Podcast
Questions and Answers
What is a significant disadvantage of using hydrogels for cell scaffolding?
What is a significant disadvantage of using hydrogels for cell scaffolding?
Which type of scaffold is characterized by flattened cells?
Which type of scaffold is characterized by flattened cells?
What is a primary advantage of foam or sponge scaffolds?
What is a primary advantage of foam or sponge scaffolds?
What challenge must be addressed when finding the optimal scaffold for tissue engineering?
What challenge must be addressed when finding the optimal scaffold for tissue engineering?
Signup and view all the answers
Which strategy involves using both cartilage and bone components in a scaffold?
Which strategy involves using both cartilage and bone components in a scaffold?
Signup and view all the answers
What is the primary purpose of lubrication in articular cartilage?
What is the primary purpose of lubrication in articular cartilage?
Signup and view all the answers
Which type of lubrication involves lubricin forming a monolayer on each articular surface?
Which type of lubrication involves lubricin forming a monolayer on each articular surface?
Signup and view all the answers
In film-fluid lubrication, what does hydrodynamic lubrication primarily achieve?
In film-fluid lubrication, what does hydrodynamic lubrication primarily achieve?
Signup and view all the answers
What characterizes film-press lubrication?
What characterizes film-press lubrication?
Signup and view all the answers
What predominates in areas of greater friction during mixed lubrication?
What predominates in areas of greater friction during mixed lubrication?
Signup and view all the answers
How does viscoelasticity manifest in articular cartilage under load?
How does viscoelasticity manifest in articular cartilage under load?
Signup and view all the answers
What is the distinction between film-fluid lubrication and barrier lubrication?
What is the distinction between film-fluid lubrication and barrier lubrication?
Signup and view all the answers
What is one characteristic of articular cartilage under a constant load?
What is one characteristic of articular cartilage under a constant load?
Signup and view all the answers
What is a key characteristic of inadequate cartilage compression related to patellar chondropathy?
What is a key characteristic of inadequate cartilage compression related to patellar chondropathy?
Signup and view all the answers
Which muscle is specifically highlighted as a vital dynamic stabilizer in patellar stability?
Which muscle is specifically highlighted as a vital dynamic stabilizer in patellar stability?
Signup and view all the answers
What type of trauma may lead to patellar subluxation?
What type of trauma may lead to patellar subluxation?
Signup and view all the answers
In the context of cartilage regeneration, what is microfracture?
In the context of cartilage regeneration, what is microfracture?
Signup and view all the answers
What is a disadvantage of the microfracture technique in cartilage regeneration?
What is a disadvantage of the microfracture technique in cartilage regeneration?
Signup and view all the answers
Which of the following factors contributes to abnormal patellofemoral morphology?
Which of the following factors contributes to abnormal patellofemoral morphology?
Signup and view all the answers
What does a greater than 20-degree Q angle indicate?
What does a greater than 20-degree Q angle indicate?
Signup and view all the answers
What outcomes can imbalance of the patellar structure lead to?
What outcomes can imbalance of the patellar structure lead to?
Signup and view all the answers
What is a major drawback of autologous chondrocyte implantation (ACI)?
What is a major drawback of autologous chondrocyte implantation (ACI)?
Signup and view all the answers
Which process is involved in autologous chondrocyte implantation (ACI)?
Which process is involved in autologous chondrocyte implantation (ACI)?
Signup and view all the answers
What has been a main challenge in tissue engineering for cartilage?
What has been a main challenge in tissue engineering for cartilage?
Signup and view all the answers
What is a potential limitation of fibrocartilage in relation to joint functionality?
What is a potential limitation of fibrocartilage in relation to joint functionality?
Signup and view all the answers
What is a significant advantage of osteochondral auto-grafts compared to allo-grafts?
What is a significant advantage of osteochondral auto-grafts compared to allo-grafts?
Signup and view all the answers
What factor limits the length of post-operative treatment in osteochondral grafts?
What factor limits the length of post-operative treatment in osteochondral grafts?
Signup and view all the answers
In the process of preparing for autologous chondrocyte implantation (ACI), what is the timeframe after which chondrocyte injection occurs?
In the process of preparing for autologous chondrocyte implantation (ACI), what is the timeframe after which chondrocyte injection occurs?
Signup and view all the answers
What is a benefit of physical exercise in relation to joint health?
What is a benefit of physical exercise in relation to joint health?
Signup and view all the answers
Which of the following is a characteristic of muscle strength training for osteoarthritis?
Which of the following is a characteristic of muscle strength training for osteoarthritis?
Signup and view all the answers
What is the primary focus of joint activity training?
What is the primary focus of joint activity training?
Signup and view all the answers
In terms of aerobic exercise, which statement is accurate?
