Podcast
Questions and Answers
Which type of shock is characterized by a severe antibody-antigen reaction?
Which type of shock is characterized by a severe antibody-antigen reaction?
- Anaphylactic shock (correct)
- Cardiogenic shock
- Hypovolemic shock
- Septic shock
What is the primary cause of hypovolemic shock?
What is the primary cause of hypovolemic shock?
- Impaired heart function
- Loss of circulating or intravascular volume (correct)
- Maldistribution of blood volume
- Severe allergic reaction
Which of the following classifications of shock includes septic shock?
Which of the following classifications of shock includes septic shock?
- Cardiogenic shock
- Hypovolemic shock
- Obstructive shock
- Distributive shock (correct)
What is a key pathophysiological change that occurs in all types of shock?
What is a key pathophysiological change that occurs in all types of shock?
Which type of shock results from the heart's inability to pump effectively?
Which type of shock results from the heart's inability to pump effectively?
What is the primary result of neurogenic shock?
What is the primary result of neurogenic shock?
Which stage of shock is characterized by the highest levels of lactic acid production?
Which stage of shock is characterized by the highest levels of lactic acid production?
What compensatory mechanism is primarily responsible for increasing heart rate and contractility?
What compensatory mechanism is primarily responsible for increasing heart rate and contractility?
Which hormone is produced as a result of the activation of the renin response during compensatory stage?
Which hormone is produced as a result of the activation of the renin response during compensatory stage?
What effect does hyperventilation have during chemical compensation?
What effect does hyperventilation have during chemical compensation?
The progressive stage of shock can lead to which issue within the cardiovascular system?
The progressive stage of shock can lead to which issue within the cardiovascular system?
Which of the following responses is NOT a part of the hormonal compensation during shock?
Which of the following responses is NOT a part of the hormonal compensation during shock?
In the compensatory stage of shock, what is the primary purpose of blood shunting to vital organs?
In the compensatory stage of shock, what is the primary purpose of blood shunting to vital organs?
What is a consequence of renal dysfunction during the progressive stage of ventricular failure?
What is a consequence of renal dysfunction during the progressive stage of ventricular failure?
During which stage does shock become unresponsive to therapy and is considered irreversible?
During which stage does shock become unresponsive to therapy and is considered irreversible?
Which factor does NOT influence oxygen transport to tissues?
Which factor does NOT influence oxygen transport to tissues?
What primary dysfunction develops as a result of increased pulmonary capillary membrane permeability?
What primary dysfunction develops as a result of increased pulmonary capillary membrane permeability?
Which of the following is a sign of shock in the assessment and diagnosis stage?
Which of the following is a sign of shock in the assessment and diagnosis stage?
What physiological consequence results from splanchnic vasoconstriction during gastrointestinal dysfunction?
What physiological consequence results from splanchnic vasoconstriction during gastrointestinal dysfunction?
What should be the first step in ensuring adequate oxygenation during medical management?
What should be the first step in ensuring adequate oxygenation during medical management?
Which element is crucial for adequate cardiac output (CO) and subsequently for oxygen transport?
Which element is crucial for adequate cardiac output (CO) and subsequently for oxygen transport?
What initial signs indicate the progressive stage of hypovolemic shock?
What initial signs indicate the progressive stage of hypovolemic shock?
Which of the following is a characteristic of the refractory stage of hypovolemic shock?
Which of the following is a characteristic of the refractory stage of hypovolemic shock?
Which hemodynamic changes are expected in hypovolemic shock?
Which hemodynamic changes are expected in hypovolemic shock?
What is the primary goal in managing hypovolemic shock?
What is the primary goal in managing hypovolemic shock?
What is the expected clinical manifestation in the patient during the refractory stage of hypovolemic shock?
What is the expected clinical manifestation in the patient during the refractory stage of hypovolemic shock?
What characterizes absolute hypovolemia?
What characterizes absolute hypovolemia?
What is a compensatory mechanism that occurs when fluid volume loss is up to 30%?
What is a compensatory mechanism that occurs when fluid volume loss is up to 30%?
Which of the following best describes the progressive stage of hypovolemic shock?
Which of the following best describes the progressive stage of hypovolemic shock?
What does a decrease in venous return lead to in the context of hypovolemic shock?
What does a decrease in venous return lead to in the context of hypovolemic shock?
