Podcast
Questions and Answers
What is the purpose of the sinuses in the head?
What is the purpose of the sinuses in the head?
- To aid in the digestion of food
- To regulate body temperature
- To protect the brain from injury
- To lighten the weight of the head and give resonance to the voice (correct)
What is the result of oxygen absorption by the blood vessels in the nasal membrane during inflammation?
What is the result of oxygen absorption by the blood vessels in the nasal membrane during inflammation?
- A painful, negative pressure in the sinuses (correct)
- A reduction in sinus congestion
- A decrease in blood pressure
- An increase in body temperature
What is the response of the membranes to the negative pressure in the sinuses?
What is the response of the membranes to the negative pressure in the sinuses?
- They release a hormone to reduce inflammation
- They become thinner to facilitate drainage
- They constrict to reduce blood flow
- They release a transudate, which fills the sinus cavity (correct)
What is the characteristic symptom of sinusitis?
What is the characteristic symptom of sinusitis?
Where is the sinus cavity located?
Where is the sinus cavity located?
Which of the following is NOT a cause of sinusitis?
Which of the following is NOT a cause of sinusitis?
What is the characteristic feature of all sinusitis and sinus headache?
What is the characteristic feature of all sinusitis and sinus headache?
What is the common location of pain in a Maxillary Sinus Headache?
What is the common location of pain in a Maxillary Sinus Headache?
What is the primary cause of about 25% of maxillary viral/bacterial sinusitis?
What is the primary cause of about 25% of maxillary viral/bacterial sinusitis?
What is the name of the condition characterized by the onset of itchy eyes, roof of mouth, pharynx and eyes?
What is the name of the condition characterized by the onset of itchy eyes, roof of mouth, pharynx and eyes?
What is the name of the condition that can occur if a bacterial or viral infection is left untreated?
What is the name of the condition that can occur if a bacterial or viral infection is left untreated?
What is the common feature of a bacterial or viral infection?
What is the common feature of a bacterial or viral infection?
What is the name of the most common culprit of allergic sinusitis/ rhinitis?
What is the name of the most common culprit of allergic sinusitis/ rhinitis?
What is the primary symptom of sinusitis?
What is the primary symptom of sinusitis?
What is the common structure that can cause a structural obstruction?
What is the common structure that can cause a structural obstruction?
What is a common predisposing factor for fungal infections in the sinuses?
What is a common predisposing factor for fungal infections in the sinuses?
What is a characteristic of rebound sinus headache?
What is a characteristic of rebound sinus headache?
What should be assessed during a case history for sinusitis?
What should be assessed during a case history for sinusitis?
What may indicate possible conjunctivitis during an observation?
What may indicate possible conjunctivitis during an observation?
What should be palpated initially during the palpation assessment?
What should be palpated initially during the palpation assessment?
What is a short-term aim of treatment for sinusitis?
What is a short-term aim of treatment for sinusitis?
What may be a long-term aim of treatment for sinusitis?
What may be a long-term aim of treatment for sinusitis?
What should be checked during the testing assessment?
What should be checked during the testing assessment?
What is a possible complication of chronic use of nasal sprays?
What is a possible complication of chronic use of nasal sprays?
What should be referred for immediate medical treatment during assessment?
What should be referred for immediate medical treatment during assessment?
What is the recommended treatment for chronic, recurrent sinusitis?
What is the recommended treatment for chronic, recurrent sinusitis?
Why is massage contraindicated for clients with fever?
Why is massage contraindicated for clients with fever?
What is the benefit of incorporating facial steams into the treatment?
What is the benefit of incorporating facial steams into the treatment?
What is the recommended frequency of treatment during a sinusitis flare-up?
What is the recommended frequency of treatment during a sinusitis flare-up?
Why should the therapist avoid placing the client in a face cradle if the sinuses are swollen and tender?
Why should the therapist avoid placing the client in a face cradle if the sinuses are swollen and tender?
What is the benefit of teaching full diaphragmatic breathing to clients with sinusitis?
What is the benefit of teaching full diaphragmatic breathing to clients with sinusitis?
What is the purpose of incorporating cold compresses over the cheeks, eyes, and forehead?