In terms of aerobic exercise, which statement is accurate?
Signup and view all the answers
What role does aquatic exercise therapy play in joint care?
What role does aquatic exercise therapy play in joint care?
Signup and view all the answers
What characteristic is essential for scaffolds used in cartilage tissue engineering?
What characteristic is essential for scaffolds used in cartilage tissue engineering?
Signup and view all the answers
What is a major concern with using autologous chondrocyte cell lines?
What is a major concern with using autologous chondrocyte cell lines?
Signup and view all the answers
Which of the following statements about mesenchymal stem cells is accurate?
Which of the following statements about mesenchymal stem cells is accurate?
Signup and view all the answers
Which natural polymer is mentioned as promoting the re-differentiation of encapsulated chondrocytes?
Which natural polymer is mentioned as promoting the re-differentiation of encapsulated chondrocytes?
Signup and view all the answers
What is a significant benefit of synthetic polymers in scaffold matrices?
What is a significant benefit of synthetic polymers in scaffold matrices?
Signup and view all the answers
Chondroprogenitor cells are highlighted for their:
Chondroprogenitor cells are highlighted for their:
Signup and view all the answers
During in vivo tissue development, what property must scaffolds maintain?
During in vivo tissue development, what property must scaffolds maintain?
Signup and view all the answers
What is a common misconception regarding the reliability of chondrocyte cell lines?
What is a common misconception regarding the reliability of chondrocyte cell lines?
Signup and view all the answers
Flashcards
Lubrication
Lubrication
The process of reducing friction between moving surfaces by introducing a fluid between them.
Barrier lubrication
Barrier lubrication
Lubricin, a glycoprotein, forms a thin layer on each articular surface, preventing direct contact.
Film-fluid lubrication
Film-fluid lubrication
Creating a thicker layer of fluid between surfaces to separate them and support weight.
Hydrodynamic lubrication
Hydrodynamic lubrication
Signup and view all the flashcards
Film-press lubrication
Film-press lubrication
Signup and view all the flashcards
Mixed lubrication
Mixed lubrication
Signup and view all the flashcards
Viscoelasticity
Viscoelasticity
Signup and view all the flashcards
Viscoelastic response of cartilage
Viscoelastic response of cartilage
Signup and view all the flashcards
Etiopathogenic Factors
Etiopathogenic Factors
Signup and view all the flashcards
Patellar Imbalance
Patellar Imbalance
Signup and view all the flashcards
Patellofemoral Congruence
Patellofemoral Congruence
Signup and view all the flashcards
Extensor Apparatus
Extensor Apparatus
Signup and view all the flashcards
Q Angle
Q Angle
Signup and view all the flashcards
Microfracture
Microfracture
Signup and view all the flashcards
Autologous Chondrocyte Implantation (ACI)
Autologous Chondrocyte Implantation (ACI)
Signup and view all the flashcards
Osteochondral Autograft
Osteochondral Autograft
Signup and view all the flashcards
Osteochondral Auto-/Allograft
Osteochondral Auto-/Allograft
Signup and view all the flashcards
Challenge in Cartilage Tissue Engineering
Challenge in Cartilage Tissue Engineering
Signup and view all the flashcards
Enzymatic Digestion
Enzymatic Digestion
Signup and view all the flashcards
In Vitro Expansion of Chondrocytes
In Vitro Expansion of Chondrocytes
Signup and view all the flashcards
Tissue Engineering
Tissue Engineering
Signup and view all the flashcards
Load Bearing Capacity
Load Bearing Capacity
Signup and view all the flashcards
Long-Term Functionality
Long-Term Functionality
Signup and view all the flashcards
Autologous chondrocyte cell lines
Autologous chondrocyte cell lines
Signup and view all the flashcards
Chondroprogenitor cells
Chondroprogenitor cells
Signup and view all the flashcards
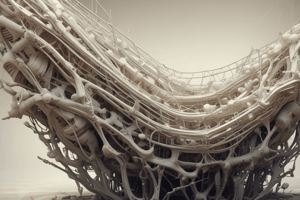
Matrices for cartilage tissue engineering
Matrices for cartilage tissue engineering
Signup and view all the flashcards
Natural polymers as scaffold matrices
Natural polymers as scaffold matrices
Signup and view all the flashcards
Synthetic polymers as scaffold matrices
Synthetic polymers as scaffold matrices
Signup and view all the flashcards
Degrading Scaffold
Degrading Scaffold
Signup and view all the flashcards
Non-Degrading Scaffold
Non-Degrading Scaffold
Signup and view all the flashcards
Chondrogenesis
Chondrogenesis
Signup and view all the flashcards
Hydrogels
Hydrogels
Signup and view all the flashcards
Fibrous Scaffolds
Fibrous Scaffolds
Signup and view all the flashcards
Stratification of Scaffolds
Stratification of Scaffolds
Signup and view all the flashcards
Bilayer System
Bilayer System
Signup and view all the flashcards
Multizonal Scaffold
Multizonal Scaffold
Signup and view all the flashcards
Joint Activity Training
Joint Activity Training
Signup and view all the flashcards
Aerobic Exercise
Aerobic Exercise
Signup and view all the flashcards
Aquatic Exercise Therapy
Aquatic Exercise Therapy
Signup and view all the flashcards
Muscle Strength Training
Muscle Strength Training
Signup and view all the flashcards
Multipoint Intermittent Isometric Exercise
Multipoint Intermittent Isometric Exercise
Signup and view all the flashcards
Study Notes
Cartilage Composition and Structure
- Cartilage is a white, solid, strong, and elastic connective tissue.
