Podcast
Questions and Answers
Which statement best describes the composition of tendons and ligaments?
Which statement best describes the composition of tendons and ligaments?
- They are collagenous tissues with relatively few cells and an abundant extracellular matrix (ECM). (correct)
- They are composed mainly of minerals, providing rigidity and compressive strength.
- They consist of a high density of cells actively dividing to provide tensile strength.
- They are primarily composed of elastin, allowing for high degrees of flexibility.
What is the primary biomechanical function of the endotendon?
What is the primary biomechanical function of the endotendon?
- Resisting longitudinal stress generated by muscle and ground reaction force
- Providing microvasculature to the entire tendon structure
- Packing fascicles together and being continuous with the epitenon
- Organizing and holding fibers in a linear direction to form fascicles (correct)
How does synovial fluid contribute to tendon healing?
How does synovial fluid contribute to tendon healing?
- It promotes mineralization of the tendon matrix.
- It provides the primary vascular perfusion necessary for nutrient supply.
- It directly stimulates the synthesis of elastin fibers.
- It serves as a nutrient source when vascular perfusion is limited. (correct)
Why is early motion important in tendon repair?
Why is early motion important in tendon repair?
Which factor primarily determines the extent of injury to a tendon under excessive loading?
Which factor primarily determines the extent of injury to a tendon under excessive loading?
What is passive insufficiency in the context of muscle biomechanics?
What is passive insufficiency in the context of muscle biomechanics?
Which of the following is a critical factor that determines fatigue failure in biological materials?
Which of the following is a critical factor that determines fatigue failure in biological materials?
How does increased temperature generally affect the stiffness of biological tissues?
How does increased temperature generally affect the stiffness of biological tissues?
What characterizes cyclic loading in the context of tissue biomechanics?
What characterizes cyclic loading in the context of tissue biomechanics?
Why are biological materials, like living tissues, able to withstand degradation from excessive loading better than non-biological materials?
Why are biological materials, like living tissues, able to withstand degradation from excessive loading better than non-biological materials?
What is the best definition of 'strain' in the context of bone strain injuries?
What is the best definition of 'strain' in the context of bone strain injuries?
Which characteristic is associated with the 'severe' stage of a bone stress injury (BSI)?
Which characteristic is associated with the 'severe' stage of a bone stress injury (BSI)?
How is Grade V spondylolisthesis characterized?
How is Grade V spondylolisthesis characterized?
Which of the following is characteristic of ankylosing spondylitis?
Which of the following is characteristic of ankylosing spondylitis?
Which condition is most likely indicated by areflexic bladder, bowel, and saddle paresthesia?
Which condition is most likely indicated by areflexic bladder, bowel, and saddle paresthesia?
How do facet joints guide intervertebral motion?
How do facet joints guide intervertebral motion?
Which of the following is a typical characteristic of thoracic vertebrae?
Which of the following is a typical characteristic of thoracic vertebrae?
What is the primary function of the anterior cruciate ligament (ACL)?
What is the primary function of the anterior cruciate ligament (ACL)?
Why are females more prone to ACL injuries compared to males?
Why are females more prone to ACL injuries compared to males?
What is typically the primary method of rehabilitation after ACL reconstruction?
What is typically the primary method of rehabilitation after ACL reconstruction?
A direct blow to the anterior tibia is most likely to cause injury to which ligament?
A direct blow to the anterior tibia is most likely to cause injury to which ligament?
At what degree of knee flexion does the posterolateral corner provide primary stability to external rotation?
At what degree of knee flexion does the posterolateral corner provide primary stability to external rotation?
What is the primary function of the superficial band of the Medial Collateral Ligament?
What is the primary function of the superficial band of the Medial Collateral Ligament?
Why are the majority of the menisci avascular?
Why are the majority of the menisci avascular?
Flashcards
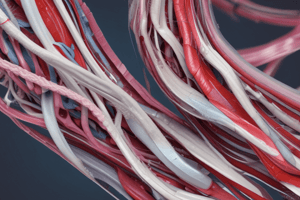
Tendons & Ligaments
Tendons & Ligaments
Parallel-fibered collagenous tissues that connect muscle to bone and bone to bone, respectively.
Collagen Type in Tendons/Ligaments
Collagen Type in Tendons/Ligaments
Type I, best suited for resisting tensile loads.
