Podcast
Questions and Answers
The thyroid gland's isthmus unites the two lobes in front of the first three tracheal rings.
The thyroid gland's isthmus unites the two lobes in front of the first three tracheal rings.
False (B)
The lateral surface of the thyroid lobe is superficial and directly visible without any muscular covering.
The lateral surface of the thyroid lobe is superficial and directly visible without any muscular covering.
False (B)
The upper pole of the thyroid lobe extends freely, unrestricted by any muscular attachments.
The upper pole of the thyroid lobe extends freely, unrestricted by any muscular attachments.
False (B)
The medial surface of the thyroid gland directly contacts the internal jugular vein.
The medial surface of the thyroid gland directly contacts the internal jugular vein.
The inferior thyroid artery arches behind the lower pole of the thyroid gland at the level of the C4 vertebra.
The inferior thyroid artery arches behind the lower pole of the thyroid gland at the level of the C4 vertebra.
The thoracic duct on the left side arches behind the lower pole of the thyroid at the level of the C6 vertebra.
The thoracic duct on the left side arches behind the lower pole of the thyroid at the level of the C6 vertebra.
The recurrent laryngeal nerve approaches the medial surface of the thyroid gland from above.
The recurrent laryngeal nerve approaches the medial surface of the thyroid gland from above.
The left recurrent laryngeal nerve is more likely to lie in front of the inferior thyroid artery.
The left recurrent laryngeal nerve is more likely to lie in front of the inferior thyroid artery.
On the right side, the recurrent laryngeal nerve always passes behind the inferior thyroid artery.
On the right side, the recurrent laryngeal nerve always passes behind the inferior thyroid artery.
Parathyroid glands are located within the pretracheal fascia, separate from the posterior surface of the thyroid gland.
Parathyroid glands are located within the pretracheal fascia, separate from the posterior surface of the thyroid gland.
The recurrent laryngeal nerve is situated anterior to the pretracheal fascia.
The recurrent laryngeal nerve is situated anterior to the pretracheal fascia.
The isthmus of the thyroid gland typically adheres to the fifth, sixth, and seventh tracheal rings.
The isthmus of the thyroid gland typically adheres to the fifth, sixth, and seventh tracheal rings.
The external laryngeal nerve provides motor innervation to the cricothyroid muscle and runs a few millimeters anterior to the superior thyroid artery.
The external laryngeal nerve provides motor innervation to the cricothyroid muscle and runs a few millimeters anterior to the superior thyroid artery.
The pyramidal lobe is a projection of glandular tissue typically found to the right of the midline.
The pyramidal lobe is a projection of glandular tissue typically found to the right of the midline.
The inferior thyroid artery typically originates from the subclavian artery, ascending laterally to the lower pole of the thyroid gland.
The inferior thyroid artery typically originates from the subclavian artery, ascending laterally to the lower pole of the thyroid gland.
The thyroidea ima artery, present in approximately 15% of individuals, usually originates from the internal carotid artery.
The thyroidea ima artery, present in approximately 15% of individuals, usually originates from the internal carotid artery.
The middle thyroid vein drains the superior aspect of the thyroid gland directly into the external jugular vein.
The middle thyroid vein drains the superior aspect of the thyroid gland directly into the external jugular vein.
Lymphatic drainage from the lower pole of the thyroid gland flows directly into the pretracheal nodes, following the path of the superior thyroid artery.
Lymphatic drainage from the lower pole of the thyroid gland flows directly into the pretracheal nodes, following the path of the superior thyroid artery.
The thyroid gland receives parasympathetic innervation directly from branches of the facial nerve.
The thyroid gland receives parasympathetic innervation directly from branches of the facial nerve.
Iodination of the colloid within the thyroid gland occurs inside the epithelial cells before its release into the follicles.
Iodination of the colloid within the thyroid gland occurs inside the epithelial cells before its release into the follicles.
The thyroid gland, despite its small size, has a relatively low blood flow compared to other organs.
The thyroid gland, despite its small size, has a relatively low blood flow compared to other organs.
Thyroxine (T5) and triiodothyronine (T2) are the primary hormonal products secreted by the thyroid gland.