What blood gas abnormality is typically present during the progressive stage of hypovolemic shock?
What blood gas abnormality is typically present during the progressive stage of hypovolemic shock?
Which compensatory response occurs when fluid volume loss reaches 15% to 30%?
Which compensatory response occurs when fluid volume loss reaches 15% to 30%?
What indicates ineffective tissue perfusion during the progressive stage of hypovolemic shock?
What indicates ineffective tissue perfusion during the progressive stage of hypovolemic shock?
What is a potential clinical manifestation during the compensatory stage of hypovolemic shock?
What is a potential clinical manifestation during the compensatory stage of hypovolemic shock?
Flashcards
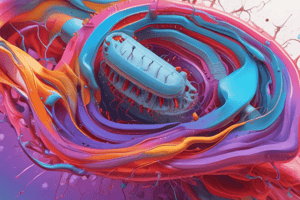
Shock
Shock
A widespread process hindering tissue perfusion, causing cellular, metabolic, and hemodynamic changes.
Hypovolemic Shock
Hypovolemic Shock
Shock resulting from fluid loss, internal or external.
Cardiogenic Shock
Cardiogenic Shock
Shock caused by the heart's poor pumping ability.
Distributive Shock
Distributive Shock
Signup and view all the flashcards
Septic Shock
Septic Shock
Signup and view all the flashcards
Anaphylactic Shock
Anaphylactic Shock
Signup and view all the flashcards
Neurogenic Shock
Neurogenic Shock
Signup and view all the flashcards
Initial Stage of Shock
Initial Stage of Shock
Signup and view all the flashcards
Compensatory Stage of Shock
Compensatory Stage of Shock
Signup and view all the flashcards
Progressive Stage of Shock
Progressive Stage of Shock
Signup and view all the flashcards
Refractory Stage of Shock
Refractory Stage of Shock
Signup and view all the flashcards
MAP
MAP
Signup and view all the flashcards
Hypovolemic Shock Causes
Hypovolemic Shock Causes
Signup and view all the flashcards
Absolute Hypovolemia
Absolute Hypovolemia
Signup and view all the flashcards
Relative Hypovolemia
Relative Hypovolemia
Signup and view all the flashcards
Clinical Manifestations of Hypovolemic Shock
Clinical Manifestations of Hypovolemic Shock
Signup and view all the flashcards
Compensatory stage of hypovolemia
Compensatory stage of hypovolemia
Signup and view all the flashcards
Progressive Stage of Hypovolemic Shock
Progressive Stage of Hypovolemic Shock
Signup and view all the flashcards
Refractory Stage of Hypovolemic Shock
Refractory Stage of Hypovolemic Shock
Signup and view all the flashcards
Hemodynamic Parameters in Hypovolemic Shock
Hemodynamic Parameters in Hypovolemic Shock
Signup and view all the flashcards
Reduced Cardiac Output (CO)
Reduced Cardiac Output (CO)
Signup and view all the flashcards
Lowered MAP
Lowered MAP
Signup and view all the flashcards
Medical Management of Shock
Medical Management of Shock
Signup and view all the flashcards
Study Notes
Definition of Shock
- Shock is a widespread process that impairs tissue perfusion causing cellular, metabolic, and hemodynamic alterations.
Classification of Shock
- Hypovolemic shock: results from fluid loss, either external or internal.
- Cardiogenic shock: occurs due to the heart's inability to pump effectively.
- Distributive shock: causes blood maldistribution within the body, further categorized into:
- Septic shock: arises from infection entering the body.
- Anaphylactic shock: caused by severe allergic reactions.
- Neurogenic shock: results from the loss of sympathetic nerve function
Stages of Shock
- Initial stage: decreased cardiac output leads to anaerobic metabolism, producing lactic acid.
- Compensatory stage: sympathetic nervous system activation increases heart rate, vasoconstriction, and redirects blood to vital organs. This involves neural, hormonal, and chemical responses.
- Progressive stage: compensatory mechanisms fail, leading to organ dysfunction like cardiovascular, central nervous system, pulmonary, renal, and gastrointestinal impairments.
- Refractory stage: shock becomes unresponsive to treatment, leading to multiple organ dysfunction syndrome (MODS) and eventual death.
Pathophysiology of the Compensatory Stage
- Neural response: increased heart rate, contractility, and vasoconstriction to redirect blood.