Tendon/Ligament Composition
Tendon/Ligament Composition
Relatively few cells (fibroblasts mature into fibrocytes) & an abundant ECM. 20% cellular, 80% ECM (70% water, 30% solids).
Tendon Structure
Tendon Structure
Signup and view all the flashcards
Endotendon Function
Endotendon Function
Signup and view all the flashcards
Epitenon Role
Epitenon Role
Signup and view all the flashcards
Nonvascular Nutrient Source for new collagen synthesis
Nonvascular Nutrient Source for new collagen synthesis
Signup and view all the flashcards
Passive Insufficiency
Passive Insufficiency
Signup and view all the flashcards
Passive Insufficiency (definition)
Passive Insufficiency (definition)
Signup and view all the flashcards
Wrist Grip & Insufficiency
Wrist Grip & Insufficiency
Signup and view all the flashcards
Fatigue Determinants
Fatigue Determinants
Signup and view all the flashcards
Loading Rate Effect
Loading Rate Effect
Signup and view all the flashcards
Cyclic Loading Fatigue
Cyclic Loading Fatigue
Signup and view all the flashcards
Temperature & Stiffness
Temperature & Stiffness
Signup and view all the flashcards
Bone Strain Injury
Bone Strain Injury
Signup and view all the flashcards
Bone Stress Injury
Bone Stress Injury
Signup and view all the flashcards
BSI Stages
BSI Stages
Signup and view all the flashcards
Spondylolisthesis
Spondylolisthesis
Signup and view all the flashcards
Spondylolysis
Spondylolysis
Signup and view all the flashcards
Spondylitis
Spondylitis
Signup and view all the flashcards
Ankylosing Spondylitis
Ankylosing Spondylitis
Signup and view all the flashcards
Cauda Equina Syndrome
Cauda Equina Syndrome
Signup and view all the flashcards
ACL Function
ACL Function
Signup and view all the flashcards
ACL Injury Risk Factor
ACL Injury Risk Factor
Signup and view all the flashcards
Post-op ACL training
Post-op ACL training
Signup and view all the flashcards
Study Notes
Biomechanics of Tendons and Ligaments
- Tendons and ligaments are composed of parallel-fibered collagenous tissues, specifically type I collagen, optimized for resisting tensile loads.
- Collagen is a fibrous protein that makes up roughly half of the total protein in the human body.
Fiber Alignment
- Tendons feature parallel bundles of collagen fibers, while ligaments consist of nearly parallel bundles.
Composition and Structure
- Tendons and ligaments are primarily composed of few cells known as fibroblasts that mature into fibrocytes with an abundance of ECM.
- Fibroblasts actively produce components of the tissue.
- Fibrocytes maintain and repair the tissue.
- The composition is about 20% cellular material and 80% extracellular matrix (ECM)
- ECM consists of about 70% water and 30% solids like collagen, elastin, and ground substance.
Tendon Structure and Composition
- Tendons are biomechanically designed to resist longitudinal stress from muscle activity and ground reaction force (GRF).
- Chains of tropocollagen are arranged longitudinally and unite into fibers.
- The endotendon organizes and holds fibers linearly, forming fascicles.
- The epitenon packs fascicles continuously with the endotendon and microvasculature.
Mechanical Behavior
- Tendons and ligaments resist primarily tensile loads during normal activities.
- Injury occurs when there is excessive or abnormal loading.
- Trauma severity depends on tendon quality, rate of impact, load magnitude, and integrity of supporting structures.
Tendon Healing
- Tendons can intrinsically synthesize new collagen fibrils.
- They rely on synovial fluid diffusion for nutrients, beyond vascular perfusion.
- Early tendon gliding facilitates healing, indicating motion programs are crucial for recovery.
- Motion critically promotes tendon repair.
Passive Insufficiency of Muscle
- Passive insufficiency occurs in multi-joint muscles when the antagonist's length is insufficient for the full elongation of the stretched muscle group over all joints simultaneously.
- Hip flexion can reach ~125° with a flexed knee, but is limited to ~70° with an extended knee due to hamstring insufficiency.
- Passive insufficiency occurs when a biarticular muscle, like the hamstring, is stretched too much across both joints, limiting movement because the muscle can no longer lengthen.
Wrist Grip and Insufficiency
- Maximum grip strength is greatest when the wrist is slightly extended.
- Grip strength diminishes when the wrist is flexed.
