Podcast
Questions and Answers
Which reproductive structure is the primary site of spermatogenesis, where spermatozoa are produced?
Which reproductive structure is the primary site of spermatogenesis, where spermatozoa are produced?
- Interstitial cells of Leydig
- Vas deferens
- Epididymis
- Seminiferous tubules (correct)
What role do Sertoli cells play within the seminiferous tubules?
What role do Sertoli cells play within the seminiferous tubules?
- Providing nutrients and hormones for spermatogenesis (correct)
- Storing and maturing sperm
- Propelling sperm to the ejaculatory duct
- Producing testosterone
Which component of seminal vesicle secretions serves as the primary energy source for sperm?
Which component of seminal vesicle secretions serves as the primary energy source for sperm?
- Prostaglandins
- Potassium
- Phosphorous
- Fructose (correct)
What characteristic appearance does flavin impart to semen and how is this visualized?
What characteristic appearance does flavin impart to semen and how is this visualized?
What is the primary function of prostatic fluid secretions in semen?
What is the primary function of prostatic fluid secretions in semen?
Azoospermia, characterized by a low percentage of live and a high percentage of immotile or dead spermatozoa in semen, is often a result of bilateral or unilateral hypotrophic testes and possibly secondary to hypothyroidism.
Azoospermia, characterized by a low percentage of live and a high percentage of immotile or dead spermatozoa in semen, is often a result of bilateral or unilateral hypotrophic testes and possibly secondary to hypothyroidism.
Why is the collection of the first portion of the ejaculate considered more critical for semen analysis?
Why is the collection of the first portion of the ejaculate considered more critical for semen analysis?
What effect does a prolonged period of sexual abstinence typically have on semen characteristics?
What effect does a prolonged period of sexual abstinence typically have on semen characteristics?
Which method of semen collection is generally associated with lower quality samples?
Which method of semen collection is generally associated with lower quality samples?
When collecting a semen sample for analysis, the patient should always empty their bladder before ejaculation because urine is toxic to sperm.
When collecting a semen sample for analysis, the patient should always empty their bladder before ejaculation because urine is toxic to sperm.
Why are ordinary latex condoms unacceptable for semen collection?
Why are ordinary latex condoms unacceptable for semen collection?
What initial step is recommended if a semen sample does not completely liquefy within the standard observation period?
What initial step is recommended if a semen sample does not completely liquefy within the standard observation period?
Which range on the viscosity reporting scale indicates that semen is gel-like?
Which range on the viscosity reporting scale indicates that semen is gel-like?
What does a rusty red or red-brown color in semen typically indicate?
What does a rusty red or red-brown color in semen typically indicate?
What does increased pH in semen indicate?
What does increased pH in semen indicate?
At what magnification is the initial microscopic examination of semen typically performed to assess sperm number and other cellular components?
At what magnification is the initial microscopic examination of semen typically performed to assess sperm number and other cellular components?
Why should the semen sample not be mixed vigorously when preparing a wet mount for microscopic examination?
Why should the semen sample not be mixed vigorously when preparing a wet mount for microscopic examination?
What specific criterion defines agglutination of spermatozoa in semen analysis?
What specific criterion defines agglutination of spermatozoa in semen analysis?
What does the presence of ciliary tufts in a semen sample indicate?
What does the presence of ciliary tufts in a semen sample indicate?
Within what timeframe should sperm motility be assessed after semen liquefaction to ensure accurate results?
Within what timeframe should sperm motility be assessed after semen liquefaction to ensure accurate results?
Match each sperm motility grading (WHO criteria) with its corresponding description:
Match each sperm motility grading (WHO criteria) with its corresponding description:
The normal lower reference limit for total sperm number is ≥ __________ x10^6/ejaculate.
The normal lower reference limit for total sperm number is ≥ __________ x10^6/ejaculate.
A semen sample is diluted 1:20, and after counting, the average number of spermatozoa per HPF is determined to be >101. What is the next step for processing this sample?
A semen sample is diluted 1:20, and after counting, the average number of spermatozoa per HPF is determined to be >101. What is the next step for processing this sample?