Thyroxine (T5) and triiodothyronine (T2) are the primary hormonal products secreted by the thyroid gland.
C cells, responsible for calcitonin secretion, constitute approximately 20% of the epithelial cells in the thyroid gland.
C cells, responsible for calcitonin secretion, constitute approximately 20% of the epithelial cells in the thyroid gland.
The thyroid gland originates from the caudal end of the thyroglossal duct and the sixth pharyngeal pouch.
The thyroid gland originates from the caudal end of the thyroglossal duct and the sixth pharyngeal pouch.
During a partial thyroidectomy, dividing the sternohyoid and sternothyroid muscles near their upper ends risks damaging their nerve supplies from the vagus nerve.
During a partial thyroidectomy, dividing the sternohyoid and sternothyroid muscles near their upper ends risks damaging their nerve supplies from the vagus nerve.
The parathyroid glands are typically located anterior to the lateral lobes of the thyroid gland, within the pretracheal fascia.
The parathyroid glands are typically located anterior to the lateral lobes of the thyroid gland, within the pretracheal fascia.
In most individuals, there are six parathyroid glands, with a combined weight usually exceeding 500 mg.
In most individuals, there are six parathyroid glands, with a combined weight usually exceeding 500 mg.
The superior parathyroid gland usually resides on the anterior aspect of the thyroid lobe, inferior to the inferior thyroid artery.
The superior parathyroid gland usually resides on the anterior aspect of the thyroid lobe, inferior to the inferior thyroid artery.
Oxyphil cells, found within the parathyroid gland, are derived from lymphoid stem cells and are responsible for synthesizing parathyroid hormone.
Oxyphil cells, found within the parathyroid gland, are derived from lymphoid stem cells and are responsible for synthesizing parathyroid hormone.
The trachea maintains its patency due to complete cartilaginous rings connected by a muscular membrane.
The trachea maintains its patency due to complete cartilaginous rings connected by a muscular membrane.
Flashcards
Thyroid Isthmus
Thyroid Isthmus
Connects the two lobes of the thyroid gland.
Pretracheal Fascia
Pretracheal Fascia
Covers the thyroid gland, external to its own capsule.
Sternothyroid and Sternohyoid
Sternothyroid and Sternohyoid
Muscles that cover the lateral surface of the thyroid gland.
Sternocleidomastoid muscle
Sternocleidomastoid muscle
Overlaps the strap muscles covering the thyroid.
Signup and view all the flashcards
Cricothyroid muscle
Cricothyroid muscle
Relates to the medial surface of the thyroid gland.
Signup and view all the flashcards
Posterior Surface
Posterior Surface
Surface of the thyroid gland near the carotid artery.
Signup and view all the flashcards
Parathyroid Glands
Parathyroid Glands
Glands typically found on the posterior surface of the thyroid.
Signup and view all the flashcards
Inferior Thyroid Artery
Inferior Thyroid Artery
Artery that arches behind the lower pole of the thyroid.
Signup and view all the flashcards
Recurrent Laryngeal Nerve
Recurrent Laryngeal Nerve
Critical nerve near the thyroid, important in surgery.
Signup and view all the flashcards
Esophagus location
Esophagus location
Runs near the medial surface of the thyroid gland
Signup and view all the flashcards
External Laryngeal Nerve
External Laryngeal Nerve
Smaller nerve that supplies the cricothyroid muscle; runs close to the superior thyroid artery.
Signup and view all the flashcards
Pyramidal Lobe
Pyramidal Lobe
Projection of thyroid tissue upward from the isthmus, representing the thyroglossal duct.
Signup and view all the flashcards
Superior Thyroid Artery
Superior Thyroid Artery
Artery branching off the external carotid to supply the upper thyroid pole. Ligate at the pole to spare nerve.
Signup and view all the flashcards
Thyroidea Ima Artery
Thyroidea Ima Artery
Unpaired artery arising from the brachiocephalic trunk or aorta, supplying the isthmus in some individuals.
Signup and view all the flashcards
Middle Thyroid Vein
Middle Thyroid Vein
Vein that drains the middle of the thyroid lobe directly into the internal jugular vein.