- It's crucial for supporting and enabling movement of body parts.
- Cartilage doesn't contain blood vessels or nerves.
- Functions include: bone movement in joints, providing a framework for some organs, and shaping long bones.
Types of Cartilage
- Hyaline cartilage (articular cartilage): Common, with few cells and fibers, surrounded by perichondrium.
- Elastic cartilage: Features numerous, large chondrocytes, rich in elastic fibers, also surrounded by perichondrium.
- Fibrocartilage: Has intermediate characteristics between dense connective tissue and hyaline cartilage. Chondrocytes are arranged in rows, containing collagens I and II, and lacks perichondrium.
Components of Articular Cartilage
- Extracellular matrix: Consists of fibers and ground substance.
- Cells: Include chondrogenic cells, chondroblasts, and chondrocytes.
- Perichondrium: Connective tissue surrounding cartilage.
Chondrogenic Cells and Development
- Chondrogenic cells (stem cells) differentiate into chondroblasts.
- Chondroblasts mature into chondrocytes.
- Chondrocytes maintain and maintain extracellular matrix.
- Chondrocytes are found inside lacunae, or chondroplasts.
Articular Cartilage Structure
- Surface zone: Elongated chondrocytes in parallel arrangement with surface collagen.
- Intermediate zone: Chondrocytes without specific order.
- Deep zone: Chondrocytes arranged in groups perpendicular to the surface with collagen.
- Calcified zone: Contains calcified matrix.
Cartilage Locations
- Articular cartilage is found in various locations, including the skeleton, growth plates, nasal septum, and the surfaces of mobile joints (e.g., knees, ankles, hips).
Lubrication of Articular Cartilage
- Barrier lubrication: Lubricin (a glycoprotein) forms a monolayer on articular surfaces.
- Film-fluid lubrication: Fluid separation between surfaces supports load.
Cartilage Wear
- Cartilage wear is related to imbalance between synthesis and degradation.
- Factors like overweight accelerate wear.
- Age produces changes in cells, leading to decreased tissue maintenance and increasing wear.
- Overuse of joints causes repetitive loads that lead to tissue deformity.
Cartilage Injuries
- Chondropathics: Minor repetitive trauma, pressure from cartilage, or direct trauma.
- Osteochondritis: Gradual wear from excess load or synovial fluid viscosity change/injury to cartilage.
- Osteochondritis dissecans: Degeneration of central zone of cartilage, thickening of perichondrium/cartilage edge; possible ossification, bone "mice."
Tissue Engineering for Cartilage Repair
- Microfracture: Removes damaged cartilage and creates fibrocartilage.
- ACI (Autologous chondrocyte implantation): A two-stage approach that is surgically intensive, involves cartilage biopsy and in vitro chondrocyte expansion, then implantation.
- Osteochondral auto- and allografts: A surgical cartilage transplant including the subchondral bone.
Cell Sources and Culture Conditions
- Autologous chondrocytes are lines that may not reflect phenotypic changes found in vivo or lead to tumors from unlimited proliferation.
- Mesenchymal stem or chondroprogenitor cells better alternatives to stem cells.
Biomaterials
- Matrices: Biocompatible, biodegradable scaffolds capable of supporting and stimulating chondrogenesis, to support joint load.
- Natural polymers: Collagen, hyaluronic acid, etc.
- Synthetic polymers: Polymers provide mechanical support and control degradation.
Future Challenges and Exercise for Cartilage
- Challenges include finding optimal scaffolds, cell sources, and mimicking cartilage development in vitro.
- Exercise can prevent damage and improve joint function by preventing/reducing cartilage wear, increasing ligament function, and improving muscle and strength.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz explores the properties and challenges of scaffolds used in tissue engineering, particularly focusing on hydrogels, foam, and sponge scaffolds. It also examines the lubrication mechanisms of articular cartilage, including various lubrication strategies and their implications for joint health.