Podcast
Questions and Answers
What is the primary storage form of iron in the body?
What is the primary storage form of iron in the body?
- Ferritin (correct)
- Hemosiderin
- Transferrin
- Globin
Which of the following foods is a rich source of heme iron?
Which of the following foods is a rich source of heme iron?
- Beef liver (correct)
- Whole grains
- Spinach
- Dark chocolate
What regulates iron absorption and metabolism in the body?
What regulates iron absorption and metabolism in the body?
- Ferroportin
- Ferritin
- Transferrin
- Hepcidin (correct)
Which vitamin enhances the absorption of nonheme iron?
Which vitamin enhances the absorption of nonheme iron?
In what scenario would you expect an increase in iron transport proteins like DMT1 and transferrin receptors?
In what scenario would you expect an increase in iron transport proteins like DMT1 and transferrin receptors?
Which of the following is a common sign of iron deficiency anemia?
Which of the following is a common sign of iron deficiency anemia?
What is the average daily iron loss for an adult male?
What is the average daily iron loss for an adult male?
Which mechanism primarily facilitates the absorption of heme iron in the intestines?
Which mechanism primarily facilitates the absorption of heme iron in the intestines?
What can cause iron toxicity in humans?
What can cause iron toxicity in humans?
Which of the following groups is at the highest risk for iron deficiency worldwide?
Which of the following groups is at the highest risk for iron deficiency worldwide?
Which food component can inhibit nonheme iron absorption?
Which food component can inhibit nonheme iron absorption?
What condition may result from chronic iron overload?
What condition may result from chronic iron overload?
What condition arises from a hereditary defect leading to excessive iron absorption and storage?
What condition arises from a hereditary defect leading to excessive iron absorption and storage?
Which of the following is not typically a sign of iron deficiency anemia?
Which of the following is not typically a sign of iron deficiency anemia?
Which of the following conditions can increase the body's iron requirements?
Which of the following conditions can increase the body's iron requirements?
Which of the following assessments indicates the proportion of total blood volume that is red blood cells?
Which of the following assessments indicates the proportion of total blood volume that is red blood cells?
Which metal primarily exists in the form of Zn2+ in biological systems?
Which metal primarily exists in the form of Zn2+ in biological systems?
What treatment is recommended for managing hemochromatosis?
What treatment is recommended for managing hemochromatosis?
Which food source is considered very high in zinc content?
Which food source is considered very high in zinc content?
What factor can decrease zinc absorption in the body?
What factor can decrease zinc absorption in the body?
How is zinc transported in the blood?
How is zinc transported in the blood?
Which zinc transporter proteins are responsible for increasing cytoplasmic zinc concentration?
Which zinc transporter proteins are responsible for increasing cytoplasmic zinc concentration?
What is a primary contributor to the tight homeostatic control of zinc?
What is a primary contributor to the tight homeostatic control of zinc?
What is the average hemoglobin content in each red blood cell called?
What is the average hemoglobin content in each red blood cell called?
Which condition typically results from excessive intake or absorption of iron?
Which condition typically results from excessive intake or absorption of iron?
What is the typical dietary source of zinc that has moderate bioavailability?
What is the typical dietary source of zinc that has moderate bioavailability?
What inhibits zinc absorption due to its formation of complexes with zinc?
What inhibits zinc absorption due to its formation of complexes with zinc?
What percentage of the U.S. diet for zinc typically comes from animal products?
What percentage of the U.S. diet for zinc typically comes from animal products?
Flashcards
Iron Storage
Iron Storage
Iron stored primarily in liver, bone marrow, and spleen, mainly in the form of ferritin.
Ferritin
Ferritin
Primary storage form of iron, capable of holding up to 4500 iron atoms. Most is found intracellularly, with a small amount circulating in the blood.
Hemosiderin
Hemosiderin
A protein composed of damaged ferritin. Stores iron at a slower rate than ferritin and is formed when ferritin's capacity is exceeded.