Signup and view all the flashcards
Upper Pole Lymph Drainage
Upper Pole Lymph Drainage
Lymphatic drainage route from the upper thyroid pole to the anterosuperior deep cervical nodes.
Signup and view all the flashcards
Lower Pole Lymph Drainage
Lower Pole Lymph Drainage
Lymphatic drainage from lower thyroid pole following the inferior thyroid artery to posteroinferior deep cervical nodes.
Signup and view all the flashcards
Thyroxine (T4) and Triiodothyronine (T3)
Thyroxine (T4) and Triiodothyronine (T3)
Main hormonal products of the thyroid gland; regulate metabolism.
Signup and view all the flashcards
Thyroid C (Parafollicular) Cells
Thyroid C (Parafollicular) Cells
Epithelial cells in the thyroid that secrete calcitonin, which lowers blood calcium levels.
Signup and view all the flashcards
Thyroidectomy Incision Site
Thyroidectomy Incision Site
Surgical incision point for partial thyroidectomy.
Signup and view all the flashcards
Strap Muscles
Strap Muscles
Muscles that overlie the trachea during thyroid surgery.
Signup and view all the flashcards
Superior Parathyroid Gland
Superior Parathyroid Gland
More constant parathyroid gland located level with the first tracheal ring.
Signup and view all the flashcards
Parathyroid Hormone (PTH)
Parathyroid Hormone (PTH)
Parathyroid hormone; secreted by chief cells, increases blood calcium.
Signup and view all the flashcards
Oxyphil Cells
Oxyphil Cells
Cells in the parathyroid gland, probably derived from chief cells, function is unknown.
Signup and view all the flashcards
Trachea
Trachea
Connects the larynx to the lungs. Kept open by C-shaped cartilage rings.
Signup and view all the flashcardsStudy Notes
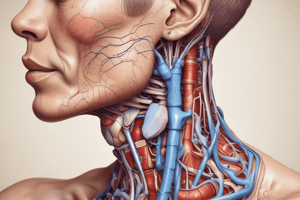
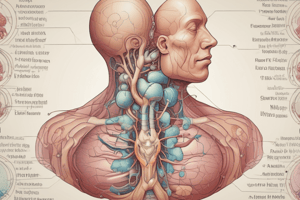
- The thyroid gland has two symmetrical lobes connected by an isthmus in front of the 2nd, 3rd, and 4th tracheal rings.
- The gland is enclosed by its capsule and the pretracheal fascia.
Lateral Lobes
- Pear-shaped with a narrow upper pole and broader lower pole.
- Roughly triangular in cross-section with lateral, medial, and posterior surfaces.
Lateral Surface
- Covered by sternothyroid and sternohyoid muscles.
- The upper pole is beneath the upper end of sternothyroid, limiting its expansion when enlarged.
- The lower end of sternocleidomastoid overlaps the strap muscles.
Medial Surface
- Lies against the larynx and upper trachea.
- The lower pole extends along the trachea to the 6th tracheal ring.
- The lower pharynx and upper esophagus are immediately behind.
- Related muscles include the cricothyroid and inferior constrictor.
- The external and recurrent laryngeal nerves approach it from above and below.
Posterior Surface
- Overlaps the medial part of the carotid sheath (containing the common carotid artery).
- Enlargement can extend across the internal jugular vein.
- Parathyroid glands typically lie in contact between the thyroid and fascial sheath.
- The inferior thyroid artery arches behind the lower pole, at the C6 vertebra.
- On the left, the thoracic duct also arches behind, but at the C7 vertebra.
Recurrent Laryngeal Nerve
- Crucial in thyroid surgery due to its proximity to the gland.
- Approaches the medial surface from below, usually in front of the groove between the trachea and esophagus.
- The left nerve is more likely to be behind the inferior thyroid artery, while the right has an equal chance of being in front or behind.
- The nerve may pass between branches of the artery.
- A minute artery is usually visible on the nerve’s surface, aiding identification.
- Located behind the pretracheal fascia, including the suspensory ligament of Berry.
- Passes upwards under the inferior constrictor, behind the cricothyroid joint.