- Reduced grip during full flexion combines active insufficiency of finger flexors and passive insufficiency of the antagonistic finger extensor.
Fatigue Failure in Biological Material
- Fatigue is influenced by the magnitude of applied loads measured by loading rate.
- Most substances are stiffer at higher loading rates; loading quickly makes failure less likely.
- Fatigue is also determined by the number of load repetitions on that structure over time.
- Cyclic loading where the rate exceeds the tissue's adaptive capacity results in failure.
- Temperature impacts fatigue; most substances are less stiff at higher temperatures.
Biological Materials and Fatigue
- Living biological tissues can adapt and regenerate over a varying extent.
- This regeneration counteracts the degradative effects of excessive loading.
- Examples of causes of fatigue failure are stress fractures and soft-tissue overuse syndromes.
- Fatigue failure/biological failure is indicated by overuse or cumulative trauma.
- It depends on the load magnitude and number of repetitions.
- Loading rate increases stiffness, leading to less deformation before failure.
- Cyclic loading reduces the capacity to adapt and leads to fatigue failure.
- Increased temperature reduces stiffness, causing greater deformation before failure.
- Self-repair can counteract the negative effects of excessive loading.
Bone Strain Injuries
- Bone strain injuries involve damage from excessive deformation due to external forces, often from high force causing microdamage.
- Strain is the bone's deformation, contributing to stress injuries over time.
Mechanical Concept of Bone
- Mechanical concept is how much a bone deforms under force.
- Bone Stress Injury (BSI) is a progressive overuse injury from repetitive loading that exceeds the bone's ability to self-repair.
Stages of Bone Injury
- BSI occurs from repetitive stress from activities like running or jumping.
- Stages include mild bone stress reaction and severe stress fracture, resulting in clinical damage.
- Shin splints can progress to tibial stress fractures.
- Important to understand that amount of stretch in a bone is strain while how often the bone is stretched to cause weakening/breaking/damage is stress.
Spondylolisthesis
- Spondylolisthesis involves anterior subluxation of one vertebra over another, often between L4 and L5.
- It can be traumatic or degenerative, with 70% of patients experiencing lower back pain.
- The Meyerding method grades it from I (0-25%) to V (>100%, spondyloptosis).
Spondylolysis
- Spondylolysis is a stress fracture of the pars interarticularis, known as a "Scotty dog" fracture, typically due to trauma.
Spondylosis
- Spondylosis is arthritis of the spine, typically from wear and tear in IVD and other regional structures.
Spondylitis
- Spondylitis is the inflammation of vertebrae.
- This is one of the most common causes of neck and back pain.
- Spondylitis results from inflammation of vertebral joints and may go undetected until fully developed.
Ankylosing Spondylitis
- Ankylosing spondylitis is a chronic inflammatory disease, causing axial arthritis and initial low back pain, eventually impairing the spine and sacroiliac joint mobility.
- Fusion occurs with the HLA-B27 gene typically in men in their 20s-30s.
- Bilateral sacroiliitis is a telltale feature, causing pain at rest in the sacrum and iliac spine.
- A diagnostic biological hallmark is the observation of "bamboo spine"
Central Stenosis
- Central stenosis typically occurs in the 4th decade of life
- It is characterized by pain worsened by spinal extension and relieved by rest.
Cauda Equina Syndrome
- Cauda equina syndrome involves areflexic bladder/bowel and saddle paresthesia in lower limbs.
- A common cause of Cauda Equina Syndrome is massive midline disc herniation below L1.
- The cauda equina itself is the collection of nerve roots at the end of the vertebral canal.
Spinal Infections
- Spinal infections are caused by UTIs, skin abscesses, indwelling catheters, or IV drug use.
- Presentation involves dull, continuous back pain and low-grade fever.
- A hallmark finding is epidural abscess.
Intervertebral Foraminal Stenosis
- Intervertebral foramen is where nerves enter/exit the spinal cord.
- Its size is dictated by the disc height.
- Foraminal stenosis results from osteophyte formation and ligament hypertrophy.
Facet Arthropathy
- Spondylitis is associated with spondylodiscitis, spondyloarthritides, facet arthropathy, local muscle pain, and guarding.
Facet Joints
- The facet joints guide intervertebral motion.
- Their articular surfaces are covered by hyaline cartilage and enveloped by a loose fibrous capsule.
- Cervical spine facets are directed superoposteriorly (superior) and inferoanteriorly (inferior), with oblique-placed facets being nearly horizontal.
