Podcast
Questions and Answers
In a patient with Systemic Lupus Erythematosus (SLE), what clinical manifestation should prompt immediate notification to the healthcare provider due to potential cardiopulmonary complications?
In a patient with Systemic Lupus Erythematosus (SLE), what clinical manifestation should prompt immediate notification to the healthcare provider due to potential cardiopulmonary complications?
- Exacerbation of the malar rash after sun exposure.
- Increased joint pain and stiffness in the extremities.
- Reports of fatigue and generalized weakness.
- Complaints of chest pain that worsens with breathing or movement. (correct)
A client with Rheumatoid Arthritis (RA) is prescribed corticosteroids to manage inflammation. Which focused assessment is most critical for the nurse to perform regularly?
A client with Rheumatoid Arthritis (RA) is prescribed corticosteroids to manage inflammation. Which focused assessment is most critical for the nurse to perform regularly?
- Evaluating for signs of gastrointestinal bleeding.
- Monitoring glucose levels for hyperglycemia. (correct)
- Assessing for changes in range of motion and joint flexibility.
- Monitoring for signs of skin breakdown and delayed wound healing.
Which diagnostic finding is most indicative of Hodgkin's Lymphoma when evaluating a patient with persistent lymphadenopathy?
Which diagnostic finding is most indicative of Hodgkin's Lymphoma when evaluating a patient with persistent lymphadenopathy?
- Increased percentage of blast cells in bone marrow aspirate.
- Presence of Reed-Sternberg cells on lymph node biopsy. (correct)
- Detection of Bence-Jones protein in urine sample.
- Elevated levels of Epstein-Barr virus antibodies in serum.
A patient with Multiple Myeloma is at risk for developing spinal cord compression. Which symptom should the nurse prioritize when assessing for this complication?
A patient with Multiple Myeloma is at risk for developing spinal cord compression. Which symptom should the nurse prioritize when assessing for this complication?
A patient diagnosed with Acute Myeloid Leukemia (AML) is undergoing induction chemotherapy. Which lab value would be most concerning during this phase of treatment?
A patient diagnosed with Acute Myeloid Leukemia (AML) is undergoing induction chemotherapy. Which lab value would be most concerning during this phase of treatment?
What is the primary mechanism by which HIV compromises the immune system?
What is the primary mechanism by which HIV compromises the immune system?
A patient with advanced HIV is diagnosed with Pneumocystis jirovecii Pneumonia (PCP). What clinical finding is most indicative of this infection?
A patient with advanced HIV is diagnosed with Pneumocystis jirovecii Pneumonia (PCP). What clinical finding is most indicative of this infection?
In a patient with Scleroderma, which of the following clinical manifestations is associated with increased pulmonary hypertension risk?
In a patient with Scleroderma, which of the following clinical manifestations is associated with increased pulmonary hypertension risk?
Following a bone marrow transplant a patient with Acute Lymphoblastic Leukemia (ALL) has the following lab results: platelets 90,000 and WBC 3,000. What is the priority nursing intervention?
Following a bone marrow transplant a patient with Acute Lymphoblastic Leukemia (ALL) has the following lab results: platelets 90,000 and WBC 3,000. What is the priority nursing intervention?
For a patient receiving chemotherapy, what is the most critical aspect of central venous access device (CVAD) management to prevent complications?
For a patient receiving chemotherapy, what is the most critical aspect of central venous access device (CVAD) management to prevent complications?
A client with a history of anaphylaxis after a bee sting is prescribed an epinephrine auto-injector. What education component of the medication teaching is most critical?
A client with a history of anaphylaxis after a bee sting is prescribed an epinephrine auto-injector. What education component of the medication teaching is most critical?
A patient is diagnosed with Chronic Myeloid Leukemia (CML) and prescribed a tyrosine kinase inhibitor (TKI). What is the most important instruction for the nurse to emphasize regarding medication adherence?
A patient is diagnosed with Chronic Myeloid Leukemia (CML) and prescribed a tyrosine kinase inhibitor (TKI). What is the most important instruction for the nurse to emphasize regarding medication adherence?
A patient with Non-Hodgkin’s Lymphoma is beginning treatment. Which preventative measure is most important to teach to maintain skin integrity during treatment?
A patient with Non-Hodgkin’s Lymphoma is beginning treatment. Which preventative measure is most important to teach to maintain skin integrity during treatment?
A patient with Systemic Lupus Erythematosus (SLE) tests positive for the ANA and LE Cell Test. What is the significance of these findings related to the pathophysiology of SLE?
A patient with Systemic Lupus Erythematosus (SLE) tests positive for the ANA and LE Cell Test. What is the significance of these findings related to the pathophysiology of SLE?
After completing chemotherapy for Acute Lymphoblastic Leukemia (ALL), a pediatric client is encouraged to slowly gain weight. Which rationale explains the importance of this recommendation?
After completing chemotherapy for Acute Lymphoblastic Leukemia (ALL), a pediatric client is encouraged to slowly gain weight. Which rationale explains the importance of this recommendation?
