Podcast
Questions and Answers
What is the primary function of the kidneys in the urinary system?
What is the primary function of the kidneys in the urinary system?
- To store urine until it is ready to be expelled
- To regulate blood pH by controlling hydrogen ion concentration (correct)
- To eliminate waste from the body through the urethra
- To carry urine from the kidneys to the bladder
What is the name of the hormone produced by the kidneys that stimulates red blood cell production?
What is the name of the hormone produced by the kidneys that stimulates red blood cell production?
- Vitamin D
- Erythropoietin (correct)
- Hydrogen ion
- Urea
What is the name of the tube that carries urine from the kidneys to the bladder?
What is the name of the tube that carries urine from the kidneys to the bladder?
- Urethra
- Bladder
- Ureters (correct)
- Kidney
What is the primary function of the bladder in the urinary system?
What is the primary function of the bladder in the urinary system?
What is the role of the kidneys in regulating blood volume and blood pressure?
What is the role of the kidneys in regulating blood volume and blood pressure?
What is the name of the process by which the body eliminates waste from the body?
What is the name of the process by which the body eliminates waste from the body?
What is the function of the urethra in the urinary system?
What is the function of the urethra in the urinary system?
What is the role of the kidneys in producing vitamin D?
What is the role of the kidneys in producing vitamin D?
Match the components of the urinary system with their functions:
Match the components of the urinary system with their functions:
Match the processes with the organs involved in the urinary system:
Match the processes with the organs involved in the urinary system:
Match the urinary system components with their interactions:
Match the urinary system components with their interactions:
Match the hormones with their functions in the urinary system:
Match the hormones with their functions in the urinary system:
Match the processes with their importance in the urinary system:
Match the processes with their importance in the urinary system:
Match the components of the urinary system with their importance:
Match the components of the urinary system with their importance:
Match the kidney structures with their functions:
Match the kidney structures with their functions:
Match the kidney components with their roles:
Match the kidney components with their roles:
Match the nephron components with their functions:
Match the nephron components with their functions:
Match the processes with the location where they occur in the nephron:
Match the processes with the location where they occur in the nephron:
Match the blood vessels with their functions in the kidney:
Match the blood vessels with their functions in the kidney:
Match the nephron structures with their relationships:
Match the nephron structures with their relationships:
Match the kidney processes with their purposes:
Match the kidney processes with their purposes:
Match the kidney components with their characteristics:
Match the kidney components with their characteristics:
Match the kidney processes with their importance:
Match the kidney processes with their importance:
What is the primary function of the kidneys in the body?
What is the primary function of the kidneys in the body?
Which part of the nephron is responsible for filtration?
Which part of the nephron is responsible for filtration?
How many nephrons are approximately present in each kidney?
How many nephrons are approximately present in each kidney?
What is the name of the vessel that carries blood that needs to be filtered and modified into the kidney?
What is the name of the vessel that carries blood that needs to be filtered and modified into the kidney?
Where does reabsorption occur in the nephron?
Where does reabsorption occur in the nephron?
What is the function of the efferent arteriole in the nephron?
What is the function of the efferent arteriole in the nephron?
What is the purpose of the peritubular capillaries in the nephron?
What is the purpose of the peritubular capillaries in the nephron?
What is the name of the vessel that carries filtered blood out of the kidney?
What is the name of the vessel that carries filtered blood out of the kidney?
What is the functional unit of the kidney?
What is the functional unit of the kidney?
What are the three main processes that occur in the nephron?
What are the three main processes that occur in the nephron?
What percentage of water, ions, glucose, urea, and other substances is forced out of the blood during glomerular filtration?
What percentage of water, ions, glucose, urea, and other substances is forced out of the blood during glomerular filtration?
What is the purpose of the filtration barrier in the glomerulus?
What is the purpose of the filtration barrier in the glomerulus?
What is the role of podocytes in the glomerulus?
What is the role of podocytes in the glomerulus?
What is the result of the afferent arteriole having a larger diameter than the efferent arteriole?
What is the result of the afferent arteriole having a larger diameter than the efferent arteriole?
What is the significance of glomerular filtration rate (GFR) in the kidneys?
What is the significance of glomerular filtration rate (GFR) in the kidneys?
What is dependent on blood pressure and the need to retain or remove fluid volume?
What is dependent on blood pressure and the need to retain or remove fluid volume?
What is the purpose of regulating the diameter of the afferent arteriole?
What is the purpose of regulating the diameter of the afferent arteriole?
What is the direction of fluid flow in the glomerulus?
What is the direction of fluid flow in the glomerulus?
What is the role of hydrostatic pressure in glomerular filtration?
What is the role of hydrostatic pressure in glomerular filtration?
What is the result of the filtration barrier in the glomerulus?
What is the result of the filtration barrier in the glomerulus?