According to Kruger's Strict criteria, what percentage of sperm should exhibit normal morphology for a semen sample to be considered within normal limits?
According to Kruger's Strict criteria, what percentage of sperm should exhibit normal morphology for a semen sample to be considered within normal limits?
Which of the following is NOT a reason for seminal fluid analysis?
Which of the following is NOT a reason for seminal fluid analysis?
Phosphorous and Magnesium contributes to sperm motility.
Phosphorous and Magnesium contributes to sperm motility.
What is the clinical significance of detecting ACP in semen?
What is the clinical significance of detecting ACP in semen?
What part of the body regulate the Seminiferous tubules?
What part of the body regulate the Seminiferous tubules?
What is the role of Semenogelin?
What is the role of Semenogelin?
What does the bulbourethral gland add to neutralize what?
What does the bulbourethral gland add to neutralize what?
Which of the following cause Oligospermia?
Which of the following cause Oligospermia?
What is the minimum of days of abstinence?
What is the minimum of days of abstinence?
What affect sperm number and quality?
What affect sperm number and quality?
With prolonged abstinence what happends to volumes?
With prolonged abstinence what happends to volumes?
After the spermatozoa accumulate in the epididymis then where do they overflow and have the tendency to be flushed out in the urine?
After the spermatozoa accumulate in the epididymis then where do they overflow and have the tendency to be flushed out in the urine?
As the epididymis are completely emptied by one ejaculation, some spermatozoa remain from the time of the previous ejaculation.
As the epididymis are completely emptied by one ejaculation, some spermatozoa remain from the time of the previous ejaculation.
What is the best product of sexual activity?
What is the best product of sexual activity?
How many months apart should the fertility test be in?
How many months apart should the fertility test be in?
Before ejaculation, what should be empty because urine is toxic to sperm?
Before ejaculation, what should be empty because urine is toxic to sperm?
In transport what should be contained inside the pocket?
In transport what should be contained inside the pocket?
What type of semen can be used?
What type of semen can be used?
Semen samples may contain non-infectious agents.
Semen samples may contain non-infectious agents.
Flashcards
Seminiferous tubules
Seminiferous tubules
Site of spermatogenesis and spermatozoa production.
Sertoli cells
Sertoli cells
Cells that supply nutrients and hormones for normal spermatogenesis.
Epididymis
Epididymis
Storage and sperm maturation; sperm gain motility until ejaculation
Interstitial cells of Leydig
Interstitial cells of Leydig
Signup and view all the flashcards
Vas / Ductus deferens
Vas / Ductus deferens
Signup and view all the flashcards
Seminal vesicle
Seminal vesicle
Signup and view all the flashcards
Fructose
Fructose
Signup and view all the flashcards
Flavin
Flavin
Signup and view all the flashcards
Bulbourethral gland
Bulbourethral gland
Signup and view all the flashcards
Azoospermia
Azoospermia
Signup and view all the flashcards
Oligospermia
Oligospermia
Signup and view all the flashcards
Necrozoospermia
Necrozoospermia
Signup and view all the flashcards
Asthenozoospermia
Asthenozoospermia
Signup and view all the flashcards
Fertility testing, Postvasectomy semen analysis,Forensic analyses
Fertility testing, Postvasectomy semen analysis,Forensic analyses
Signup and view all the flashcards
Abstinence (Semen)
Abstinence (Semen)
Signup and view all the flashcards
Semi-solid coagulated mass