What is the purpose of incorporating cold compresses over the cheeks, eyes, and forehead?
What essential oil should be avoided in facial steams for clients with Hay Fever or Ragweed allergies?
What essential oil should be avoided in facial steams for clients with Hay Fever or Ragweed allergies?
Why should the therapist work within the client's pain tolerance, especially over the sinuses?
Why should the therapist work within the client's pain tolerance, especially over the sinuses?
What is the recommended self-care practice for clients with sinusitis?
What is the recommended self-care practice for clients with sinusitis?
What is the primary goal of surgery in treating sinusitis?
What is the primary goal of surgery in treating sinusitis?
What medication may be used to treat allergic sinusitis/rhinitis?
What medication may be used to treat allergic sinusitis/rhinitis?
What may be administered to hypertensive patients taking oral antihistamines and vasoconstrictors?
What may be administered to hypertensive patients taking oral antihistamines and vasoconstrictors?
What is the mechanism of action of Cromolyn sodium?
What is the mechanism of action of Cromolyn sodium?
When is systemic, oral corticosteroids such as Prednisone typically used?
When is systemic, oral corticosteroids such as Prednisone typically used?
How is immunosuppressed patients' fungal infections of the sinuses typically treated?
How is immunosuppressed patients' fungal infections of the sinuses typically treated?
What is Acute Bronchitis?
What is Acute Bronchitis?
What is Chronic Bronchitis classified as?
What is Chronic Bronchitis classified as?
What is the result of irritation and inflammation of the bronchial walls in Bronchitis?
What is the result of irritation and inflammation of the bronchial walls in Bronchitis?
What is a characteristic of Mucopurulent Bronchitis?
What is a characteristic of Mucopurulent Bronchitis?
What is the role of the diaphragm in anatomy related to respiratory conditions?
What is the role of the diaphragm in anatomy related to respiratory conditions?
What muscles are involved in respiratory anatomy?
What muscles are involved in respiratory anatomy?
What is usually a preceding symptom of bronchitis?
What is usually a preceding symptom of bronchitis?
What is a characteristic of chronic bronchitis?
What is a characteristic of chronic bronchitis?
What is a common cause of bronchitis?
What is a common cause of bronchitis?
What is an important aspect of assessing a client with bronchitis?
What is an important aspect of assessing a client with bronchitis?
What is the purpose of vocal fremitus?
What is the purpose of vocal fremitus?
What may indicate pneumonia?
What may indicate pneumonia?
What should the therapist do during percussion tests?
What should the therapist do during percussion tests?
What may be noticed in clients with chronic bronchitis?
What may be noticed in clients with chronic bronchitis?
What should the therapist assess during a case history for bronchitis?
What should the therapist assess during a case history for bronchitis?
What is an important aspect of testing for bronchitis?
What is an important aspect of testing for bronchitis?
What is the primary aim of the treatment in terms of facilitating removal of secretions?
What is the primary aim of the treatment in terms of facilitating removal of secretions?
What is the recommended position for treating the right middle lobe?
What is the recommended position for treating the right middle lobe?
What is the benefit of using inhalations of certain essential oils in the treatment?
What is the benefit of using inhalations of certain essential oils in the treatment?
What is the purpose of teaching the client how to perform DDB?
What is the purpose of teaching the client how to perform DDB?
What is a contraindication for this treatment?
What is a contraindication for this treatment?
What is the purpose of the assisted forced expiration/cough technique?
What is the purpose of the assisted forced expiration/cough technique?
What is the recommended frequency of treatment?
What is the recommended frequency of treatment?
What is the purpose of joint play and thoracic mobilizations in the treatment?
What is the purpose of joint play and thoracic mobilizations in the treatment?
What is the benefit of using tapotement in the treatment?
What is the benefit of using tapotement in the treatment?
Why should the therapist arrange a hand signal with the client?
Why should the therapist arrange a hand signal with the client?
What is the primary function of the alveoli in the lungs?
What is the primary function of the alveoli in the lungs?
What is the result of long-term exposure to irritants such as smoking and pollution in the lungs?