A client is undergoing a Mantoux skin test for tuberculosis (TB) screening. What type of hypersensitivity reaction is involved in a positive Mantoux test?
A client is undergoing a Mantoux skin test for tuberculosis (TB) screening. What type of hypersensitivity reaction is involved in a positive Mantoux test?
Which of the following is an important teaching point the nurse must include when providing discharge instruction for a patient with scleroderma?
Which of the following is an important teaching point the nurse must include when providing discharge instruction for a patient with scleroderma?
A phlebotomist is stuck by a needle while collecting blood from a patient who is HIV positive. What is the most important initial action for the phlebotomist to take?
A phlebotomist is stuck by a needle while collecting blood from a patient who is HIV positive. What is the most important initial action for the phlebotomist to take?
A patient with a diagnosis of Metastatic cancer has a potassium level of 2.9. Which assessment finding is most concerning?
A patient with a diagnosis of Metastatic cancer has a potassium level of 2.9. Which assessment finding is most concerning?
A patient with a history of Rheumatoid Arthritis (RA) is at risk of developing symmetrical polyarthritis. What clinical manifestation in the patient's hands would warrant provider notification?
A patient with a history of Rheumatoid Arthritis (RA) is at risk of developing symmetrical polyarthritis. What clinical manifestation in the patient's hands would warrant provider notification?
Flashcards
Systemic Lupus Erythematosus (SLE)
Systemic Lupus Erythematosus (SLE)
Auto-antibody production, more common in women, caused by an abnormal immune and phagocytic system that decreases tolerance to self.
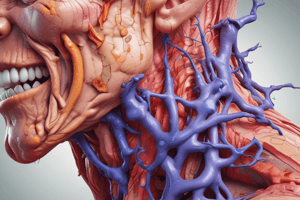
Rheumatoid Arthritis
Rheumatoid Arthritis
Autoimmune, inflammatory response causing immune cells to aggregate in small joints, leading to bone deformities.
Scleroderma
Scleroderma
Collagenous tissue deposits in connective tissues, triggered by genetics and infection, affecting skin and internal organs.
Hypersensitivity 1: Anaphylaxis
Hypersensitivity 1: Anaphylaxis
Signup and view all the flashcards
Hypersensitivity 2
Hypersensitivity 2
Signup and view all the flashcards
Hypersensitivity 3
Hypersensitivity 3
Signup and view all the flashcards
Hypersensitivity 4
Hypersensitivity 4
Signup and view all the flashcards
Pneumocystitis jirovecii Pneumonia
Pneumocystitis jirovecii Pneumonia
Signup and view all the flashcards
Human Immunodeficiency Virus (HIV)
Human Immunodeficiency Virus (HIV)
Signup and view all the flashcards
Chronic Myeloid Leukemia (CML)
Chronic Myeloid Leukemia (CML)
Signup and view all the flashcards
Acute Myeloid Leukemia (AML)
Acute Myeloid Leukemia (AML)
Signup and view all the flashcards
Multiple Myeloma
Multiple Myeloma
Signup and view all the flashcards
Acute Lymphoblastic Leukemia (ALL)
Acute Lymphoblastic Leukemia (ALL)
Signup and view all the flashcards
Hodgkin’s Lymphoma
Hodgkin’s Lymphoma
Signup and view all the flashcards
Non-Hodgkin’s Lymphoma
Non-Hodgkin’s Lymphoma
Signup and view all the flashcards
Metastatic Cancer
Metastatic Cancer
Signup and view all the flashcards
Chemotherapy
Chemotherapy
Signup and view all the flashcards
Normal WBC
Normal WBC
Signup and view all the flashcards
Normal PLT
Normal PLT
Signup and view all the flashcards
Prothrombin Time
Prothrombin Time
Signup and view all the flashcards
Study Notes
- The notes below provide key information about various diseases and disorders, along with their clinical manifestations, diagnostic methods, and treatments.
Systemic Lupus Erythematosus (SLE)
- Auto-antibody production occurs primarily in women with SLE.
- An abnormal immune and phagocytic system leads to decreased tolerance to self.
- Glomerulonephritis, indicating kidney involvement, signals systemic SLE.
- Malar rash and cardiac/respiratory inflammation are clinical signs.
- Diagnosis involves ANA and LE Cell Tests.
- Advise patients to seek medical attention for chest pain with breathing/movement.
- Education includes wearing sunscreen to prevent malar rash exacerbation.
Rheumatoid Arthritis
- An autoimmune, inflammatory response causes immune cells to accumulate in small joints.
- Bilateral-symmetrical polyarthritis, bone deformities, and fatigue are clinical manifestations.
- Diagnosis is confirmed through labs and X-rays.
- Educate patients about medications, encourage activity with rest, and adaptive equipment use.
- Monitor glucose levels due to potential corticosteroid treatments.
Scleroderma
- Collagenous tissue deposits occur in the body's connective tissues due to genetic factors and infection.
- The condition can affect the skin or present systemically with internal organ involvement.
- CREST (calcinosis, Raynaud's, esophageal dysfunction, sclerodactyly, telangiectasias) and vascular lesions on the lips are clinical signs.