Hepcidin
Hepcidin
Signup and view all the flashcards
Transferrin
Transferrin
Signup and view all the flashcards
Transferrin Receptor (TfR)
Transferrin Receptor (TfR)
Signup and view all the flashcards
Reductases
Reductases
Signup and view all the flashcards
Hepcidin
Hepcidin
Signup and view all the flashcards
Hemochromatosis
Hemochromatosis
Signup and view all the flashcards
Iron Toxicity
Iron Toxicity
Signup and view all the flashcards
Ferroportin
Ferroportin
Signup and view all the flashcards
Iron Deficiency Anemia
Iron Deficiency Anemia
Signup and view all the flashcards
Plasma Ferritin
Plasma Ferritin
Signup and view all the flashcards
Iron Depletion
Iron Depletion
Signup and view all the flashcards
Serum Transferrin Receptor Levels
Serum Transferrin Receptor Levels
Signup and view all the flashcards
Zinc
Zinc
Signup and view all the flashcards
Iron Overload
Iron Overload
Signup and view all the flashcards
Pica
Pica
Signup and view all the flashcards
Zinc Absorption
Zinc Absorption
Signup and view all the flashcards
Heme Proteins
Heme Proteins
Signup and view all the flashcards
ZIP Transporters
ZIP Transporters
Signup and view all the flashcards
ZnT Transporters
ZnT Transporters
Signup and view all the flashcards
Zinc Transport and Storage
Zinc Transport and Storage
Signup and view all the flashcards
Factors Affecting Zinc Absorption (Decreasing)
Factors Affecting Zinc Absorption (Decreasing)
Signup and view all the flashcards
Factors Affecting Zinc Absorption (Increasing)
Factors Affecting Zinc Absorption (Increasing)
Signup and view all the flashcards
Zinc Excretion
Zinc Excretion
Signup and view all the flashcards
Hemoglobin (Hgb)
Hemoglobin (Hgb)
Signup and view all the flashcards
Hematocrit (Hct)
Hematocrit (Hct)
Signup and view all the flashcards
Study Notes
Trace and Ultratrace Minerals
- Learning objectives include identifying good food sources, explaining digestion/absorption/transport/storage/excretion, describing functions & mechanisms of action, explaining recommended intakes, deficiencies, and toxicities, and explaining how essential mineral status is assessed
Iron
- Iron exists in several oxidation states, but only Fe2+ (ferrous) and Fe3+ (ferric) are stable in the body and food.
- Heme iron (50-60% of iron in meat, fish, and poultry, especially red meats, oysters, and clams) is absorbed more readily than nonheme iron from plant foods, dairy (poor source), whole grains, nuts, legumes, tofu, and spinach.
- Nonheme iron requires hydrolysis and reduction to be absorbed.
- Fortified breads, rolls, pasta, cereals, and flour provide additional iron.
- High doses of oral iron supplements can cause problems such as constipation, stomach pain, and nausea.
Iron Content of Selected Foods
- Breakfast cereals provide 100% of the Daily Value (DV) for iron per serving.
- Other examples of iron-rich foods are Oysters, White beans, Dark Chocolate, Beef Liver, Lentils, Spinach, Tofu, Kidney beans, Chickpeas, Canned Tomatoes, Beef, Potatoes, and Cashew nuts. Iron content and percentage DV are listed for each.
- DV= 18 mg.
Digestion & Absorption
- Heme Iron: Proteases digest heme from the globin, leaving heme intact for absorption into the enterocyte. Inside the enterocyte heme is hydrolyzed into Fe²⁺ and protoporphyrin.
- Nonheme Iron: Food components must be hydrolyzed and iron is reduced to cross the intestinal membrane. Stomach acid (HCl) helps reduce Fe³⁺ to Fe²⁺; reductases at the brush border further reduce Fe³⁺ to Fe²⁺.
- Enhancers of iron absorption include sugars, vitamin C, meat, fish, or poultry consumed alongside nonheme sources, and low iron status (hypoxia).
- Inhibitors include polyphenols, oxalates, phytates, and divalent cations like calcium, zinc, and manganese and an alkaline pH.
Absorption
- Enhancers of nonheme iron absorption (factors that increase absorption):
- Vitamin C, sugars, meat, fish, and poultry with nonheme iron
- Low iron status (hypoxia).
- Inhibitors of nonheme iron absorption:
- Polyphenols, oxalates, phytates, divalent cations (calcium, zinc, manganese), an alkaline pH.
- Acidic pH is optimal.
Iron Must Be Oxidized for Transport
- Fe2+ crosses the basolateral membrane through ferroportin.
- Hephaestin in the intestine, and ceruloplasmin in other cells and plasma, oxidize Fe2+ into Fe3+ as it leaves the cell.
- Fe3+ can then bind to transferrin for transport.
Transport and Cellular Uptake
- Free iron is potentially harmful, increasing free radical production.
- Transferrin transports and delivers iron to cells. It's a glycoprotein with two Fe-binding sites; 20-40% is saturated with iron in healthy conditions, while the remainder is available to bind other minerals.
- Transferrin receptors (TfR1 on almost all cells and TfR2 in hepatocytes and erythroblasts) take up transferrin-bound iron. TfR2 regulates liver iron and hepcidin synthesis.
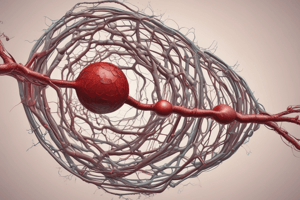
Iron Storage
- Iron is stored primarily in the liver (60%), bone marrow, and spleen.