What is the result of long-term exposure to irritants such as smoking and pollution in the lungs?
What is the role of alpha-1 antitrypsin (AAT) protein in the lungs?
What is the role of alpha-1 antitrypsin (AAT) protein in the lungs?
What is a characteristic symptom of emphysema?
What is a characteristic symptom of emphysema?
What is the age range of most emphysema patients?
What is the age range of most emphysema patients?
What is the result of chronic irritation of the bronchioles?
What is the result of chronic irritation of the bronchioles?
What is a common feature of emphysema patients diagnosed before age 50?
What is a common feature of emphysema patients diagnosed before age 50?
What is the term used to describe the merging of alveoli to form large sacs?
What is the term used to describe the merging of alveoli to form large sacs?
What percentage of their energy does a healthy person expend on breathing?
What percentage of their energy does a healthy person expend on breathing?
What is the result of a person having to work harder for gas exchange due to emphysema?
What is the result of a person having to work harder for gas exchange due to emphysema?
What is a common complication of emphysema?
What is a common complication of emphysema?
What is a characteristic of a person with emphysema?
What is a characteristic of a person with emphysema?
What is the aim of treatment in the early stage of emphysema?
What is the aim of treatment in the early stage of emphysema?
What is a technique that may be taught to clients with emphysema?
What is a technique that may be taught to clients with emphysema?
What is a consideration for massage therapy in clients with emphysema?
What is a consideration for massage therapy in clients with emphysema?
What is the prognosis for emphysema?
What is the prognosis for emphysema?
What is a medical treatment for emphysema?
What is a medical treatment for emphysema?
What is a possible complication of emphysema?
What is a possible complication of emphysema?
What is a common risk factor for developing asthma?
What is a common risk factor for developing asthma?
What happens to the diaphragm during an asthma attack?
What happens to the diaphragm during an asthma attack?
What is a characteristic symptom of asthma?
What is a characteristic symptom of asthma?
What is the type of hypersensitivity reaction that occurs in asthma?
What is the type of hypersensitivity reaction that occurs in asthma?
What is a common trigger for asthma attacks?
What is a common trigger for asthma attacks?
What is a complication that can occur if asthma is left untreated?
What is a complication that can occur if asthma is left untreated?
What is a possible trigger for asthma?
What is a possible trigger for asthma?
What is a co-morbid condition that is often associated with asthma?
What is a co-morbid condition that is often associated with asthma?
What is a characteristic breathing pattern in people with asthma?
What is a characteristic breathing pattern in people with asthma?
What is a goal of massage therapy for asthma?
What is a goal of massage therapy for asthma?
What should be avoided during hydrotherapy for asthma?
What should be avoided during hydrotherapy for asthma?
What is a characteristic of Cardiac Asthma?
What is a characteristic of Cardiac Asthma?
What is a recommended frequency for massage therapy for asthma?
What is a recommended frequency for massage therapy for asthma?
What is a benefit of incorporating steams into the treatment for asthma?
What is a benefit of incorporating steams into the treatment for asthma?
What is a type of exercise recommended for asthma?
What is a type of exercise recommended for asthma?
What is a complication associated with asthma?
What is a complication associated with asthma?
What is the primary organ affected by Cystic Fibrosis?
What is the primary organ affected by Cystic Fibrosis?
What is the average life expectancy for Cystic Fibrosis patients with modern day management?
What is the average life expectancy for Cystic Fibrosis patients with modern day management?
What is the result of chronic infection/inflammation in the bronchiole walls?
What is the result of chronic infection/inflammation in the bronchiole walls?
What is a common respiratory symptom of Cystic Fibrosis?
What is a common respiratory symptom of Cystic Fibrosis?
What percentage of male Cystic Fibrosis patients are infertile?
What percentage of male Cystic Fibrosis patients are infertile?
What is a digestive symptom of Cystic Fibrosis?
What is a digestive symptom of Cystic Fibrosis?
When was Cystic Fibrosis first officially diagnosed and labeled?
When was Cystic Fibrosis first officially diagnosed and labeled?
What is a common complication of Cystic Fibrosis?
What is a common complication of Cystic Fibrosis?
