Podcast
Questions and Answers
What is the primary mechanism of action for moist heat sterilization?
What is the primary mechanism of action for moist heat sterilization?
- Coagulating proteins in microorganisms (correct)
- Disrupting the DNA of pathogens
- Oxidizing cellular components
- Destroying the cell membrane of microorganisms
At what temperature is milk typically pasteurized using the Holder method?
At what temperature is milk typically pasteurized using the Holder method?
- 72°C for 15-20 seconds
- 56°C for one hour
- 100°C for 10 minutes
- 63°C for 30 minutes (correct)
Which of the following correctly describes the use of boiling in sterilization?
Which of the following correctly describes the use of boiling in sterilization?
- It guarantees the destruction of all endospores
- It can kill vegetative forms of bacterial pathogens (correct)
- It is effective against all types of viruses reliably
- It is a preferred method for sterilizing vaccines
What is a key feature of the autoclave designed by Charles Chamberland?
What is a key feature of the autoclave designed by Charles Chamberland?
What temperature and duration are generally used for a vaccine preparation in a hot water bath?
What temperature and duration are generally used for a vaccine preparation in a hot water bath?
What is the primary action of hydrogen peroxide as an oxidizing agent?
What is the primary action of hydrogen peroxide as an oxidizing agent?
Which of the following is a disadvantage of metallic salts used as disinfectants?
Which of the following is a disadvantage of metallic salts used as disinfectants?
What types of surfaces can ethylene oxide effectively sterilize?
What types of surfaces can ethylene oxide effectively sterilize?
Which filter types are commonly used for sterilization by filtration?
Which filter types are commonly used for sterilization by filtration?
What type of radiation is considered suitable for rapid mass sterilization?
What type of radiation is considered suitable for rapid mass sterilization?
What is the primary method by which dry heat sterilization kills microorganisms?
What is the primary method by which dry heat sterilization kills microorganisms?
At what temperature is a holding period of 2 hours most effective for dry heat sterilization?
At what temperature is a holding period of 2 hours most effective for dry heat sterilization?
Which of the following agents is NOT classified as a chemical agent for sterilization?
Which of the following agents is NOT classified as a chemical agent for sterilization?
What type of filtration is used for liquids?
What type of filtration is used for liquids?
Which treatment method is specifically described as ideal for destroying contaminated materials?
Which treatment method is specifically described as ideal for destroying contaminated materials?
Which of the following methods involves using a Bunsen flame?
Which of the following methods involves using a Bunsen flame?
What is the range of temperatures that a dry oven operates within for sterilization?
What is the range of temperatures that a dry oven operates within for sterilization?
Which chemical agent is specifically used for inanimate objects?
Which chemical agent is specifically used for inanimate objects?
At what temperature and duration is flash sterilization achieved?
At what temperature and duration is flash sterilization achieved?
Which of the following chemical agents is NOT effective against spores?
Which of the following chemical agents is NOT effective against spores?
Which statement correctly describes the action of hydrogen peroxide?
Which statement correctly describes the action of hydrogen peroxide?
What is the recommended concentration of alcohol for disinfection purposes?
What is the recommended concentration of alcohol for disinfection purposes?
Which of the following uses formaldehyde?
Which of the following uses formaldehyde?
What is the primary goal of sterilization?
What is the primary goal of sterilization?
Chlorine compounds are primarily utilized for which purpose?
Chlorine compounds are primarily utilized for which purpose?
Which method is commonly used for sterilization of surgical instruments that can be damaged by moist heat?
Which method is commonly used for sterilization of surgical instruments that can be damaged by moist heat?
What is a key property of phenolic derivatives in antisepsis?
What is a key property of phenolic derivatives in antisepsis?
What does disinfection achieve?
What does disinfection achieve?
Iodine solutions are known for what type of action against bacteria?
Iodine solutions are known for what type of action against bacteria?
What physical condition is required for autoclaving?
What physical condition is required for autoclaving?
Which process involves the mechanical removal of microbes from surfaces?
Which process involves the mechanical removal of microbes from surfaces?