- Often divides into two branches near the upper border of the isthmus.
- The anterior (larger) branch is motor to laryngeal muscles, and the posterior branch is sensory only.
- The occasional non-recurrent right laryngeal nerve should be considered.
External Laryngeal Nerve
- Supplies the cricothyroid muscle.
- Lies a millimeter or two behind the superior thyroid artery, passing medial to the upper pole.
Isthmus
- Joins the anterior surfaces of the lobes towards their lower poles.
- Its posterior surface is attached to the 2nd, 3rd, and 4th tracheal rings.
- The pretracheal fascia is fixed between the isthmus and trachea.
- Fixation causes the thyroid gland to move with the larynx during swallowing.
Arteries and Veins Around Isthmus
- An anastomosis between the two superior thyroid arteries exists across the upper border.
- Tributaries of the inferior thyroid veins emerge from the lower border.
Pyramidal Lobe
- A small projection of gland substance often extends upwards from the isthmus (usually left of midline).
- Represents glandular tissue development from the caudal end of the thyroglossal duct.
- Attached to the hyoid bone's inferior border by fibrous tissue.
- Muscle fibers (levator glandulae thyroideae) may be present, innervated by the external laryngeal nerve.
Accessory Thyroid Glands
- Separate masses of thyroid tissue found near the hyoid bone, in the tongue, mediastinum, or beneath the sternocleidomastoid.
Blood Supply: Superior Thyroid Artery
- The first branch from the external carotid's anterior aspect.
- Gives off sternocleidomastoid and superior laryngeal branches.
- Pierces the pretracheal fascia as a single vessel to the upper pole.
- The external laryngeal nerve is immediately behind the artery near the pole.
- Ligation occurs right at the pole to avoid nerve damage during thyroidectomies.
- Divides into an anterior branch (to the isthmus) and a posterior branch (anastomosing with the inferior thyroid artery).
- A separate branch from the left artery may supply the pyramidal lobe.
Blood Supply: Inferior Thyroid Artery
- Arises from the thyrocervical trunk.
- Arches upwards and medially behind the lower pole.
- Divides outside the pretracheal fascia into four or five branches that pierce the fascia.
- The suspensory ligament always contains small branches.
- The recurrent laryngeal nerve has a variable relationship, but always lies behind the pretracheal fascia.
- The artery is ligated lateral to the gland before it divides into terminal branches.
- The inferior thyroid artery gives off esophageal and inferior laryngeal branches.
Thyroidea Ima Artery
- Enters the lower part of the isthmus in 3% of individuals.
- Originates from the brachiocephalic trunk, right common carotid artery, or aortic arch.
- Represents a persistent embryonic vessel.
Venous Return
- The superior thyroid vein follows the superior thyroid artery and enters the internal jugular or facial vein.
- The middle thyroid vein (short and wide) passes directly from the middle of the lobe into the internal jugular vein.
- Inferior thyroid veins form a plexus in the pretracheal fascia, draining into the brachiocephalic veins (mostly the left).
Lymph Drainage
- Lymphatics follow the arteries.
- The upper pole drains into the anterosuperior group of deep cervical lymph nodes.
- The lower pole drains into the posteroinferior group, behind the carotid sheath.
- A few lymphatics pass downwards into pretracheal nodes along the thyroidea ima artery.
Nerve Supply
- The sympathetic supply (vasoconstrictor) comes from the middle cervical ganglion via the inferior thyroid artery.
- Some fibers from the superior cervical ganglion travel with the superior thyroid artery.
- Vagus nerve filaments are present, but their purpose is unknown.
Structure
- Composed of follicles (vesicles) filled with colloid, the iodine-containing product of follicular cells.
- Unique as the only endocrine gland storing secretion outside the cells.
- Colloid is iodinated in the follicle and reabsorbed by cells before being discharged into blood capillaries.
- Highly vascular.
- Main hormones produced are thyroxine (T4) and triiodothyronine (T3).
- C or parafollicular cells (less than 2%) secrete calcitonin.
- C cells are scattered on the outer aspects of follicles and don't reach the lumina.
Development
- Originates as a proliferation of cells from the caudal end of the thyroglossal duct.