- Thoracic spine facets are nearly vertical, with superior facets directed posteriorly and inferior facets anteriorly. Typical thoracic vertebrae bear superior and inferior half facets.
- Lumbar spine facets have nearly vertical facets directed posteromedially (superior) and anterolaterally (inferior).
Cruciate Ligaments of the Knee
- The ACL originates on the lateral femoral condyle and inserts on the tibia eminences. It prevents anterior translation of the tibia on the femur while limiting internal and external rotation, especially in extension.
- The ACL's anteromedial bundle is tight in flexion, and a posterolateral bundle is tight in extension
- Females are more susceptible to ACL tears.
- ACL injuries can occur because women have a anatomically smaller ligament with a narrow notch width, decreased protective role of knee dynamic stabilizers, hormonal influences, and landing mechanics. This is proven, as women are 2-6x more likely to tear them.
- Most ACL tears (70%) are non-contact injuries.
Diagnostic findings
- Diagnostic findings show stenosis of the notch or tibial avulsion fracture.
- A Segond fracture may be pathognomonic for ACL tear.
ACL Reconstruction
- Indications include active individuals with acute tears, instability despite modification, or repairable meniscus tear.
- Graft sources include autografts and allografts.
- Primary method of training post-op is closed-chain exercises.
PCL Overview
- The PCL is the knee's primary static stabilizer, resisting posterior tibial translation though not isometric during flexion.
- The PCL's AL bundle tightens in flexion, and a PM bundle tightens in extension.
- PCL injuries typically occur from contact, mechanisms can include direct blow to the anterior tibia, hyperflexion, or hyperextension.
- Goals for Rehab are restoring quadriceps strength so that Athletes can return to their previous level of activity.
- In the long term medial compartment and patellofemoral degeneration may occur.
Collateral Ligaments
- The LCL forms the posterolateral corner, stabilizing external rotation at 30°.
- LCL structures include the LCL, popliteus complex, fabellar ligament, and arcuate ligament.
- Instability can be assessed via dial test and could be increased with high tibial external rotation.
- Layer I includes the IT band and biceps femoris whereas Layer III has the LCL, arcuate ligament, fabellar ligament, and lateral capsular ligament
- Primary injury mechanism is varus force indicated when there;s an avulsion of proximal fibula.
- Treatment of isolated LCL injuries will commonly be non-operative for grade 1 or 2 and treated with a primary or reconstruction for grade 3 injurie
MCL of the Knee
- The superficial band of the MCL is a primary stabilizer against valgus stress and has three main stabilizing layers: Tensor fasciae, Sartorius tendon (Layer I), Superficial MCL, Posterior oblique (Layer II) and Deep MCL, Knee capsule (Layer III).
- Its injury mechanism is a valgus force to a flexed weight-bearing knee.
- Instability can be assessed with valgus stress and may be calcified (Pelligrini-Steida lesion).
Collateral Ligament Laxity - Injuries
- Laxity in full extension implies complete collateral tear and injury to secondary varus/valgus restraints
- Injuries include ACL and PCL
Meniscus Injury
- Meniscus injury is more painful than ACL injury, commonly injuring the medial meniscus due to its less mobility.
- Fractures are the shock absorption, load transmission, stabilization, lubrication, and proprioception.
- Diagnosis using MRI is common.
- Harmful effects are increases to local contact stress as the menisci may need to be removed.
- Surgeries like menisectomies is contraindicated; increasing local stress on the other tissues.
Vascularity
- The majority of menisci are avascular, with only the outer 3mm being perfused and the inner 1/3rd receiving no blood.
Exams to Examine Knee Ligaments
- Lachman tests measure sensitive tests for ACL tears and show amount of anterior translation.
- Pivot shift tests looks for "screw home" mechanism of the tibia
- Anterior Drawer looks at how much anterior translation of the tibia exhibits when flexed at 90 degrees
- Posterior drawer test most sensitive for PCL tear.
Knee Biomechanics
- "Screw home" mechanism describes how the medial tibia externally rotates 5° in the last 15° of extension and allows knee to lock in extension and decrease quadriceps work.
- Rollback mechanism describes how the center of rotation translates posteriorly during flexion allowing increased flexion without impingement.
Femur
- Trabecular Pattern is based on Wolffs law, which adapts to mechanical stress and load distribution. In other words, the bone grows stronger when subjected to stress.