Semi-solid coagulated mass
Signup and view all the flashcards
Liquefaction
Liquefaction
Signup and view all the flashcards
Small discrete drops
Small discrete drops
Signup and view all the flashcards
Homogeneous, grey-opalescent, translucent
Homogeneous, grey-opalescent, translucent
Signup and view all the flashcards
1.5 – 5 mL
1.5 – 5 mL
Signup and view all the flashcards
Musty, bleach-like odor
Musty, bleach-like odor
Signup and view all the flashcards
7.2 – 8.0 pH semen
7.2 – 8.0 pH semen
Signup and view all the flashcards
Phase contrast microscope
Phase contrast microscope
Signup and view all the flashcards
Initial Microscopic Examination
Initial Microscopic Examination
Signup and view all the flashcards
Progressive Motility (PR)
Progressive Motility (PR)
Signup and view all the flashcards
Non-progressive Motility (NP)
Non-progressive Motility (NP)
Signup and view all the flashcards
Immotile
Immotile
Signup and view all the flashcards
Sperm Mobility Percentage
Sperm Mobility Percentage
Signup and view all the flashcards
Agglutination of Spermatozoa
Agglutination of Spermatozoa
Signup and view all the flashcards
Cellular Elements in Semen
Cellular Elements in Semen
Signup and view all the flashcards
How to calculate sperm concentration
How to calculate sperm concentration
Signup and view all the flashcards
Total Sperm Count
Total Sperm Count
Signup and view all the flashcards
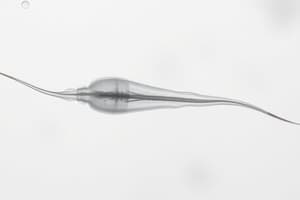
Normal Sperm
Normal Sperm
Signup and view all the flashcards
Study Notes
- Seminal fluid is another type of body fluid
Objectives
- The function of reproductive structures for seminal fluid formation can be described
- Composition of seminal fluid can be discussed
- Seminal fluid analysis can be described including collection, physical, chemical and microscopic evaluation
- Morphologic appearance of normal and abnormal forms of spermatozoa can be described and identified
- The origin and clinical significance of cells other than sperm in the seminal fluid can be discussed
Clinical Significance
- Reasons for seminal fluid analysis include fertility testing, and postvasectomy semen analysis
- Forensic analyses can be conducted including medicolegal cases, and alleged rape
- Seminal fluid analysis can be used for selection of donors for therapeutic insemination, in-vitro fertilization or embryo transfer
- It can be used for exposure screening to reproductive toxicants
- and for cryopreservation or sperm banking
Male Reproductive System
- Male reproductive system includes the ureter, urinary bladder, ductus deferens and seminal vesicle
- Additional components include prostate gland, bulbourethral gland, urethra and epididymis
- The testis, penis and glans penis are also components
- The sagittal section includes the pubic bone, and scrotum
Definition of Terms
- Seminiferous tubules are the site of spermatogenesis and spermatozoa production and regulated by Sertoli cells
- Sertoli cells play a role in supplying nutrients, hormones and other necessary substances for spermatogenesis or nurse cells for developing sperms
- The epididymis is where sperm maturation and storage occurs, and where sperm gain motility before ejaculation
- Interstitial cells of Leydig produce and secrete testosterone
- The vas/ ductus defens propels sperm to the ejaculatory duct
- Seminal vesicles makes up 60-70% of seminal fluid, provides nutrients such as fructose for sperm, alkaline fluid, fructose, prostaglandins and flavin
- Fructose provides energy for sperm
- Flavin imparts the characteristic gray or opalescent to light yellow, and green-white fluorescence under UV
- Prostaglandin lowers the female immune response to the semen.