Match the following components of the glomerulus with their functions:
Match the following components of the glomerulus with their functions:
Match the following with their roles in regulating glomerular filtration rate (GFR):
Match the following with their roles in regulating glomerular filtration rate (GFR):
Match the following with their characteristics in the glomerulus:
Match the following with their characteristics in the glomerulus:
Match the following with their effects on glomerular filtration:
Match the following with their effects on glomerular filtration:
Match the following with their roles in the urinary system:
Match the following with their roles in the urinary system:
Match the following with their effects on the filtration barrier:
Match the following with their effects on the filtration barrier:
Match the following with their roles in the nephron:
Match the following with their roles in the nephron:
Match the following with their characteristics in glomerular filtration:
Match the following with their characteristics in glomerular filtration:
What percentage of water is reabsorbed in the proximal convoluted tubule?
What percentage of water is reabsorbed in the proximal convoluted tubule?
What happens when glucose is not reabsorbed into the bloodstream?
What happens when glucose is not reabsorbed into the bloodstream?
What is the minimum plasma concentration of a substance that will result in its excretion in the urine?
What is the minimum plasma concentration of a substance that will result in its excretion in the urine?
Which of the following is NOT reabsorbed in the proximal convoluted tubule?
Which of the following is NOT reabsorbed in the proximal convoluted tubule?
What is the function of the proximal convoluted tubule in the nephron?
What is the function of the proximal convoluted tubule in the nephron?
How much blood is filtered by the kidneys daily?
How much blood is filtered by the kidneys daily?
What is the result of high glucose levels in the blood?
What is the result of high glucose levels in the blood?
What is the role of glucose in the urinary system?
What is the role of glucose in the urinary system?
How much urine is produced daily by the kidneys?
How much urine is produced daily by the kidneys?
Match the following kidney processes with their importance in the urinary system:
Match the following kidney processes with their importance in the urinary system:
Match the components of the nephron with their functions:
Match the components of the nephron with their functions:
Match the terms with their definitions in the urinary system:
Match the terms with their definitions in the urinary system:
Match the kidney structures with their functions in the urinary system:
Match the kidney structures with their functions in the urinary system:
What is the primary function of the loop of Henle in the nephron?
What is the primary function of the loop of Henle in the nephron?
Which hormone regulates the amount of water reabsorbed from the collecting duct as it passes through the medulla?
Which hormone regulates the amount of water reabsorbed from the collecting duct as it passes through the medulla?
What is the significance of the loop of Henle being longer in desert animals like the kangaroo rat?
What is the significance of the loop of Henle being longer in desert animals like the kangaroo rat?
What is the direction of water flow in the descending loop of Henle?
What is the direction of water flow in the descending loop of Henle?
What is the effect of the accumulation of salt in the interstitial fluid in the loop of Henle?
What is the effect of the accumulation of salt in the interstitial fluid in the loop of Henle?
What is the adaptation that allows the kangaroo rat to conserve water more efficiently?
What is the adaptation that allows the kangaroo rat to conserve water more efficiently?
What is the direction of salt movement in the ascending limb of the loop of Henle?
What is the direction of salt movement in the ascending limb of the loop of Henle?
Match the structures of the loop of Henle with their permeability characteristics:
Match the structures of the loop of Henle with their permeability characteristics:
Match the following nephron structures with their functions:
Match the following nephron structures with their functions:
Match the components of the nephron with their functions in the loop of Henle:
Match the components of the nephron with their functions in the loop of Henle:
Match the characteristics of the medulla with their effects on the kidney:
Match the characteristics of the medulla with their effects on the kidney:
Match the following substances with their reabsorption rates in the nephron:
Match the following substances with their reabsorption rates in the nephron:
Match the following hormones with their functions in the nephron:
Match the following hormones with their functions in the nephron:
Match the components of the nephron with their functions in water reabsorption:
Match the components of the nephron with their functions in water reabsorption:
What is the primary function of the kidneys in regulating electrolyte balance?
What is the primary function of the kidneys in regulating electrolyte balance?
What happens when the body becomes too acidic (acidosis)?
What happens when the body becomes too acidic (acidosis)?
In which part of the nephron does reabsorption of glucose, amino acids, and salts occur?
In which part of the nephron does reabsorption of glucose, amino acids, and salts occur?
What is the result of the loop of Henle creating a hyperosmotic medulla?
What is the result of the loop of Henle creating a hyperosmotic medulla?
What is the function of the kidneys in regulating blood pH?
What is the function of the kidneys in regulating blood pH?
What is the function of the ascending limb of the loop of Henle?
What is the function of the ascending limb of the loop of Henle?
What is the result of the kidneys regulating electrolyte levels?
What is the result of the kidneys regulating electrolyte levels?
What is the function of the descending limb of the loop of Henle?
What is the function of the descending limb of the loop of Henle?
What is the role of hormones in the distal convoluted tubule and collecting duct?
What is the role of hormones in the distal convoluted tubule and collecting duct?
Match the kidney structures with their primary functions:
Match the kidney structures with their primary functions:
Match the kidney regions with their permeability characteristics:
Match the kidney regions with their permeability characteristics:
Match the kidney processes with their purposes:
Match the kidney processes with their purposes:
Match the kidney components with their relationships:
Match the kidney components with their relationships:
Match the kidney regions with their functions in the urinary system:
Match the kidney regions with their functions in the urinary system:
Match the kidney processes with their effects on the body:
Match the kidney processes with their effects on the body:
Match the kidney structures with their roles in regulating blood pH:
Match the kidney structures with their roles in regulating blood pH:
What triggers the release of ADH?
