Graves' disease?
What is the outcome of antibodies stimulating thyroid epithelial cells in Graves' disease?
What is the function of HLA antigens in the immune system?
What is the function of HLA antigens in the immune system?
What is the consequence of loss of immune tolerance?
What is the consequence of loss of immune tolerance?
What is the process by which autoreactive T cells are eliminated in the thymus?
What is the process by which autoreactive T cells are eliminated in the thymus?
Why do some autoreactive lymphocytes escape clonal deletion in the thymus?
Why do some autoreactive lymphocytes escape clonal deletion in the thymus?
What is the mechanism of peripheral tolerance that involves the functional inactivation of lymphocytes?
What is the mechanism of peripheral tolerance that involves the functional inactivation of lymphocytes?
Which of the following is NOT a mechanism of peripheral tolerance?
Which of the following is NOT a mechanism of peripheral tolerance?
What is the term for the phenomenon where the body's response to a microbial antigen attacks self-tissues?
What is the term for the phenomenon where the body's response to a microbial antigen attacks self-tissues?
Which of the following is a genetic factor that contributes to the development of autoimmune diseases?
Which of the following is a genetic factor that contributes to the development of autoimmune diseases?
What is the term for the deletion or inactivation of autoreactive T cells or B cells that escaped elimination in the central lymphoid organs?
What is the term for the deletion or inactivation of autoreactive T cells or B cells that escaped elimination in the central lymphoid organs?
Which of the following is an example of an immune-privileged site?
Which of the following is an example of an immune-privileged site?
What is the mechanism of peripheral tolerance that involves the apoptosis of mature lymphocytes as a result of self-antigen recognition?
What is the mechanism of peripheral tolerance that involves the apoptosis of mature lymphocytes as a result of self-antigen recognition?
Which of the following is a trigger for autoimmunity?
Which of the following is a trigger for autoimmunity?
What is the primary mechanism by which the provirus genome integrates into host cell DNA?
What is the primary mechanism by which the provirus genome integrates into host cell DNA?
What is the primary mechanism of immune deficiency in HIV infection?
What is the primary mechanism of immune deficiency in HIV infection?
What is the primary site of acute infection in HIV?
What is the primary site of acute infection in HIV?
What is a common clinical feature of HIV infection?
What is a common clinical feature of HIV infection?
What is a late complication of HIV infection?
What is a late complication of HIV infection?
What is a consequence of chronic HIV infection?
What is a consequence of chronic HIV infection?
Flashcards are hidden until you start studying
Study Notes
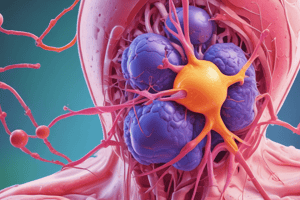
Transplantation Immunopathology
- Solid organ and bone marrow transplants have become routine due to understanding of humoral and cellular immune response, development of immunosuppressive drugs, and understanding of MHC (Major Histocompatibility Complex) antigens.
- MHC antigens are cell surface antigens that determine whether transplanted tissue is recognized as foreign or not.
Types of Transplantation
- Allogeneic: Donor and recipient are related or unrelated but share similar HLA types.
- Syngeneic: Donor and recipient are identical twins.
- Autologous: Donor and recipient are the same person.
Immune Recognition of Allografts
- Rejection of allografts is a response to MHC molecules, which are highly polymorphic.
- There are two main mechanisms of host immune system recognition and response to MHC molecules on the graft:
- Direct recognition: Host T cells directly recognize foreign MHC molecules on graft cells.
- Indirect recognition: Host CD4+ T cells recognize donor MHC molecules after they are picked up, processed, and presented by host APCs.
Host-Versus-Graft Disease (HVGD)
- If the transplanted graft bears foreign MHC antigens, the recipient's immune system attacks the donor cells of the transplanted organ.
- Rejection involves T cell-mediated and circulating antibody responses.
- Three basic patterns of transplant rejection:
- Hyperacute reaction: Occurs immediately after transplantation, often in kidney transplants.
- Acute rejection: Usually occurs within the first few months after transplantation, evidenced by signs of organ failure.
- Chronic HVGD: Occurs over a prolonged period, manifest by dense fibrosis of the intimal layer of blood vessels in the transplanted organ.
Graft-Versus-Host Disease (GVHD)
- GVHD occurs when the cellular immune system of the transplanted graft (donor T cells) recognizes and attacks the unrelated recipient HLA.
- Occurs mainly in:
- Bone marrow transplant.
- Severely immunocompromised patients who have received blood products containing HLA-incompatible lymphocytes.
- After transplantation of solid organs rich in lymphoid cells (e.g., the liver).
Autoimmune Disorders
- Caused by a breakdown in the ability of the immune system to differentiate between self and non-self antigens.
- Normally, there is a high degree of immunologic tolerance to self-antigens, which prevents the immune system from destroying the host.
- Autoimmune diseases can affect almost any cell or tissue in the body.
- Some autoimmune disorders are tissue-specific, while others affect multiple organs and systems.
Mechanisms of Antibody-Mediated Diseases
- Opsonization and phagocytosis: Circulating cells coated with autoantibodies are targeted for phagocytosis by neutrophils and macrophages.
- Inflammation: Antibodies bound to cellular or tissue antigens activate the complement system, recruiting neutrophils and monocytes, triggering inflammation in tissues.
- Antibody-mediated cellular dysfunction:
- Antibodies can impair or dysregulate cellular function without causing cell injury or inflammation (e.g., myasthenia gravis).
- Antibodies can stimulate cell function inappropriately (e.g., Graves' disease).
Immunologic Tolerance
- The ability of the immune system to differentiate self from non-self antigens by the presence of HLA antigens.
- Autoimmune diseases result from loss of immune tolerance.
- Central tolerance: Elimination of autoreactive T cells in the thymus and B cells in the bone marrow.
- Peripheral tolerance: Deletion or inactivation of autoreactive T cells or B cells that escaped elimination in the central lymphoid organs.
- Several mechanisms in peripheral tissues that silence autoreactive T cells:
- Anergy: Functional inactivation of lymphocytes.
- Suppression of the response of T lymphocytes by regulatory T cells.
- Activation-induced cell death: Apoptosis of mature lymphocytes as a result of self-antigen recognition.
- Antigen sequestration: Some antigens are hidden from the immune system because they are located in immune-privileged sites.
Mechanisms of Autoimmune Disease
- Breakdown of self-tolerance and development of autoimmunity are related to the inheritance of various susceptibility genes and changes in tissues, often induced by infections or injury.
- Genetic factors play an important role in the development of autoimmune diseases.
- Role of infections and tissue injury:
- Molecular mimicry: Viruses and other microbes share cross-reacting epitopes with self-antigens, leading to an immune response that attacks self-tissues.
- Viral replication: Provirus genome integrates into host cell DNA, and viral gene expression is triggered by stimuli that activate infected cells.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.