Podcast
Questions and Answers
What is the primary function of the upper esophageal sphincter?
What is the primary function of the upper esophageal sphincter?
- To prevent the backflow of food from the stomach into the esophagus
- To control the flow of acid from the stomach back into the esophagus
- To control the flow of food from the esophagus into the stomach
- To allow the passage of food from the pharynx into the esophagus (correct)
What is the approximate volume of the empty human stomach?
What is the approximate volume of the empty human stomach?
- Half the size of your fist (correct)
- 4 liters
- 1 liter
- 2 liters
Which type of cell in the gastric glands is responsible for secreting hydrochloric acid?
Which type of cell in the gastric glands is responsible for secreting hydrochloric acid?
- Mucous neck cells
- Chief cells
- Parietal cells (correct)
- Enteroendocrine cells
What is the purpose of the lower esophageal sphincter?
What is the purpose of the lower esophageal sphincter?
What is the name of the final phase of the swallowing process?
What is the name of the final phase of the swallowing process?
What is the purpose of the oblique muscle layer in the stomach?
What is the purpose of the oblique muscle layer in the stomach?
What is the main purpose of the regulatory mechanisms in the digestive system?
What is the main purpose of the regulatory mechanisms in the digestive system?
What is the primary purpose of the short reflex in the digestive system?
What is the primary purpose of the short reflex in the digestive system?
Which hormone is responsible for stimulating the release of gastric acid?
Which hormone is responsible for stimulating the release of gastric acid?
What is the primary function of the tongue in the digestive system?
What is the primary function of the tongue in the digestive system?
What is the purpose of the soft palate and the uvula in the digestive system?
What is the purpose of the soft palate and the uvula in the digestive system?
What is the main function of the long reflex in the digestive system?
What is the main function of the long reflex in the digestive system?
What is the main function of the hepatocytes in the liver?
What is the main function of the hepatocytes in the liver?
Which organ is responsible for storing extra bile?
Which organ is responsible for storing extra bile?
What can happen if feces are delayed in the colon for too long?
What can happen if feces are delayed in the colon for too long?
Which nutrient breakdown process in the small intestine is comparable to the action of dish soap on fats in water?
Which nutrient breakdown process in the small intestine is comparable to the action of dish soap on fats in water?
What is the role of the Valsalva maneuver in the process of defecation?
What is the role of the Valsalva maneuver in the process of defecation?
What is the primary function of the pancreas in digestion?
What is the primary function of the pancreas in digestion?
Which layer of the stomach wall is the most superficial and only present in the region inside the abdominal cavity?
Which layer of the stomach wall is the most superficial and only present in the region inside the abdominal cavity?
What is the primary function of the enteric nervous system?
What is the primary function of the enteric nervous system?
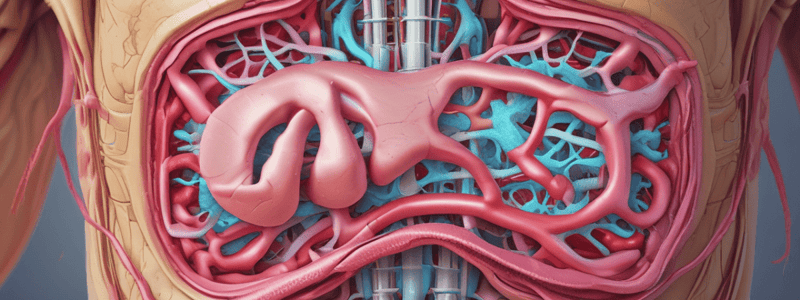
What is the function of the hepatic portal system?
What is the function of the hepatic portal system?
Which of the following statements about the peritoneum is correct?
Which of the following statements about the peritoneum is correct?
What is the primary function of the mouth in the digestive process?
What is the primary function of the mouth in the digestive process?
What percentage of the blood pumped by the heart enters the arteries serving the intestines during resting and digesting states?
What percentage of the blood pumped by the heart enters the arteries serving the intestines during resting and digesting states?
What is the rate of peristaltic contractions in the duodenum compared to the ileum?
What is the rate of peristaltic contractions in the duodenum compared to the ileum?
Which of the following statements about lipid digestion is true?
Which of the following statements about lipid digestion is true?
What is the primary function of the cecum in the large intestine?
What is the primary function of the cecum in the large intestine?
What is the primary function of the bacterial flora in the large intestine?
What is the primary function of the bacterial flora in the large intestine?