- Phosphorous and potassium contributes to sperm motility
- Proteins play a role in coagulation of ejaculate, creating a gel-like protective layer around sperm
- The prostate gland contributes 20-30% to seminal fluid
- Prostatic fluid secretions aid coagulation and liquefaction
- Principal components of the milky, slightly acidic fluid: citric acid, enzymes (ACP and proteolytic enzymes), and proteins for coagulation
- ACP can be used to identify semen
- Proteolytic enzyme can be used for liquefaction
- Zinc is used to evaluate prostate function and a decreased level of zinc is associated with the prostate gland disorders
- Bulbourethral gland contributes 5% and adds alkaline mucus to neutralize prostatic acid and vaginal acidity
- Azoospermia describes the total absence of sperm cells that results from bilaterally small, underdeveloped testes, ejaculatory obstruction from traumatic or operative procedures or secondary to gonorrhea
- Oligospermia is characterized by presence of a few motile cells and low sperm count from bilateral or unilateral hypotrophic testes; and may be secondary to hypothyroidism
- Necrozoospermia describes a condition in which there is a low percentage of live and a high percentage of immotile or dead spermatozoa in semen
- Asthenozoospermia describes inability of vital sperm cells to move. (slow moving sperm cells or "lazy" sperm cells)
Factors Affecting Semen Quality
- The 1st portions of semen are prostatic secretions rich in sperm cells
- If a portion of the initial ejaculate is not collected, there is decreased volume, decreased sperm concentration, and increased pH
- If the semen coagulum will fails to liquefy
- Later fractions/last portion contains seminal vesicular fluid
- If the last portion of ejaculate is missing there is decreased semen volume, increased sperm contraction and a coagulation will not form
- Losing the first portion of the ejaculate has more influence on the results of semen analysis than losing the last portion
- Increased volume of seminal fluid enhances sperm motility = dilution may occur and underestimate sperm concentration
- Abstinence for a minimum of 2 days is needed
- Lacking at least 2 days of abstinence can affect sperm number and quality
- Abstinence for a maximum of 7 days is needed
- Prolonged abstinence increases volumes and reduces motility or increases flavin
- Absence of ejaculation causes spermatozoa to accumulate in the epididymis, overflow into the urethra and have tendency to be flushed into the urine
- Penultimate abstinence period can affect sperm count, as a single ejaculation will not clear all sperm cells
- As the epididymis are not completely emptied by ejaculation with some spermatozoa remain from the previous
- The size of the testis influences the total number of spermatozoa per ejaculate
- Size also reflects the level of sperm activity which also affects sperm, morphology
- Takiara demonstrated that the size of the testes bears a direct correlation with testicular function
- The product of masturbation correlates to a lower quality, in a room near laboratory; sperm
- Product of sexual activity corresponds to higher quality. Condoms during intercourse
Specimen Collection
- Instructions should be clearly written and spoken concerning the collection of the sample. Ensure the sample is complete and any loss of any fraction of the sample should be reported
- Abstinence for a minimum of 2 days, and a maximum of 7 days of sexual abstinence is needed
- The collection site should be a private room near the laboratory to limit the exposure of the semen to fluctuations in temperature and to control the time between collection and analysis
- Report form should document the name of the patient and date of birth, period of abstinence and date/time of collection
- Additional information should include completeness of sample (any producing difficulties), and the time interval between collection, and the start of semen analysis
- Complete collection is needed, the bladder should be empty before ejaculation, as urine is toxic to sperm
- 2-3 samples within a 3-month period and at least 7 days apart should be examined for fertility testing
- A clean wide mouthed container made of glass or plastic that has been confirmed to be non-toxic for spermatozoa should be used for collection
- A pre-weighed container can be labeled with the name and ID number of the subject
- Transport to and preserve the sample, in the laboratory within one hour of collection
- Keep sample at ambient temperature between 20 and 37 degrees celsius (close to body temp) while waiting for analysis
- Artificial insemination requires samples to be preserved and frozen at -85 degrees Celsius
- The best collection method is masturbation, or a nonlubricated rubber or polyurethane condom
- Ordinary latex condoms are not acceptable because they interfere with the motility of spermatozoa
