Podcast
Questions and Answers
Which of the following statements best describes the reductionist approach to understanding complex phenomena?
Which of the following statements best describes the reductionist approach to understanding complex phenomena?
- It emphasizes the importance of viewing the whole to understand the parts.
- It combines all perspectives to derive a singular conclusion.
- It considers only the individual components, ignoring the whole. (correct)
- It assumes that all observations are equally valid without context.
What is NOT one of the determinants of maximal contractile force in skeletal muscle?
What is NOT one of the determinants of maximal contractile force in skeletal muscle?
- Delivery of Ca++ to contractile proteins
- Depleted ATP levels (correct)
- Calcium Sensitivity
- Calcium Activated Force
In the context of skeletal muscle fatigue, what does decreased SR Ca2+ release contribute to?
In the context of skeletal muscle fatigue, what does decreased SR Ca2+ release contribute to?
- Increased muscle endurance
- Enhanced contractile efficiency
- Fatigue-induced force decline (correct)
- Improved calcium sensitivity
How does the analogy of the blind men and the elephant relate to understanding physiological phenomena?
How does the analogy of the blind men and the elephant relate to understanding physiological phenomena?
Which of the following is a potential factor contributing to fatigue in muscle contraction?
Which of the following is a potential factor contributing to fatigue in muscle contraction?
What is the primary effect of disuse on muscle fibers regarding their metabolic processes?
What is the primary effect of disuse on muscle fibers regarding their metabolic processes?
How does disuse affect muscle fiber Vmax, and what does this imply?
How does disuse affect muscle fiber Vmax, and what does this imply?
Which of the following describes a consequence of muscle disuse on fatigue resistance?
Which of the following describes a consequence of muscle disuse on fatigue resistance?
What phenomenon is associated with the motor innervation and voluntary activation of disused muscle?
What phenomenon is associated with the motor innervation and voluntary activation of disused muscle?
What role does Ca2+ play in the excitation-contraction coupling process?
What role does Ca2+ play in the excitation-contraction coupling process?
What change occurs to ACh receptors in disused muscle fibers?
What change occurs to ACh receptors in disused muscle fibers?
Which structure is responsible for the release of Ca2+ during muscle contraction?
Which structure is responsible for the release of Ca2+ during muscle contraction?
What is the effect of central fatigue on motor unit activation?
What is the effect of central fatigue on motor unit activation?
During muscle contraction, what happens to the actin filament?
During muscle contraction, what happens to the actin filament?
What initiates the action potential in a skeletal muscle fiber?
What initiates the action potential in a skeletal muscle fiber?
What best describes the group of motor units that work together to coordinate contractions of a single muscle?
What best describes the group of motor units that work together to coordinate contractions of a single muscle?
Which factor is NOT considered in fiber type classification schemes for muscle fibers?
Which factor is NOT considered in fiber type classification schemes for muscle fibers?
Which adaptation to training specifically involves changes in muscle fiber size?
Which adaptation to training specifically involves changes in muscle fiber size?
Which statement correctly distinguishes between oxidative and non-oxidative machinery in muscle fibers?
Which statement correctly distinguishes between oxidative and non-oxidative machinery in muscle fibers?
What role does membrane input resistance (Rm) play in the excitation of muscle fibers?
What role does membrane input resistance (Rm) play in the excitation of muscle fibers?
Flashcards
Motor Unit
Motor Unit
A single motor neuron and all the muscle fibers it innervates. This is the basic functional unit of muscle contraction.
Motor Pool
Motor Pool
The collection of all motor neurons that innervate a single muscle. This allows coordinated movement of the whole muscle.
Muscle Fiber Types
Muscle Fiber Types
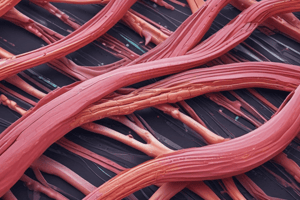
Muscle fibers are categorized based on their speed of contraction, resistance to fatigue, and metabolic pathways.
What are the 3 main factors used to classify muscle fiber types?
What are the 3 main factors used to classify muscle fiber types?