What is the primary cause of cystic fibrosis?
What is the primary cause of cystic fibrosis?
How do people typically inherit cystic fibrosis?
How do people typically inherit cystic fibrosis?
What is the purpose of sweat testing in diagnosing cystic fibrosis?
What is the purpose of sweat testing in diagnosing cystic fibrosis?
Why is genetic testing important for adults who are carriers of cystic fibrosis?
Why is genetic testing important for adults who are carriers of cystic fibrosis?
What is the primary aim of treating cystic fibrosis in massage therapy?
What is the primary aim of treating cystic fibrosis in massage therapy?
What is the main focus of techniques used in massage therapy for cystic fibrosis?
What is the main focus of techniques used in massage therapy for cystic fibrosis?
What is the importance of addressing digestive issues in clients with cystic fibrosis?
What is the importance of addressing digestive issues in clients with cystic fibrosis?
What is the benefit of incorporating preventive care in massage therapy for cystic fibrosis?
What is the benefit of incorporating preventive care in massage therapy for cystic fibrosis?
Flashcards are hidden until you start studying
Study Notes
Sinusitis
- The sinuses are hollow areas located above the eyes and behind and lateral to the nose, serving to lighten the weight of the head, give resonance to the voice, and provide additional surface area for the sticky, mucous membrane lining to trap pathogens during inhalation.
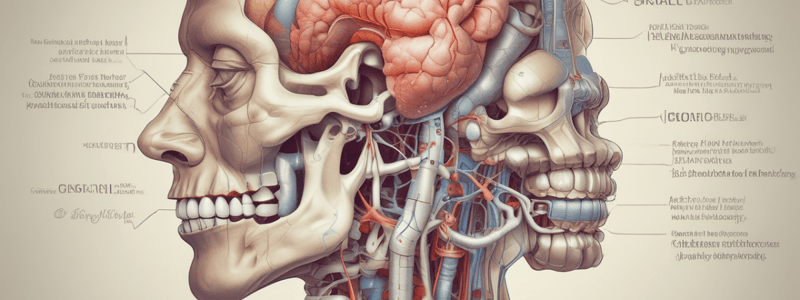
Anatomy
- Frontal, Ethmoidal, Sphenoidal, and Maxillary Sinuses
- Frontal and Occipital bones, Zygomatic Arch, Supra and Infra orbital margins, Mandible and Temporomandibular joint, Sphenoid bone, Cervical spine (particularly the Atlanto-occipital and Atlanto-axial joints)
- Frontalis and Occipitalis, Sub-occipitals, Upper Trapezius, Levator Scapula, Splenius Capitus, Splenius Cervicis, Sternocleidomastoid, Scalenes, and Masseter muscles
Signs and Symptoms
- Guarded head and neck movement
- Pained facial expression
- FEVER
- Malaise, muscle/joint ache
- Insomnia
- Loss of Appetite (anorexia)
- Swelling, redness around eyes and cheeks
- Watery eyes
- Itchy eyes, nose, throat
- Cough
- Mucous: thin & watery or thick & sticky
- Colour of mucous: clear, yellow, green
- Headache (especially in the morning)
- Muscle stiffness of head and neck
- Pain upon forward flexion
- Irritability
- Inability to concentrate
- Toothache
- Conjunctivitis
- Signs of Meningitis (rapid onset stiff neck and severe headache)
Types of Sinusitis
- Acute or chronic, recurrent inflammation of the mucous membranes in the para-nasal sinuses
- Caused by:
- Viral or bacterial infection
- Allergic reaction/rhinitis
- Structural obstruction
- Fungal infection
- Intolerance to medicine
Sinus Headache
- A painful headache that often accompanies a sinusitis
- Location and quality defined by the location of maximum sinus irritation
- Types:
- Frontal Sinus Headache: located in the frontal area above the eyes
- Ethmoidal Sinus Headache: causes both a frontal headache that is described as "splitting" and pain behind the eyes
- Sphenoidal Sinus Headache: less well localized, causing pain in both the frontal and occipital area
- Maxillary Sinus Headache: causes pain in the maxillary area under the eyes, a frontal headache, and often toothache