- Parafollicular cells come from the ultimobranchial body (fifth pharyngeal pouch).
Surgical Approach
- For partial thyroidectomy, a transverse skin incision is made 2.5 cm above the jugular notch.
- The gap between sternohyoids and sternothyroids is opened to expose the trachea and isthmus.
- Muscles are retracted or divided to display lateral lobes, preserving nerve supplies from the ansa cervicalis.
- Vessels of each lobe are ligated and divided.
- The required portion of each lobe is removed, leaving parathyroids intact.
- Proper identification of the plane deep to sternothyroid and sternohyoid muscles is crucial to avoid damage to the internal jugular vein.
Parathyroid Glands
Location
- Normally lie behind the lateral lobe of the thyroid gland.
- Can be within or outside the thyroid's capsule of pretracheal fascia.
Number and Size
- Usually four glands (90% of subjects), two on each side.
- Total weight is not more than 200 mg.
Superior Gland
- More constant in position on the back of the thyroid lobe.
- Level with the first tracheal ring, above the inferior thyroid artery.
Inferior Gland
- More variable in position, usually behind the lower pole.
- Below the inferior thyroid artery and lateral to the recurrent laryngeal nerve.
- Glands are not necessarily at the same level on each side.
Appearance and Identification
- Brownish-yellow in color to distinguish from thyroid tissue and fat.
- Sometimes embedded within the thyroid lobe.
- Follow branches of the inferior thyroid artery upwards and downwards.
- A small branch enters each gland.
Blood Supply
- Both upper and lower parathyroids are usually supplied by the inferior thyroid artery.
- Minute veins join thyroid vessels.
Lymph Drainage
- Same as the thyroid gland.
Nerve Supply
- Sympathetic vasoconstrictor fibers enter with the arteries.
Structure
- Homogeneous and very vascular.
- Composed of small, closely-packed chief or principal cells that secrete parathyroid hormone (PTH).
- Resembles lymphoid tissue but distinguished by numerous blood capillaries.
- Oxyphil cells are scattered among chief cells, derived from them, but their function is unknown.
Development
- The superior gland (parathyroid IV) develops from the dorsal diverticulum of the fourth pharyngeal pouch.
- The inferior gland (parathyroid III) develops from the third pouch but migrates caudally due to thymus descent.
- Inferior glands are more likely to end up in unusual positions due to longer migration than superior glands.
- About 10% of inferior glands are within the capsule of the thymus. Aberrant glands may be in the lower neck, posterior or anterior mediastinum.
Surgical Considerations
- For parathyroidectomy, the thyroid gland lobes are exposed and retracted forward and medially to inspect for parathyroids.
- Branches of the inferior thyroid artery are followed to locate the glands.
- Exposure of the thymus may be necessary.
- If all four glands are removed, part of one can be implanted into the brachioradialis muscle as an endocrine graft.
Trachea
- Extends from the larynx (attached to the cricoid cartilage by the cricotracheal ligament) into the thorax.
- Patency is maintained by C-shaped hyaline cartilages (rings) joined by a fibroelastic membrane.
- The posterior gap in the C-shaped rings is closed by the trachealis muscle.
- Has cervical and thoracic parts.
Length
- Total length is 10 cm (4 in), with 5 cm in the neck from the cricoid cartilage to the jugular notch.
- During deep inspiration, the total length may increase to 15 cm.
Cervical Part
- Lies in the midline of the neck, in contact with the front of the esophagus.
- The recurrent laryngeal nerve runs in the groove between the trachea and esophagus.
- The carotid sheath is to the side of the trachea.
- The isthmus of the thyroid gland is adherent to the 2nd, 3rd, and 4th tracheal rings, with lobes against the trachea down to the 6th ring.
- The inferior thyroid veins and anterior jugular venous arch lie in front.
- Also anterior are the thyroidea ima artery, levator glandulae thyroideae, and the upper end of a persistently large thymus (if present).
- The trachea passes downwards and backwards due to the shape of the lower cervical and upper thoracic vertebral column.
- Just below the skin at cricoid level but 2 cm or more deep to the front of the jugular notch.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.