Podcast
Questions and Answers
What is the typical temperature used in autoclaving for sterilization?
What is the typical temperature used in autoclaving for sterilization?
- 254°C
- 121°C (correct)
- 160°C
- 100°C
Boiling water for 10-15 minutes is considered a true sterilization method.
Boiling water for 10-15 minutes is considered a true sterilization method.
False (B)
What is the primary method of killing microorganisms in dry heat sterilization?
What is the primary method of killing microorganisms in dry heat sterilization?
oxidizing microbial cells
_______ is a physical sterilization method that uses gamma rays or electron beams to break down DNA in microorganisms.
_______ is a physical sterilization method that uses gamma rays or electron beams to break down DNA in microorganisms.
Match the following physical sterilization methods with their applications:
Match the following physical sterilization methods with their applications:
Which physical sterilization method is suitable for sterilizing metal instruments?
Which physical sterilization method is suitable for sterilizing metal instruments?
UV-C light is effective for deep penetration through materials.
UV-C light is effective for deep penetration through materials.
What is the maximum temperature used in dry heat sterilization typically?
What is the maximum temperature used in dry heat sterilization typically?
Which technique is primarily used for drug testing and toxicology?
Which technique is primarily used for drug testing and toxicology?
Automated analyzers are only useful for measuring glucose levels.
Automated analyzers are only useful for measuring glucose levels.
What is the purpose of electrophoresis in laboratory analysis?
What is the purpose of electrophoresis in laboratory analysis?
In the laboratory, it is important to follow __________ protocols to handle pathogens safely.
In the laboratory, it is important to follow __________ protocols to handle pathogens safely.
What is the primary purpose of sterilization?
What is the primary purpose of sterilization?
Match the following safety measures with their purposes:
Match the following safety measures with their purposes:
All disinfectants can be used as antiseptics.
All disinfectants can be used as antiseptics.
Name two types of sterilization methods.
Name two types of sterilization methods.
High level disinfectants can kill all forms of microbes including _____ and _____ after prolonged exposure.
High level disinfectants can kill all forms of microbes including _____ and _____ after prolonged exposure.
Which of the following is an example of a low level disinfectant?
Which of the following is an example of a low level disinfectant?
Match the following disinfectants with their classifications:
Match the following disinfectants with their classifications:
Chemical vapor sterilization requires high heat for effective sterilization.
Chemical vapor sterilization requires high heat for effective sterilization.
What is the minimum pressure and temperature required for the Chemiclave process?
What is the minimum pressure and temperature required for the Chemiclave process?
Which staining technique is used primarily to detect Mycobacterium species, such as tuberculosis?
Which staining technique is used primarily to detect Mycobacterium species, such as tuberculosis?
Blood analysis can evaluate the components and characteristics of blood to detect only blood disorders.
Blood analysis can evaluate the components and characteristics of blood to detect only blood disorders.
What is the purpose of using agar plates in bacterial diagnosis?
What is the purpose of using agar plates in bacterial diagnosis?
The __________ technique is used to identify Gram-positive and Gram-negative bacteria based on their cell wall structure.
The __________ technique is used to identify Gram-positive and Gram-negative bacteria based on their cell wall structure.
Match the following techniques with their primary usage:
Match the following techniques with their primary usage:
Which method is commonly used to differentiate among Gram-negative bacteria?
Which method is commonly used to differentiate among Gram-negative bacteria?
Name one automated system used for biochemical testing.
Name one automated system used for biochemical testing.
Phase-contrast and dark-field microscopy are useful for enhancing visualization of bacterial morphology and motility.
Phase-contrast and dark-field microscopy are useful for enhancing visualization of bacterial morphology and motility.
What is the primary function of automated hematology analyzers?
What is the primary function of automated hematology analyzers?
Blood smear microscopy is primarily used for the diagnosis of infections like malaria and leukemia.
Blood smear microscopy is primarily used for the diagnosis of infections like malaria and leukemia.
What tests are used to assess blood coagulation?
What tests are used to assess blood coagulation?
The __________ analysis involves measuring electrolyte levels in blood.
The __________ analysis involves measuring electrolyte levels in blood.