Causes
- Viral/Bacterial:
- May require medical treatment
- Usually occurs when the immune defenses are low
- Mucous is often thick, sticky, and green or yellow in colour
- Client often has accompanying symptoms of malaise, fever, and chills
- If left untreated, the infection can infiltrate the facial bones causing osteomyelitis and permanent bone damage or can infect the central nervous system causing Meningitis
- Allergic Sinusitis/Rhinitis:
- Related to allergic reactions and is seasonal in nature
- Hay Fever is the most common culprit along with wind-borne pollens
- Characterized by the onset of itchy eyes, roof of mouth, pharynx, and eyes followed or accompanied by nasal congestion, sneezing, clear watery nasal discharge, watery eyes, frontal headache, and possible conjunctivitis
- Structural Obstruction:
- A deviated septum or nasal polyps are the most common obstructions
- While they are not infectious in and of themselves, they tend to obstruct the normal flow and drainage of the sinuses and create a desirable growth medium for bacterial infection
- Fungal Infections:
- Most common in people who are immune-suppressed and as such, are more susceptible to infection by common fungi such as Aspergillus and Curvularia
- Treated aggressively with IV therapy and paras nasal sinus surgery as this condition can often become a fatal infection
- Medication Intolerance:
- On rare occasions, people can have reactions to medications such as aspirin or ibuprofen, which leads to inflammation of the sinuses but not infection
- Rebound Sinus Headache:
- Overuse of nasal sprays that contain decongestants and anti-inflammatory medication
Bronchitis
- Acute bronchitis: self-limited inflammation of the tracheobronchial tree with eventual healing and return to function
- Chronic bronchitis: prolonged exposure to nonspecific bronchial irritants resulting in hypersecretion of mucus and productive cough for a period of 3 months for two consecutive years
- Types of chronic bronchitis:
- Simple chronic: mild, persistent cough with clear sputum
- Mucopurulent: thick, yellowish sputum due to bacterial infection
- Obstructive: structural damage due to continual infection and inflammation, leading to obstruction and obliteration of small airways
Anatomy
- Joints involved: C and T spine, Costovertebral and Sternocostal joints, and Sternoclavicular joints
- Muscles involved: diaphragm, intercostals, abdominal muscles, Pectoralis Major and minor, SCM, Scalenes, Thoracic erectors, and Posterior cervical muscles
Signs and Symptoms
- Acute:
- Preceded by cold or flu
- Chills, fever, back and muscle pain, sore throat
- Onset of cough signals onset of bronchitis
- Cough is initially dry and non-productive, becomes productive after a few days
- Sputum is suggestive of bacterial infection
- Persistent fever suggests pneumonia
- Chronic:
- Cough, sputum, wheeze, dyspnea
- May have a mild smoker’s cough
- Cough, wheeze, recurrent respiratory infections
- Copious sputum with signs of infection
- Tendency to be “Blue Bloaters” in later stages
- Extended or slowed forced expiration (taking longer than 4 seconds) with some wheeze noted towards the end
Causes
- Smoking is the most common cause of bronchitis
- Pollution
- Viral or bacterial agents
- Dust, Solvent, fumes, Acids, etc.