- Ferritin is the primary storage form, a spherical protein with a hollow core.
- The hollow core contains iron in a variety of ferric compounds.
- Iron is deposited in the center as a variety of ferric compounds.
- Damaged ferritin forms hemosiderin.
Systemic Iron Regulation
- The liver detects iron status via Tf saturation, triggering the release of hepcidin.
- Hepcidin binds to ferroportin, inhibiting iron transport from enterocytes, hepatocytes, and reticuloendothelial macrophages.
- Iron accumulates in these cells
Cellular Iron Regulation
- Iron regulatory proteins 1 and 2 (IRP1 and IRP2) bind to iron response elements (IREs) in specific mRNA segments, regulating the synthesis of iron-related proteins.
- Low iron: ↑ DMT1, TfR, DCYTB, ferroportin, ↓ ferritin, & ALAS.
- High iron: ↓ DMT1, TfR, DCYTB, ferroportin, ↑ ferritin, & ALAS.
Zinc
- Zinc is primarily found in its divalent form (Zn2+) in the body.
- Good sources: red meats (organ meats) and seafood, poultry, pork, dairy, whole grains, leafy vegetables, and root vegetables.
- Heating can reduce zinc bioavailability.
- Sources in pancreatic and biliary secretions are absorbed for re-use.
- Supplemental zinc comes in various forms (pills, lozenges).
Zinc Transporters
- ZIP transporters increase cytoplasmic zinc concentration.
- ZnT transporters facilitate zinc efflux.
- Both ZIP and ZnT genes can be up or downregulated in response to zinc.
Factors Influencing Zinc Absorption
- Enhancers include organic acids, glutathione, and amino acids.
- Inhibitors include phytic acid, oxalic acid, polyphenols, and selected nutrients.
Zinc Functions
- Crucial for protein synthesis, cell membrane structure and function, skin integrity, cell-mediated immunity, sexual maturation, fertility and reproduction, insulin synthesis and storage, taste, and basal metabolic rate.
Copper
- Copper exists in both cuprous (Cu1+) and cupric (Cu2+) forms, but most is in the Cu2+ form
- The richest sources are organ meats and shellfish.
- Other good sources include nuts, seeds, legumes, dried fruits, potatoes, whole grains, and cocoa
Copper Content of Selected Foods
- A list of various foods provides their content of Copper in µg and % daily value (DV).
Copper Absorption
- Enhancers include some amino acids, glutathione, and acids
- Inhibitors include phytic acid and zinc.
Copper Homeostasis
- Copper is transported to the liver in albumin and other protein complexes.
- The liver deals with copper uptake via CTR1, CTR2, DMT1, and other receptors.
- Copper binds metallothionein.
- Chaperones direct intracellular trafficking and Cu delivery for metabolism.
Copper Storage and Excretion
- Relatively little copper is stored, widely distributed throughout the tissues
- The liver is the major storage organ.
- Excreted mostly as bile into feces and smaller amounts in sweat and exfoliated skin cells.
Copper Functions and Mechanisms of Action
- Ceruloplasmin (and hephaestin) function as an oxidase that oxidizes minerals, e.g. Fe2+ → Fe3+, in the circulation.
- Antioxidant, modulating inflammatory and infection responses.
- Other functions: Superoxide dismutase (SOD), ATP production, connective tissue formation, neurotransmitter synthesis, and melanin synthesis.
Selenium
- Selenium exists in different oxidation states and is chemically similar to sulfur, replacing sulfur in certain amino acids.
- Selenium content varies in food based on soil concentrations.
- Animal foods generally have more selenium than plants.
- Absorption is not affected by nutritional status and directly related to food levels.
Selenium in Selected Food Sources
- A list of various foods provides their content of Selenium in µg and daily value (DV).
Selenium Transport, Storage, and Excretion
- Transported in blood attached to hemoglobin, albumin, and red blood cells.
- The liver takes up around 50% on the first pass.
- Se is metabolized into selenoprotein P (SePP1).
- Stored in liver, kidney, and spleen, and excreted mostly in urine and bile.
Selenium Functions
- Selenoproteins play a role in antioxidant activity (removing ROS (hydroperoxides).
- Roles include maintaining thyroid homeostasis, and reducing and removing signal molecules.
Recommended Intakes, Deficiency, Toxicity, and Assessment (for each mineral)
Deficiency
- Insufficient dietary intake, reduced absorption, and/or normal blood loss are sources of deficiency.
- Deficiency can appear in early stages, progressing to anemia.
Toxicity
- Related to excessive intake usually of supplements
- Chronic cases involve organ damage.
Assessment
- General methods to assess mineral status and identify potential deficiencies in relevant minerals.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.