- Coitus interruptus: not a reliable method as the first portion of ejaculation contains highest number of spermatozoa
- The low pH of vaginal fluid affects sperm motility
- Vaginal vault aspiration: Seminal fluid from the vaginal vault after coitus
- Semen samples may contain infectious agents such as HIV, HBV, and herpes simplex virus
- Handle specimens as biohazards and discard as waste
- Use sterile materials and techniques for bioassay, intra-uterine insemination, in-vitro fertilization or intracytoplasmic sperm injection
Physical Examination
- Semen analysis should begin within 30 to 60 minutes right after liquefaction
- Liquefaction happens immediately after ejaculation forming a semi-solid coagulated mass
- At room temperature, semen usually begins to liquefy (become thinner), with a heterogeneous mixture of lumps in the fluid
- Normal samples may contain jellylike granules, but mucus strands interfere with semen analysis
- Failure of liquefaction can be caused by deficiency in prostatic enzymes and should be reported
- Adding an equal volume of Dulbecco’s phosphate -buffered saline, followed by pipetting can aid in liquefaction
- Reducing inhomogeneity: Repeated gentle passage through gauge 18/19 attached to syringes
- Viscosity
- Normal viscosity is defined by small discrete drops
- Abnormal viscousity is defined by thread >2 cm long causing interference with sperm motility/concentration
- viscosity is reported using values 0 or 4
- 0: Watery
- 4: Gel-like
- Alternate reporting: normal is slightly viscous, moderately viscous or unable to aspirate into pipette
- Color and Appearance
- Homogeneous, grey-opalescent appearance is normal
- Normal
- Turbid = WBCs (infection)
- Rusty red/red-brown = RBCs (hemospermia)/drugs like pyridium
- Yellowish = Flavin (prolonged abstinence) + urine contamination, jaundice, multivitamins
- Clear = infertility
- Volume:
- 1.5 - 5 mL is normal
- Low (hypospermia)
- Infertility, Ejaculatory duct obstruction, absence of vas deferens, loss during collection, androgen deficiency
- Active inflammation, prolonged abstinence is high
- Volume is measured by weighing pre-weighed container
- OR collecting sample into tube/cylinder
- Volume in mL can be derived: Weight in mL/ Density in g/mL. Semen density=1g/mL ranges 1.043-1.102 g/mL
- Odor
- Odor should be distinct musty/bleach-like
- Abnormal means something infectious
Chemical Examination
- pH
- pH ranges between 7.2 - 8.0
- Infections cause elevated pH in reproductive tract (bacteria=alkaline)
- Decreased pH comes from ejaculatory duct obstruction OR increased secretions
Microscopic Examination
- phase contrast microscope is recommended for all examinations of unstained preparations of fresh semen at a total magnification of x400 (at x1000 if stained preparation)
- Microscopic examination of semen involves sperm motility, vitality, concentration and morphology
- Inspected at a total magnification of x100; LPO
- Provides an overview of the sample, especially the number of spermatozoa, the presence of mucus strands, sperm agglutination or aggregation
- Determines cells other than spermatozoa (epithelial and round cells) leukocyes/germ cells
- Wet prep: Semen sample mixed well and the components are distributed
- It is mixed 10 times by aspirating with disposable pipette
- aliquot of semen (10 ul) is added after mixing
- transferred to a clean side with coverslip
- fixed depth of 20 mm to allow spermatoza to swim freely
- rotating movement is constrained at <20 mm
- Aggregation is the adherence of either immotile/motile spermatozoa to other
- Agglutination: Refers to motile spermatozoa sticking
Sperm Motility
- Graded traditionally: Examining in an undiluted specimen, determining percentage and quality
- Graded using computer-spermed analysis(CASA)
- Evaluate immediately for liquefication of sample-preferably within 30m/1hr. Standardization
- Performed at rm temp or 37 deg- may need to standardize based on each lab
- Rapid progression, some lateral movement
- B is slower, some lateral movement
- C is noticeable lateral and slow
- Progressive motility: Spermatozoa move in a line/large circle in a steady fashion
- Non-progressive motility: sperm exhibits movement by either small circles and force barely displaces head/observation of flagella
Sperm Concentration
- Locate grid to check there should be 5 squares
- Dilutions need to be carried out based on the average # if Spermatoza
- average less than 101= 1:20(50 mL in 950ul fixative)
- Normal values limits (WHO). Number over 15 x 10^6/mL.
- Total value over 39 x 10^6/ejaculate Calculations
- Sperm concentration (per ml) = Total # rows (R1+R2)/Total number of cells X VCFxDF
- Df- dilution factors= total of solution / volume. VCF( volume correction factor)- Vol wanted/ volume used Sperm #- Sperm concentration x semen vol
Sperm Morphology
- Kruger's strict # is 14%. Routine criteria # >= 4%. Can have defects to tails, neck, cytoplasm.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.