Signup and view all the flashcards
Adaptations to Training
Adaptations to Training
Signup and view all the flashcards
Disuse Effect on Muscle Fibers
Disuse Effect on Muscle Fibers
Signup and view all the flashcards
Reduced Force and Power
Reduced Force and Power
Signup and view all the flashcards
Metabolic Shift
Metabolic Shift
Signup and view all the flashcards
Change in Motor Innervation
Change in Motor Innervation
Signup and view all the flashcards
ACh Receptor Spread
ACh Receptor Spread
Signup and view all the flashcards
What is excitation-contraction coupling?
What is excitation-contraction coupling?
Signup and view all the flashcards
What role does acetylcholine play in muscle contraction?
What role does acetylcholine play in muscle contraction?
Signup and view all the flashcards
What is the role of the T-tubules?
What is the role of the T-tubules?
Signup and view all the flashcards
How does calcium trigger muscle contraction?
How does calcium trigger muscle contraction?
Signup and view all the flashcards
What is the power stroke?
What is the power stroke?
Signup and view all the flashcards
What are the 3 determinants of contractile force?
What are the 3 determinants of contractile force?
Signup and view all the flashcards
Muscle Fatigue
Muscle Fatigue
Signup and view all the flashcards
Decreased Maximal Ca2+ Activated Force
Decreased Maximal Ca2+ Activated Force
Signup and view all the flashcards
Decreased Ca2+ Sensitivity
Decreased Ca2+ Sensitivity
Signup and view all the flashcards
Decreased SR Ca2+ Release
Decreased SR Ca2+ Release
Signup and view all the flashcards
Study Notes
Muscle Module: Responses to Disuse, Training, and Aging (Sarcopenia)
- This module examines how muscles react to various conditions, including disuse, training, and aging.
- It also investigates the underlying mechanisms of muscle fatigue.
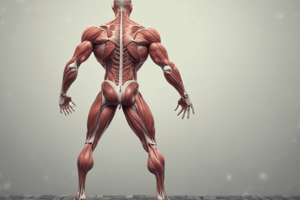
Muscle Atrophy vs. Muscle Hypertrophy
- Atrophy: A decrease in muscle size due to a reduction in the number or size of myofibers (muscle fibers).
- Hypertrophy: An increase in muscle size, typically due to an increase in the size or number of myofibers.
- Muscle degradation and synthesis interplay in response to various factors.
Causes of Sarcopenia (Aging-Related Muscle Loss)
- Age-related (primary): Genetic factors, hormonal changes, mitochondrial dysfunction, apoptosis of muscle fibers.
- Disuse: Physical inactivity, immobilization, weightlessness.
- Illness-related (cachexia): Cancer, chronic inflammation, infections like sepsis
- Other issues: Chronic obstructive pulmonary disease (COPD), Diabetes, Renal failure, AIDS, Burn injury, Fasting, Sepsis, and Neurodegenerative Diseases.
Mechanisms for Age-Related Muscle Loss (Sarcopenia)
- Muscle atrophy is related to a combination of inactivity and aging-related processes.
- Chronic inflammation
- Reduced protein synthesis
- Increased protein breakdown
- Loss of lean body mass
Muscle Fiber Type and Responses to Disuse
-
Type I (slow oxidative) fibers: Important for endurance activities.
-
Type II (fast oxidative and fast glycolytic) fibers: Essential for short bursts of strength.
-
Both fiber types can atrophy with disuse. Type II fibers display a greater loss with disuse.
Disuse Atrophy and Generalizations
- Disuse atrophy is typically reversible.
- Significant in load-bearing conditions, such as bed rest or spaceflight
- Weightlessness and bed rest cause significant atrophy in humans.
- Immobilization in limb suspension causes considerable atrophy in animals.
Adaptations to Training
-
Muscle fiber size: Hypertrophy (increase in size), Hyperplasia (increase in number)
-
Enzyme activity: Increase in oxidative and/or glycolytic enzymes
-
Isoform expression: Change in the type of myosin ATPase and Ca++ ATPase
-
Organelles and Structures: Increased mitochondria; more extensive extracellular scaffolding, increased capillarization, more extensive network
-
Endurance-type training specifically leads to metabolic adaptations.