- Repeated attacks of acute bronchitis
Assessment and Testing
- Case history: general health, history of smoking, history of respiratory infections, diagnosis of chronic bronchitis, onset, symptoms, presence of productive cough, color/quality of sputum, presence of blood in sputum, medications, other treatments and results, complicating factors
- Observations: postural assessment, tachypnea, cough and sputum, possible cyanosis of lips and nail beds
- Palpation: increased tone of accessory muscles of respiration, palpate muscles of the upper chest and shoulders for increased tone, movement of thoracic cage during breathing
- Testing: vocal fremitus, percussion tests, breath sounds
Treatment Aims and Techniques
- Facilitate removal of secretions
- Restore or maintain thoracic mobility
- Eliminate muscle spasming and trigger points in overused muscles of respiration or muscles overused due to excessive coughing
- Educate client re: FDB and proper coughing and smoking cessation
- Address postural conditions
- Techniques: myofascial techniques, general Swedish techniques, tapotement, airway clearance, shaking, huff technique, assisted forced expiration/cough technique, joint play, thoracic mobilizations, trigger point therapy, and stretching
Contraindications and Precautions
- Fever, infection which indicate contagious disease
- Osteoporosis is a precaution due to heavy tapotement in the treatment
- Some medications may alter the client’s sensation to pain
- People with severe asthma may have to have treatment intensity altered
- Some positions and treatment depth may have to be altered in people with circulatory and cardiac complications
Frequency and Remedial Exercise and Self-Care
- Frequency: depends upon general health, frequency and severity of condition
- Treat for two weeks, 1x week for two weeks, reassess
- Remedial exercise and self-care: teach DDB and a productive cough, pec, scalene, SCM stretching, Clapp’s crawl, thoracic self-mobilizations, intercostal and abdominal strengthening
Emphysema
- A condition in which the alveoli of the lungs become fibrous and inelastic, limiting the exchange of oxygen and carbon dioxide.
- Characterized by the merging of alveoli, decreasing the surface area, and limiting gas exchange.
- Classed with Chronic Bronchitis as a Chronic Obstructive Pulmonary Disease (COPD).
Causes
- Exposure to irritants such as smoking, pollution, and grain dust damages the alveoli.
- Long-term exposure to irritants can overcome the protective protein Alpha-1 Antitrypsin (AAT), leading to the destruction of alveolar elastin fibers.
- Chronic irritation results in chronic bronchitis, leading to the destruction of the alveoli.
Signs and Symptoms
- Pain with breathing
- Difficulty breathing on exertion
- Little interest in eating
- Rales (bubbles, rasps when breathing)
- Difficulty exhaling (takes longer)
- Pursed lip exhalation
- Barrel chest
- Diminished diaphragmatic breathing
- Loss of general muscle tone due to decreased activity
Complications
- More prone to influenza and other respiratory conditions
- Bullae may rupture, causing lung collapse
- Blood clots
- Pulmonary embolism
- Heart failure
Assessment
- General health
- Current symptoms
- Onset
- Breathlessness and activities that cause it
- Productive cough (chronic bronchitis)
- Blood pressure
- Precipitating factors (smoking, pollution, work-related)
- Medication
- Other therapies
- Activities that must be modified (hot bath or shower, climbing stairs)
Observations
- Postural assessment
- Barrel chest
- Prolonged or pursed lip breathing
- Head forward posture
- Weight loss
- Rosy appearance (Pink Puffers)
- Bluish appearance (Blue Bloaters – indicates chronic bronchitis)
- Clubbed ends of fingers
- Palpation of all muscles of respiration and accessory muscles for hypertrophy and trigger points
Treatment Aims
- Early stage: remove irritating stimulus, promote stress reduction, and encourage full diaphragmatic breathing
- Later stage: promote relaxation, address general tissue health, and consider contraindications
Remedial Exercise and Self-Care
- Teach full diaphragmatic breathing
- Teach pursed lip breathing rather than forced expiration
- Gentle stretching for neck, shoulders, and chest
Prognosis
- Emphysema is an irreversible disease
- If found and treated early, further damage can be avoided
- Medical attention may include bronchodilators, diuretics, oxygen supplementation, and surgery
Sinusitis
- No information provided in the text.
Asthma
- Characterized by episodes of acute airway obstruction due to bronchospasm and mucus production from exposure to various stimuli.
- More common in children, who may grow out of the condition, but may return in later years.