- Hormonal response: Includes:
- Renin response: causes vasoconstriction, aldosterone, and ADH release.
- Anterior pituitary stimulation: releases ACTH, leading to glucocorticoid release.
- Adrenal medulla stimulation: releases epinephrine and norepinephrine, reinforcing compensatory mechanisms.
- Chemical response: hyperventilation, resulting in respiratory alkalosis.
Pathophysiology of the Progressive Stage
- Cardiovascular system: Myocardial hypoperfusion causes dysfunction. Ventricular failure occurs.
- Central nervous system: Cerebral hypoperfusion causes SNS failure, cardiac and respiratory depression, and thermoregulatory failure.
- Pulmonary system: Pulmonary capillary membrane permeability, microemboli, and vasoconstriction lead to acute lung injury (ALI) and ventilatory failure.
- Renal system: Renal vasoconstriction causes renal hypoperfusion resulting in acute kidney injury (AKI).
- Gastrointestinal system: Splanchnic vasoconstriction and hypoperfusion impair gut function. Enteric bacteria release into the bloodstream, exacerbating shock.
Assessment and Diagnosis
- Mean arterial pressure (MAP) less than 60 mmHg and systolic BP less than 90 mmHg.
- Tachycardia or bradycardia.
- Altered mental status.
- Elevated serum lactate, arterial base deficit, serum bicarbonate, and reduced central or mixed venous oxygen saturation.
Medical Management
- Focus on restoring tissue perfusion through:
- Improving pulmonary gas exchange: Ensuring adequate oxygenation through airway management, supplemental oxygen, and mechanical ventilation.
- Adequate cardiac output and hemoglobin: Using fluids (crystalloids, colloids, or blood products) and medications like vasoconstrictors, vasodilators, inotropes, and anti-dysrhythmics.
Hypovolemic Shock
- Occurs due to inadequate intravascular volume, leading to decreased tissue perfusion and shock syndrome.
- Types:
- Absolute hypovolemia: external fluid loss (blood, plasma, etc).
- Relative hypovolemia: vasodilation reduces effective circulating volume.
Pathophysiology of Hypovolemic Shock
- Causes: Loss of circulating fluid volume, reduced venous return, lowered preload, decreased CO, inadequate cellular oxygen supply, and ineffective tissue perfusion.
Clinical Manifestations of Hypovolemic Shock
- Initial stage: fluid loss up to 15% (750 ml), compensatory mechanisms maintain CO, appears asymptomatic.
- Compensatory stage: fluid loss of 15-30% (750-1500 mL), CO drops, leading to:
- Increased heart rate (more than 100 bpm).
- Increased respiratory rate (20-30 bpm).
- Respiratory alkalosis and hypoxemia (low PaCO2 and low PaO2).
- Decreased urine output (20-30 ml/h).
- Pale and cool skin with delayed capillary refill.
- Flat jugular veins.
- Progressive stage: fluid loss of 30-40% (1500-2000 mL), compensatory mechanisms fail, resulting in:
- Heart rate exceeding 120 bpm, dysrhythmias, and myocardial ischemia..
- Respiratory distress.
- Respiratory and metabolic acidosis, hypoxemia (high PaCO2, low bicarbonate, low PaO2).
- Oliguria.
- Ashen, cold, and clammy skin with marked delayed capillary refill.
- Lethargy due to declining cerebral perfusion.
- Refractory stage: fluid loss exceeding 40% (2000 mL), compensatory mechanisms collapse, leading to:
- Severe tachycardia and hypotension.
- Absent peripheral pulses and capillary refill.
- Cyanotic and diaphoretic skin.
- Unresponsiveness, and multiple organ system failure manifestations.
Hemodynamic Parameters in Hypovolemic Shock
- Reduced CO and cardiac index.
- Decreased preload (reduced CVP, RAP, PAOP).
- Increased afterload (elevated SVR).
- Lowered MAP.
Management of Hypovolemic Shock
- Focus on addressing the cause of hypovolemia and restoring circulatory volume.
- Methods include:
- Stopping fluid loss.
- Administering fluids (crystalloids, colloids, blood products).
- Monitoring for fluid overload.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the critical concepts surrounding shock, including its definition, classification into hypovolemic, cardiogenic, and distributive types, and the stages of shock. Learn how tissue perfusion and metabolic alterations affect the body in this essential medical overview.