-
Increased use of fats as fuel and reduced reliance on carbohydrates.
Removal of Calcium Ions to Stop Muscle Contraction
- Sodium-calcium exchanger and calcium pump in the sarcolemma remove calcium from the cell.
- Calcium pumps in the sarcoplasmic reticulum (SR) actively transport Ca++ out of the cytoplasm.
- Calcium-binding proteins (e.g., calreticulin, calsequestrin) bind calcium within the SR, preventing further activation
Cross-Bridge Cycle
- Breakdown of ATP provides the energy for the power stroke, which allows myosin heads to bind and then release actin, then repeat.
Muscle Fiber Type Characteristics
-
Slow oxidative (type I): Slow contraction speed, fatigue-resistant, aerobic respiration
-
Fast oxidative-glycolytic (type IIa): Intermediate contraction speed and fatigue resistance. Aerobic/anaerobic respiration.
-
Fast glycolytic (type IIb): Fast contraction speed, easily fatigued. Anaerobic respiration.
-
These differences in metabolic pathways affect activities best suited to each fiber type.
Motor Units
- Functional groups of interconnected motor neurons innervating a group of muscle fibers.
- Motor units work together to coordinate contraction.
- Motor units are of different types, and are recruited in an orderly fashion according to size.
Fiber Type Classification Schemes
- Color: Red fibers rich in myoglobin are oxidative versus white fibers.
- Contraction speed: Slow versus Intermediate speed versus fast
- Fatigability: Slow versus intermediate speed versus fast
- Metabolism: Aerobic versus anaerobic
Muscle Atrophy Associated with Aging
- Decrease in muscle fiber number and size
- Decrease in motor neurons number
- Motor unit reorganization
- Decreases in force generation
- Changes in excitation-contraction coupling
Dynamic Strength Changes with Aging
- Gradual decline in strength associated with age, typically starting around 40-50 years of age. This decline occurs more prominently in dynamic strength measures than muscle mass.
Strength Loss Considerations
- Strength loss is not uniform throughout the body: Lower body strength is more greatly affected during aging;
- Possible mechanisms include relative amount of disuse, distal axonal degradation, and differing susceptibilities to aging across muscle fiber types (Type II fibers are more susceptible).
Problems with Studying Fatigue
- Variability: Fatigue can be influenced by factors like motivation, nutrition, environment, and training status.
- Experimental protocols vary significantly
- Extrapolating in vitro results to in vivo and clinical scenarios requires cautious interpretation.
- Separating fatigue from cellular damage
Mechanisms for Skeletal Muscle Fatigue
- Central fatigue (CNS): Decrease in motor units recruited due to factors like psychological issues or biochemical changes within the brain and spinal cord.
- Peripheral fatigue: Physical changes within a muscle itself. Mechanisms include ionic shifts, metabolic insufficiency, reactive oxygen species, changes in excitation-contraction coupling, and force decline.
Other Degenerative Features of Aged Muscles
- Hyaline degeneration (glassy changes) and vacuoles at fiber ends
- Fat and connective tissues replacing muscle fiber tissue
- Necrosis (cell death) associated with infiltration of immune cells
- Increased central nucleation (multi-nuclei fibers)
- Fiber splitting
- Impaired mitochondrial function
- Accumulation of SR material
Clinical Implications of Sarcopenia
- Loss of muscle mass leads to reduced basal metabolic rate
- Contributing to metabolic disorders like type 2 diabetes and osteoporosis
- Decreased muscle strength & functional capacity associated with difficulties in activities of daily living.
- Increased risk of falls & injuries
- More difficulty maintaining physical activity.
- High risk of fractures, even minor falls.
Preventing and Managing Sarcopenia
- High-resistance training
- Exercise programs involving combined resistance and aerobic exercise
- Increased physical activity levels
- Nutritional adjustments.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on the nuances of skeletal muscle physiology, exploring topics like muscle contraction determinants, fatigue mechanisms, and the effects of disuse. Understand how various physiological concepts relate to muscle functionality and performance. This quiz encompasses key elements that every student of exercise science should be familiar with.