- Risk factors include:
- Childhood history of asthma
- Environmental hazards (city pollution, second-hand smoke)
- Gastro-esophageal Reflux Disease (GERD)
- Eczema
- Hay fever
- Obesity
Signs and Symptoms
- During an attack:
- Bronchospasm traps air in the lungs
- Diaphragm unable to relax
- Rib cage unable to relax, intercostals unable to contract
- Air remains in the lungs, difficulty exhaling
- Use of accessory muscles of respiration (scalenes, SCM, upper trapezius) to expand the upper chest
- Tendency to breathe with the upper chest
- Barrel chest
- Hypertonicity of accessory muscles of respiration
- Fatigue due to decreased oxygen
- Anxiety with deep respiration
Causes
- Extrinsic:
- Type 1 hypersensitivity reaction (histamine release)
- External substances (dust, pollen, peanuts, emotional upset)
- Family history
- Intrinsic:
- Idiopathic
- Exercise-related
- Respiratory tract infection
- Emotional or physical stress
- Genetic predisposition
- Mixed:
- Combination of extrinsic and intrinsic factors
Triggers
- Smoke
- Stress
- Respiratory infection
- Intense heat or cold
- Work-related substances (detergents, plastics, fumes)
Cardiac Asthma
- Related to congestive cardiac failure, resulting in excess fluid in the lungs
Assessment and Treatment
- Case history:
- General health
- Age of onset
- Type of asthma
- Frequency of attacks
- Known triggers
- Treatment received
- Medications (inhaler)
- Aims of treatment:
- Decrease stress and anxiety
- Decrease tone of accessory muscles of respiration
- Increase mobilization of thorax
- Encourage diaphragmatic breathing
- Remove excess secretions between attacks
- Address postural concerns
- Decrease severity and frequency of attacks
- Contraindications:
- Do not massage during an attack
- Be aware of triggers
- Avoid stimulating work if stress or physical exertion is a trigger
- Avoid excessive heat or cold in hydrotherapy if it is a trigger
- Frequency of treatment:
- 1 hour/week for posture and respiratory function
- General monthly maintenance
- Remedial exercise and self-care:
- Encourage diaphragmatic breathing
- General exercise
- Treat for hyper kyphosis if indicated
- Stretches and breathing exercises
- Steams (with precautions)
Prognosis
- Asthma can be mild or severe, may remit in childhood, but may return in later years
- Associated with more severe cardiopulmonary complications
Cystic Fibrosis
- A disorder of the exocrine glands that affects the entire body and is ultimately fatal, usually due to pulmonary complications.
- The lungs and pancreas are the most affected organs, but the intestines and kidneys are also commonly affected.
- Not officially recognized as a COPD due to its systemic nature, but persistent coughing can lead to Bronchiectasis, which is sometimes considered a COPD.
- Life expectancy for untreated CF was less than 5 years old; with modern management, the global average is now 37 years old.
- In developed countries, it's not uncommon for CF patients to live into their 50's.
Bronchiectasis
- A permanent thickening of the bronchiole walls due to chronic infection/inflammation.
- Irreversible and prone to worsening, occasionally considered a member of the ‘COPD’ family.
History of Cystic Fibrosis
- First officially diagnosed and labeled in 1938.
- Observed historically as far back as the Middle Ages (1595).
Signs and Symptoms
- Respiratory symptoms:
- Persistent, productive cough with thick mucus
- Wheezing
- Shortness of breath
- Frequent infections of the lungs and sinuses
- Digestive symptoms:
- Greasy, foul-smelling stool
- Intestinal blockage and severe constipation (particularly in infants)
- Heartburn
- Other symptoms:
- Poor weight gain
- Stunted growth
- Infertility (98% of males, 20% of females)
- Pancreatic complications (e.g., diabetes)
- Excessive salt secretion through the skin
Causes
- Mutation of the 'Cystic Fibrosis Transmembrane Conductance Regulator' (CFTR) gene, with over 1900 known mutations.
- The gene is recessive, meaning a subject must inherit the defective gene from both parents to develop the disease.
- Possibility of being a carrier by possessing one defective gene.
Assessment
- Diagnostic testing is done during newborn screening.
- Adults can have genetic testing to determine if they are carriers.
- 'Sweat testing' measures chloride levels in sweat secretions, with a positive result being 60+ mmol/L.
Treatment
- Primary aims and treatment protocol are the same as for Chronic Bronchitis (mucus expulsion) and/or Constipation (improving transit time).
- Addressing digestive issues first allows for more comfort when placed in the appropriate respiratory drainage position.
- Techniques and contraindications are the same as for Bronchitis and Constipation.
- Remedial exercise and self-care can be applied as preventive care even if the client is not suffering from digestive problems.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.