Hypersensitivity Reactions
- Type 1: Anaphylaxis
- Type 2: Tissue-specific IgG/IgM (blood transfusions, medication transfusions)
- Type 3: Antigen-antibody immune complex (strep leading to glomerulonephritis)
- Type 4: Contact reaction
- A positive Mantoux skin test for TB indicates a hypersensitivity reaction.
Pneumocystitis jirovecii Pneumonia
- It is a fungal infection in the lungs, often seen in those with weakened immune systems (HIV/cancer).
- Hypoxemia is a key clinical manifestation.
Human Immunodeficiency Virus (HIV)
- Caused by a viral infection affecting CD4, lymphocytes, and macrophages.
- As an RNA retrovirus, HIV converts to DNA to replicate and infect cells.
- Transcriptase, integrase, and protease are essential for viral replication.
- The primary replication site is the GI tract.
- Risk factors include being a healthcare worker, unprotected sex, STIs, and being born to an infected mother (intrauterine, delivery, or breastfeeding).
- Initially asymptomatic; females may experience vaginal itching with discharge.
- Advanced HIV/AIDS symptoms include difficulty swallowing, SOB, productive cough, weight loss, chest pain, night sweats, and low CD4 count.
- This can cause wasting syndrome, so monitor electrolytes.
- Immunosuppressed patients: advise rest before meals, avoid cleaning litterboxes, thoroughly clean and cook raw foods, disinfect surfaces, and monitor temperatures.
Chronic Myeloid Leukemia (CML)
- Gradual onset typically occurs between ages 40-50, with a poor prognosis due to chemo response.
- Clinical signs: fatigue, weight loss, bleeding, discomfort, sweating, and high granulocyte count.
- Diagnosis: bone marrow aspiration and CBC with differential.
- Treatment: Tyrosine kinase inhibitor (PO), with emphasis on medication adherence.
Acute Myeloid Leukemia (AML)
- Acute onset with a median age of 64.
- Chromosomal problems lead to blast cell proliferation/mutation.
- AML presents in myriad ways due to assorted chromosomal translocations or inversions.
- Responds well to treatment.
- Clinical signs: splenomegaly, bone pain, anemia, and thrombocytopenia.
- Diagnosis: bone marrow aspiration, CBC, blood smear.
- Treatment: Aggressive chemotherapy, starting with induction therapy.
Multiple Myeloma
- Plasma cell disorder in antibody-secreting B lymphocytes.
- Antibodies destroy healthy cells.
- Clinical signs: bone lesions/issues and hypercalcemia.
- Complications: spinal fracture and risk for spinal cord compression.
- Diagnostic testing: Bone marrow biopsy and urinalysis for Bence-Jones protein.
- Treatments: steroids, chemo, stem cell transplant, radiation.
- Recommendations: increased daily water intake and maintain high UOP.
Acute Lymphoblastic Leukemia
- Childhood cancer with malignant transformation of B (lymphoblast) cells.
- Clinical presentation: Abrupt onset of symptoms (fever, infection, anorexia), severe headache, vomiting, and increased immature WBC count.
- Diagnostic methods: bone marrow aspiration, CBC, and blood smear.
- Treatment: Chemo and steroids.
- High remission rates are typical.
- Expected normal labs post-treatment: platelet 150,000-400,000 and WBC 5,000-10,000.
- Encourage slow weight gain (1lb a week)
Hodgkin’s Lymphoma
- It is a lymphoid neoplasm starting in lymph nodes, spreading to tissues/organs.
- Clinical signs: Lymphadenopathy (cervical, supraclavicular, mediastinal, i.e., neck, shoulder, chest); B symptoms (fever, sweating, weight loss); pruritus; jaundice; herpes zoster.
- Diagnostic identification: Biopsy showing Reed-Sternberg Cells with normal platelets.
- Treatment: Chemo, stem cell transplant, and radiation.
- Education: avoid drying soaps/lotions, wear cotton clothing, use electric razor.
Non-Hodgkin’s Lymphoma
- Clinical signs: lymphadenopathy (abd, chest, neck) with fever, sweating, weight loss/anorexia; potential spinal cord compression.
- Diagnosis often occurs at a late stage due to its less aggressive nature.
- Treatment includes chemo, antibiotics, antifungals, antivirals, and pain management.
- Education: exercise x 30 min 5x a week.
Metastatic Cancer
- Pattern related to circulatory flow.
- Cell survival is not guaranteed after entering circulation.
- All tumors should undergo grading/staging.
- Monitor WBC daily during chemotherapy; a critical drop is a complication.
- Chemotherapy shrinks/destroys all cells.
- Administration routes: Orally, IV, or directly into spinal fluid via central venous access device.
Laboratory Values
- WBC: 5,000-10,000
- PLT: 150,000-400,000
- Prothrombin Time: 11-12.5 seconds
- HCT: Male 42-52%, Female 37-47%
- BUN: 10-20 mg/dL
- Potassium: 3.5-5 mEq/L
- Sodium: 135-145 mEq/L
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.