What was a significant advancement in the mid-1800s to prevent surgical infections?
What was a significant advancement in the mid-1800s to prevent surgical infections?
Which of the following is a method of microbial growth control?
Which of the following is a method of microbial growth control?
What does a bacteriostatic agent do?
What does a bacteriostatic agent do?
What were the death rates due to nosocomial infections in surgeries prior to modern aseptic techniques?
What were the death rates due to nosocomial infections in surgeries prior to modern aseptic techniques?
Which of the following is NOT considered an antiseptic?
Which of the following is NOT considered an antiseptic?
What is a characteristic of bacterial spores that makes sterilization challenging?
What is a characteristic of bacterial spores that makes sterilization challenging?
What is considered the absence of significant contamination?
What is considered the absence of significant contamination?
Which process specifically targets the destruction of vegetative pathogens?
Which process specifically targets the destruction of vegetative pathogens?
What term describes an agent that kills spores?
What term describes an agent that kills spores?
What is the difference between antiseptics and disinfectants?
What is the difference between antiseptics and disinfectants?
Flashcards
Sterilization
Sterilization
The process of completely eliminating all microorganisms, including highly resistant bacterial spores, from an object or surface.
Disinfection
Disinfection
The killing or removal of most microorganisms, but not necessarily all, including bacterial spores, from an object or surface.
Antisepsis
Antisepsis
The process of reducing the number of microbes on living tissue to a safe level.
Alternation of membrane permeability
Alternation of membrane permeability
Signup and view all the flashcards
Damage to proteins
Damage to proteins
Signup and view all the flashcards
Damage to nucleic acids
Damage to nucleic acids
Signup and view all the flashcards
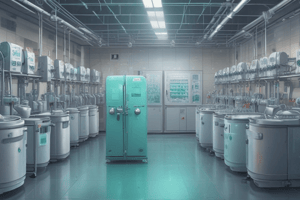
Autoclaving
Autoclaving
Signup and view all the flashcards
Ethylene oxide gas sterilization
Ethylene oxide gas sterilization
Signup and view all the flashcards
Sanitization
Sanitization
Signup and view all the flashcards
Degermation
Degermation
Signup and view all the flashcards
Sepsis
Sepsis
Signup and view all the flashcards
Asepsis
Asepsis
Signup and view all the flashcards
Dry Heat Sterilization
Dry Heat Sterilization
Signup and view all the flashcards
Chemical Sterilization
Chemical Sterilization
Signup and view all the flashcards
Pasteurization
Pasteurization
Signup and view all the flashcards
Ionizing Radiation Sterilization
Ionizing Radiation Sterilization
Signup and view all the flashcards
Ultraviolet (UV) Radiation Sterilization
Ultraviolet (UV) Radiation Sterilization
Signup and view all the flashcards
Filtration
Filtration
Signup and view all the flashcards
Flaming/Incineration
Flaming/Incineration
Signup and view all the flashcards
Autoclave
Autoclave
Signup and view all the flashcards
Boiling for sterilization
Boiling for sterilization
Signup and view all the flashcards
Steam sterilization at atmospheric pressure
Steam sterilization at atmospheric pressure
Signup and view all the flashcards
Sterilization below 100 degrees Celsius
Sterilization below 100 degrees Celsius
Signup and view all the flashcards
What is sterilization?
What is sterilization?
Signup and view all the flashcards
What is disinfection?
What is disinfection?
Signup and view all the flashcards
What is antisepsis?
What is antisepsis?
Signup and view all the flashcards
What is the ideal concentration of alcohol for disinfection?
What is the ideal concentration of alcohol for disinfection?
Signup and view all the flashcards
Why are aldehydes used as disinfectants?
Why are aldehydes used as disinfectants?
Signup and view all the flashcards
What are halogens used for in disinfection?
What are halogens used for in disinfection?
Signup and view all the flashcards
What are phenols used for?
What are phenols used for?
Signup and view all the flashcards
What limits hydrogen peroxide's disinfecting power?
What limits hydrogen peroxide's disinfecting power?