What triggers the release of ADH?
What is the primary function of ADH in the kidney?
What is the primary function of ADH in the kidney?
What is the effect of ADH on blood vessels?
What is the effect of ADH on blood vessels?
What is the significance of the hyperosmotic medulla in the kidney?
What is the significance of the hyperosmotic medulla in the kidney?
What is the effect of chronic elevation of blood pressure due to ADH?
What is the effect of chronic elevation of blood pressure due to ADH?
What is the target of ADH in the kidney?
What is the target of ADH in the kidney?
What is the result of increased blood volume due to ADH?
What is the result of increased blood volume due to ADH?
What is another name for ADH?
What is another name for ADH?
Match the following structures with their functions in the regulation of ADH:
Match the following structures with their functions in the regulation of ADH:
Match the following effects with the location where they occur in the kidney:
Match the following effects with the location where they occur in the kidney:
Match the following terms with their definitions related to ADH:
Match the following terms with their definitions related to ADH:
Match the following with their roles in the regulation of blood water levels:
Match the following with their roles in the regulation of blood water levels:
Match the following with their effects on the body:
Match the following with their effects on the body:
Match the following structures with their functions in the kidney:
Match the following structures with their functions in the kidney:
Match the following with their effects on the kidney:
Match the following with their effects on the kidney:
What type of hormone is aldosterone?
What type of hormone is aldosterone?
What stimulates the adrenal cortex to release aldosterone?
What stimulates the adrenal cortex to release aldosterone?
What is the effect of aldosterone on potassium levels in the blood?
What is the effect of aldosterone on potassium levels in the blood?
What is the response to a drop in blood volume and blood pressure?
What is the response to a drop in blood volume and blood pressure?
What is the result of aldosterone's action on the kidney?
What is the result of aldosterone's action on the kidney?
What triggers the release of aldosterone in response to elevated potassium levels in the blood?
What triggers the release of aldosterone in response to elevated potassium levels in the blood?
What system does aldosterone play a role in?
What system does aldosterone play a role in?
What is the effect of aldosterone on blood volume and blood pressure?
What is the effect of aldosterone on blood volume and blood pressure?
Match the hormones with their effects on blood volume and blood pressure:
Match the hormones with their effects on blood volume and blood pressure:
Match the components of the renin-angiotensin-aldosterone system with their functions:
Match the components of the renin-angiotensin-aldosterone system with their functions:
Match the triggers with their corresponding responses in the renin-angiotensin-aldosterone system:
Match the triggers with their corresponding responses in the renin-angiotensin-aldosterone system:
Match the components of the renin-angiotensin-aldosterone system with their sites of production:
Match the components of the renin-angiotensin-aldosterone system with their sites of production:
Match the effects of the renin-angiotensin-aldosterone system on blood pressure with their corresponding mechanisms:
Match the effects of the renin-angiotensin-aldosterone system on blood pressure with their corresponding mechanisms:
Flashcards are hidden until you start studying
Study Notes
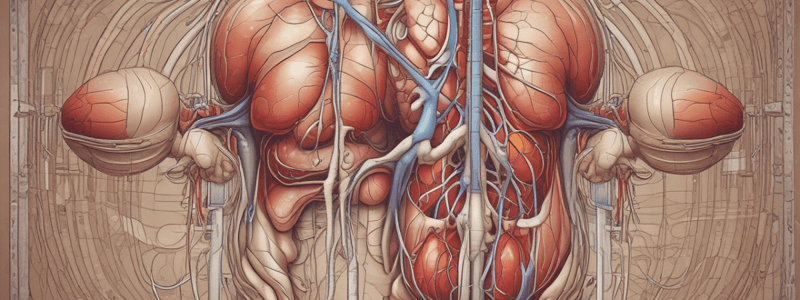
- The urinary system, also known as the renal system, is part of the excretory system, working together with the skin, respiratory system, and digestive system to eliminate waste from the body.
- The urinary system consists of the kidneys, ureters, bladder, and urethra, with the kidneys being located in the back area and the ureters carrying urine from the kidneys to the bladder.
- The bladder, also known as the urinary bladder, stores urine until it is ready to be expelled, and smooth muscles allow the urine to leave the body through the urethra during urination.
- The kidneys play a major role in filtering the blood, removing waste products such as urea, maintaining water and salt balance, regulating ion concentrations, and producing urine.
- The kidneys regulate blood pH by controlling hydrogen ion concentration, and they also help regulate blood volume and blood pressure by getting rid of excess water or retaining it when necessary.
- The kidneys function as an endocrine tissue, producing erythropoietin (EPO), a hormone that stimulates red blood cell production, and they are responsible for producing the active form of vitamin D, which is essential for calcium regulation and bone health.
- The kidneys are involved in all functions of the urinary system except for the excretion part, which is accomplished through the urethra.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.