Match the following tests with their functions:
Match the following tests with their functions:
What condition can low levels of hemoglobin indicate?
What condition can low levels of hemoglobin indicate?
Flow cytometry is primarily used for assessing organ function.
Flow cytometry is primarily used for assessing organ function.
What does ELISA stand for?
What does ELISA stand for?
Flashcards
Sterilization
Sterilization
The process of killing all living microorganisms, including spores.
Disinfectants
Disinfectants
Antimicrobial agents applied to non-living surfaces to kill or reduce the number of harmful microorganisms.
Antiseptics
Antiseptics
Antimicrobial agents used on living tissues (like skin) to reduce the risk of infection.
Chemical Sterilization
Chemical Sterilization
Signup and view all the flashcards
Chemical Liquid Sterilization
Chemical Liquid Sterilization
Signup and view all the flashcards
High-Level Disinfectants
High-Level Disinfectants
Signup and view all the flashcards
Low-Level Disinfectants
Low-Level Disinfectants
Signup and view all the flashcards
Chemical Vapor Sterilization
Chemical Vapor Sterilization
Signup and view all the flashcards
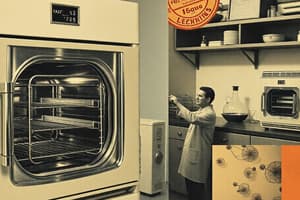
Autoclave Sterilization
Autoclave Sterilization
Signup and view all the flashcards
Incineration
Incineration
Signup and view all the flashcards
Gram Staining
Gram Staining
Signup and view all the flashcards
Acid-Fast Staining
Acid-Fast Staining
Signup and view all the flashcards
Phase-Contrast Microscopy
Phase-Contrast Microscopy
Signup and view all the flashcards
Agar Plates
Agar Plates
Signup and view all the flashcards
Coagulase Test
Coagulase Test
Signup and view all the flashcards
What is autoclaving?
What is autoclaving?
Signup and view all the flashcards
What is dry heat sterilization?
What is dry heat sterilization?
Signup and view all the flashcards
What is filtration sterilization?
What is filtration sterilization?
Signup and view all the flashcards
What is ionizing radiation sterilization?
What is ionizing radiation sterilization?
Signup and view all the flashcards
What is UV radiation sterilization?
What is UV radiation sterilization?
Signup and view all the flashcards
What is boiling sterilization?
What is boiling sterilization?
Signup and view all the flashcards
What is incineration sterilization?
What is incineration sterilization?
Signup and view all the flashcards
Automated Hematology Analyzers
Automated Hematology Analyzers
Signup and view all the flashcards
Blood Smear Microscopy
Blood Smear Microscopy
Signup and view all the flashcards
Hemoglobin and Hematocrit Tests
Hemoglobin and Hematocrit Tests
Signup and view all the flashcards
Blood Coagulation Tests
Blood Coagulation Tests
Signup and view all the flashcards
Flow Cytometry
Flow Cytometry
Signup and view all the flashcards
Bone Marrow Analysis
Bone Marrow Analysis
Signup and view all the flashcards
Clinical Chemistry
Clinical Chemistry
Signup and view all the flashcards
Spectrophotometry
Spectrophotometry
Signup and view all the flashcards
Chromatography
Chromatography
Signup and view all the flashcards
Gas Chromatography (GC)
Gas Chromatography (GC)
Signup and view all the flashcards
High-Performance Liquid Chromatography (HPLC)
High-Performance Liquid Chromatography (HPLC)
Signup and view all the flashcards
Electrophoresis
Electrophoresis
Signup and view all the flashcards
Automated Analyzers
Automated Analyzers
Signup and view all the flashcards
Study Notes
Sterilization, Disinfectants, and Antiseptics
- Sterilization is the killing of all living microbes, including spores.
- Disinfectants are antimicrobial agents used on non-living objects to reduce pathogenic microorganisms.
- Antiseptics are antimicrobial substances applied to living tissue to reduce infection or decay. Antiseptics must not damage the living tissue.
- Not all disinfectants are antiseptics.
Sterilization Methods
- Sterilization methods are categorized as chemical or physical.