Signup and view all the flashcards
How does Hydrogen peroxide work?
How does Hydrogen peroxide work?
Signup and view all the flashcards
What is Ethylene oxide gas used for?
What is Ethylene oxide gas used for?
Signup and view all the flashcards
How do metallic salts like silver, copper, and mercury work as disinfectants?
How do metallic salts like silver, copper, and mercury work as disinfectants?
Signup and view all the flashcards
How does filtration sterilize heat-sensitive liquids?
How does filtration sterilize heat-sensitive liquids?
Signup and view all the flashcards
How does non-ionizing radiation like UV rays sterilize?
How does non-ionizing radiation like UV rays sterilize?
Signup and view all the flashcards
Study Notes
Sterilization, Disinfection, and Antisepsis
- Microorganisms cause contamination, infection, and decay
- Early civilizations used methods like salting, smoking, pickling, and sun exposure to preserve food
- Aseptic techniques were developed in the mid-1800s to prevent contamination of surgical wounds
- Nosocomial infections caused significant patient deaths before aseptic techniques
- Methods of microbial growth control include altering membrane permeability, damaging proteins, and damaging nucleic acids
- Prions are the most resistant, followed by bacterial spores, mycobacteria, and cysts of protozoa
- Viruses with lipid envelopes are the least resistant
Definition of Sterilization
- Sterilization is the process of eliminating all microorganisms, including spores.
- It is essential for surgical procedures and other medical applications where contamination cannot be tolerated.
Methods of Sterilization
-
Physical Agents:
- Heat: Dry heat (e.g., incineration, dry oven) and moist heat (e.g., steam under pressure, autoclave). Dry heat sterilization is more powerful than moist heat sterilization.
- The autoclave works under pressure (121°C or 132°C for various time intervals)
- Temperature is controlled by a thermostat and double-walled insulation conserves energy.
- Autoclaves are either vertical or horizontal cylinders with an opening for placing items to be sterilized. A pressure gauge measures the pressure, and a safety valve allows steam to escape
- Radiation: Ionizing radiation (e.g., X-rays, gamma rays, cosmic rays) and non-ionizing radiation (e.g., UV rays).
- Heat: Dry heat (e.g., incineration, dry oven) and moist heat (e.g., steam under pressure, autoclave). Dry heat sterilization is more powerful than moist heat sterilization.
-
Chemical Agents:
- Gases: Ethylene oxide, hydrogen peroxide vapor, and others
- Liquids: Various chemical solutions
- Alcohols like ethanol or isopropyl alcohol frequently used as disinfectants, are often used in concentrations between 60%-90%
- They also effectively disinfect clinical thermometers.
- They can effectively disinfect the skin prior to venipunctures.
- Other Methods: Various chemical methods are employed for sterilization
- Formaldehyde and glutaraldehyde are frequently used as disinfectants.
- Phenols are employed to disinfect various surfaces and objects in hospitals.
-
Mechanical Removal: Filtration (air and liquids)
- Candle, Asbestos, and sintered glass filters are used for sterilization.
Methods of Disinfection
- Disinfectants kill many microorganisms but not all
- Antiseptics are less toxic chemical solutions
- Often, disinfectants and antiseptics are used together to ensure proper procedures
Principles of effective disinfection
- Concentration of disinfectant
- Organic matter
- pH
- Time
Terminology
- Degermation: Mechanical removal of microbes
- Sepsis: Bacterial contamination
- Asepsis: The absence of significant contamination
- Bactericidal: Kills bacteria
- Bacteriostatic: Inhibits bacteria growth but doesn't kill
- Sporicidal: Kills spores
- Sterilization: Kills all organisms, including spores
- Disinfection: Kills many organisms (not all), not spores
- Antiseptic: Disinfectant use directly on exposed body surfaces
- Sanitization: Mechanical removal of microbes
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on various sterilization techniques, including moist heat sterilization, pasteurization methods, and the use of radiation. This quiz explores key concepts such as the functioning of autoclaves, chemical agents for disinfecting, and filtration methods. Perfect for students in microbiology or healthcare fields.