Hip Surgery and Treatment
- Disadvantage of Surgical Hip Dislocation is Residual abductor weakness. Surgery to deal with it includes trochanteric osteotomy from the lateral part, preserving the blood supply
- Advantage is 360 degree access to joint
- Trocanteric-pelvic impingement is caused by one of the three locations of extra-articular hip impingement, namely Subspine, Ischiofemoral, Trochanteric-pelvc.
Occurrences
- AIs occurs typically to young athletes due to sudden muscle contractions.
Labral Tear
- Labral tears affect the hip joint due to: Hypertrophic (seen in dysplasia) or hypotrophic labrum, Focal chondral defects, or Avascular necrosis with its Femoroacetabular.
Abductors
- Forces acting on the hip joint are: body weight, GRF, and adbuctor.
Impingements
- CAM Lession is the cause of femoroacetabular impingement.
Ligaments, Function
- Ligamentum Teres connects head to acetab, isn't stabilizer, supplies blood.
- Ischiofemoral ligament restricts internal rotation and controls flexion and extension.
- Iliofemoral and pubofemoral control rotation and have biomechanical functions.
Acetabulum Function
- Acetabulum is made by joining the ilium, ischium, & pubis and is ONLY part of the body where triradiate cartilage is found.
- Contact pressure affects the shape of the femoral head. Abnormal contact leads to hip dysplasia.
- Central, cartliage, Labrum = 3 main function, protects (contact.cartliage)by limiting. Controls.(seal .Stability)Effect 3 components
- Forces of hip = joint reaction forces ( lateral , decrrasing hip). Development
- The acetabulum is a concave socket of the hip joint that articulates with the femoral and and has Ossification Centers
- the hip joint can be lateralized (increasing forces w/increased moment)
Orthotics
- Plastozaote: closed cell, polye foam and developed by Paull brand for neuropathy of feet due to ulcers.
- Orthotics Durometer: 1-20 pink, 2-36 white, 3-69 BLACK
- Polyurethane: is open cell foam, cant heat to mold due to Dr. Scholls non foam thermoset.
- Polye/Double Carbon, Polyproplye/Triple (Pvc)
- Vinyl/Poly Chlroide Pvc = used in foot. CArbon graphlite ( make foot 0rthose) is used to to strentheth with minimul thickkness( prime goal). Material include carbon graphitle, pellets.
Latex- Natural Rubber
- Created to with Vulcanizatio. Also, Neorene/ Synthic Ruber (dureprene/ dupon)
- Ethinyl- Vinal -Acetate = EVA(pelite or NIkelplait ) all Thero forming.
- Cork - Bark Of Oak Tree - Korex- sheet LATEX - Thermo cork.
Ground and ground reaction forces
- The force of the ground on the body during ambulation (walking), has external and internal factors.
- GRFV is opposite oriented relative to the torce gravity, in stance gravity passes front the ankle creating Closed Chain
- GRFV- HEIKE, flat, Midstance, heel
Anke injuries
- Deltoid Tear/ Ruptre, mallor fractuer
Talorcurl OCD
- Ankle is less sensativative (less trauma)
Ankle Joint
- Joint. forms linkge-transferes ground contact
Distil Tibialfular Joint
- Moves 1-2 mil (df and af
Ankel
- Medial Ankle Ligment + Very storng. Lateral+ATFL for Inversion
A&P Tibulus
TA,EHL = Antrior. helps.
Motion of Tibulus
Medial =Evert lateral - invertered
Tibula
The movements affects the tibia and allows the fibula to move superiorly with DF and inferiorly/PF . This allows Fibular Head to move anteriorly with dorsiflexion/eversion.
Dorsiflexion and Rotations
-
A decrease PTFJ (Proxmall, and it causes limitions DF or it may limit of ankle ROM), DF+Torsion
-
Tibilar Rotato= affects the rotation in both Directions, internally and externally.
-
The muscles. = Provide, Stababiloty,
-
Promeus = Anker,
-
When STJ pronates, these actions occur: Calcaneus Valgus, talluss adds, Tibial rotation medial. When supinate
-
TA are the antier of the lower helps to (df, and inversion) and clear, phase ecc. Ehl Extensors (df =invert)
-
Osteokinema=The Tiblis Anterior. Helps and the Enkels lower phases by and (DF. Subterl)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.