What is the primary function of the rectum in the large intestine?
What is the primary function of the rectum in the large intestine?
What is the primary function of the mass movements in the large intestine?
What is the primary function of the mass movements in the large intestine?
Flashcards are hidden until you start studying
Study Notes
Digestive System Overview
- Chemical digestion breaks down complex food molecules into their building blocks (water, acid, enzymes, and salts)
- Absorption primarily occurs in the small intestine, where nutrients are taken into the bloodstream or lipids into the lymphatic system
- Defecation removes undigested materials from the body
Regulatory Mechanisms
- Neural control: sensors in the stomach monitor expansion, food particle breakdown, liquid presence, and nutrient type, and can activate glands and muscle
- Two types of reflexes: short reflex (local stimulus and response) and long reflex (ANS and CNS reacting to stimuli outside the digestive tract)
- Hormonal control: gastrin stimulates gastric acid release, secretin stimulates bicarbonate release from the pancreas, CCK stimulates pancreatic enzyme and bile secretion, and gastric inhibitory peptide inhibits gastric secretion and slows gastric emptying and motility
Mouth, Pharynx, and Esophagus
- Mouth: oral cavity lined by cheeks, tongue, lips, and palate, capable of handling digestion and respiration simultaneously
- Tongue: involved in ingestion, mechanical and chemical digestion, swallowing, and vocalization
- Pharynx: propels food to the esophagus and lubricates food and passage
- Esophagus: propels food to the stomach, with upper and lower esophageal sphincters controlling food entry and acid reflux
Nerve Supply
- Enteric nervous system: runs from esophagus to anus, separated into myenteric and submucosal plexuses, responsible for motility and regulating digestive secretions
- Autonomic nervous system: extrinsically innervates the alimentary canal, with sympathetic nerves restricting enteric neurons and parasympathetic nerves increasing GI secretion and motility
Blood Supply
- Transports protein and carbohydrate to the liver via the hepatic portal system
- Delivers nutrients and oxygen to organs of the alimentary canal, with 25% of blood pumped entering arteries serving the intestines during rest and digestion
The Peritoneum
- Holds digestive organs in place, with parietal and visceral peritoneum regions
- Peritoneal cavity: space between parietal and visceral peritoneum
Digestive System Processes and Regulation
- Mouth: ingests, chews, and mixes food, beginning chemical breakdown of carbs and lipids
- Pharynx: propels food to the esophagus, lubricating food and passage
- Esophagus: propels food to the stomach, with upper and lower esophageal sphincters controlling food entry and acid reflux
- Deglutition (swallowing): movement of food to the stomach, with 4-8 seconds for solid food and 1 second for soft food and liquid, involving voluntary, pharyngeal, and esophageal phases
The Stomach
- Links the esophagus to the small intestine, responsible for digestion, contractions, and changing position and size
- Empty stomach is about half the size of a fist, can stretch to hold 4 liters, and has an additional oblique muscle to churn food
- Cardia, fundus, body, and pylorus regions, with gastric glands producing hydrochloric acid, pepsinogen, and mucous
Gastric Secretion
- Three phases: cephalic, gastric, and intestinal
- Cephalic phase: brief, stimulated by sight, smell, taste, or thought of food, with chemical secretion of mucous and no digestive enzymes
Feces and Defecation
- Feces: undigested food residue, unabsorbed substances, bacteria, old cells from GI mucosa, inorganic salts, and some water
- Valsalva maneuver: voluntary procedure to remove feces, increasing intra-abdominal pressure
- Feces in the anal canal opens the internal sphincter, giving the choice to open the external sphincter
Accessory Organs
- Liver: receives nutrients from the small intestine, processes nutrients, drugs, and toxins, and produces bile for emulsification of lipids in the small intestine
- Pancreas: exocrine and endocrine functions, producing bile and pancreatic lipase for digestion
Large Intestine
- Finishes absorption, forms feces, and eliminates it, with four regions: cecum, colon, rectum, and anal canal
- Bacterial flora: trillions of nonpathogenic bacteria live in the large intestine, facilitating digestion, absorption, and synthesis of certain vitamins
Digestion and Absorption
- Chemical digestion finishes carb and protein digestion in the small intestine
- Most lipids are undigested and require bile and pancreatic lipase
- Most water is absorbed through osmosis
- Mechanical digestion: haustral contractions, peristalsis, and mass movement in the large intestine
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.