- Chemical sterilization is used for devices sensitive to high heat or irradiation (e.g., rubbers, plastics).
- Chemical liquid sterilization
- Chemical vapor sterilization
- Physical sterilization uses physical agents to eliminate microorganisms. Examples include:
- Autoclaving (Moist Heat): Uses pressurized steam at high temperatures (121°C or 250°F) for 15-20 minutes to sterilize heat-resistant items.
- Dry Heat Sterilization: Uses high temperatures (160-180°C or 320-356°F) for extended time to sterilize heat-resistant materials.
- Filtration: Removes microorganisms from liquids or air using filters with small pore sizes.
- Radiation (Ionizing Radiation): Uses gamma rays or electron beams to sterilize materials by damaging microbial DNA.
- Ultraviolet (UV) Radiation: Uses UV-C light (254 nm) to damage microbial DNA, preventing replication.
- Boiling: Boiling water (100°C or 212°F) for 10-15 minutes kills most bacteria and some viruses. However, this method is not a sterilizing method.
- Incineration: Destroys contaminated material by burning.
Additional Information
- Classification of Disinfectants: Disinfectants are grouped into high-level, intermediate-level, and low-level based on their effectiveness against different organisms.
- Chemical Vapor Under Pressure (Chemiclave): A process that uses chemical mixtures (alcohol, formaldehyde, ketone, acetone, water) heated under pressure to sterilize. Requires 20 minutes at 131° C and 20 lbs pressure.
- Fumigation: A sterilization method employing potassium permanganate and formalin in a specific ratio.
- Laboratory Safety: Follow safety protocols for handling chemicals, biological hazards, and equipment.
Diagnosis of Bacteria
- Microscopy, Gram Staining: Used to classify bacteria (Gram-positive or Gram-negative) based on cell wall structure.
- Acid-Fast Staining: Useful for identifying bacteria like Mycobacterium (e.g., tuberculosis).
- Biochemical tests: used to identify different types of bacteria, such as catalase and coagulase tests.
- Automated systems: Methods like VITEK and BD Phoenix automate biochemical testing.
- Molecular Methods, DNA Sequencing: Provides highly specific identification and information on antibiotic resistance.
Blood Analysis
- Complete Blood Count (CBC): Evaluates blood components (RBCs, WBCs, platelets) to diagnose infections and disorders.
- Automated Hematology Analyzers and Blood Smear Microscopy to diagnose infections and disorders.
- Hemoglobin and Hematocrit tests: Assess RBC count and hemoglobin concentration, identifying conditions like anemia.
- Blood Coagulation Tests (PT/PTT): Assess blood clotting function to diagnose bleeding disorders.
- Platelet function Tests: Used to evaluate platelets adhesion and aggregation.
- Flow Cytometry: Helps study blood cell populations using fluorescent antibodies.
- Bone Marrow Analysis: Provides information about blood cell production, crucial for diagnosing hematological cancers, anemias, and bone marrow disorders.
Clinical Chemistry
- Spectrophotometry: Measures light absorbance by substances in bodily fluids (blood, urine) to determine their concentration (e.g., glucose, cholesterol).
- Enzymatic reactions: used in biochemical tests employing enzymatic reactions for analysis.
- Electrolyte Analysis: Measures electrolytes (e.g., sodium, potassium) for assessing kidney disease, dehydration, or heart issues.
- Immunoassays (ELISA): Detects specific proteins or hormones (e.g., insulin, TSH, troponin) using antibodies in blood samples.
- Chromatography such as GC and HPLC: Separates and identifies compounds in bodily fluids to detect drug use or monitor therapeutic drug levels.
- Electrophoresis: Separates proteins based on charge and size for detecting abnormal protein levels.
- Automated analyzers are used in modern laboratories for multiple biochemical tests.
Laboratory Safety
- First aid: necessary materials and personnel training are essential.
- Biochemical hazards: appropriate storage, handling, and disposal of chemicals are critical.
- Biological hazards: follow and adhere to biosafety protocols to minimize risks.
- General safety: use of SOPs (Standard Operating Procedures) and proper equipment is necessary. Always report hazards.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.