Podcast
Questions and Answers
What is a notable symptom of active synovitis?
What is a notable symptom of active synovitis?
- Improved range of motion in the morning
- Warm, swollen, and tender joints (correct)
- Stable joint alignment
- Asymmetrical joint involvement
Which deformity is associated with ulnar deviation of the fingers?
Which deformity is associated with ulnar deviation of the fingers?
- Boutonniere deformity (correct)
- Hammer toe
- Claw hand
- Swan neck deformity (correct)
What is a common clinical criterion for diagnosing rheumatoid arthritis?
What is a common clinical criterion for diagnosing rheumatoid arthritis?
- Elevated levels of cholesterol
- Presence of morning stiffness lasting more than an hour (correct)
- Score of 4 or more on a pain questionnaire
- Asymmetrical joint involvement
Which of the following is an extra-articular manifestation of rheumatoid arthritis?
Which of the following is an extra-articular manifestation of rheumatoid arthritis?
What is the first line treatment for rheumatoid arthritis?
What is the first line treatment for rheumatoid arthritis?
Which of the following is characteristic of CREST syndrome?
Which of the following is characteristic of CREST syndrome?
What radiological finding is not typically associated with osteoarthritis?
What radiological finding is not typically associated with osteoarthritis?
What distinguishes septic arthritis from other types of arthritis?
What distinguishes septic arthritis from other types of arthritis?
What is one of the key characteristics of rheumatoid arthritis in terms of joint involvement?
What is one of the key characteristics of rheumatoid arthritis in terms of joint involvement?
What is the primary role of anti-nuclear antibodies (ANA) in the assessment of connective tissue diseases?
What is the primary role of anti-nuclear antibodies (ANA) in the assessment of connective tissue diseases?
Which of the following antibodies is specifically monitored to assess disease activity in systemic lupus erythematosus (SLE)?
Which of the following antibodies is specifically monitored to assess disease activity in systemic lupus erythematosus (SLE)?
What environmental factors are associated with the development of rheumatoid arthritis?
What environmental factors are associated with the development of rheumatoid arthritis?
Which of the following statements regarding rheumatoid arthritis is accurate?
Which of the following statements regarding rheumatoid arthritis is accurate?
What is citrullination, and why is it relevant to rheumatoid arthritis?
What is citrullination, and why is it relevant to rheumatoid arthritis?
In rheumatoid arthritis, what is primarily attacked by autoantibodies?
In rheumatoid arthritis, what is primarily attacked by autoantibodies?
What distinguishes rheumatoid arthritis from osteoarthritis in terms of disease progression?
What distinguishes rheumatoid arthritis from osteoarthritis in terms of disease progression?
What is the primary function of the conducting zone in the respiratory system?
What is the primary function of the conducting zone in the respiratory system?
Which structure is directly involved in gas exchange in the respiratory system?
Which structure is directly involved in gas exchange in the respiratory system?
Which component of the respiratory system is responsible for producing mucus?
Which component of the respiratory system is responsible for producing mucus?
What characterizes bronchospasm in the respiratory system?
What characterizes bronchospasm in the respiratory system?
How does acetylcholine affect airway smooth muscle?
How does acetylcholine affect airway smooth muscle?
During inhalation, what happens to the diaphragm?
During inhalation, what happens to the diaphragm?
What anatomical feature differentiates the left lung from the right lung?
What anatomical feature differentiates the left lung from the right lung?
What role do the pleural membranes serve in the respiratory system?
What role do the pleural membranes serve in the respiratory system?
Which process helps to equalize air to body temperature as it enters the respiratory tract?
Which process helps to equalize air to body temperature as it enters the respiratory tract?
What is the primary mechanism leading to recurrent episodes of gout in most patients?
What is the primary mechanism leading to recurrent episodes of gout in most patients?
Which of the following treatments is appropriate for acute gout attacks?
Which of the following treatments is appropriate for acute gout attacks?
Which characteristic rash is associated with Systemic Lupus Erythematosus (SLE)?
Which characteristic rash is associated with Systemic Lupus Erythematosus (SLE)?
In which scenario is IV Vancomycin typically administered?
In which scenario is IV Vancomycin typically administered?
What is the primary protein deficiency observed in Duchenne Muscular Dystrophy?
What is the primary protein deficiency observed in Duchenne Muscular Dystrophy?
Which condition is characterized by an autoimmune response targeting postsynaptic acetylcholine receptors?
Which condition is characterized by an autoimmune response targeting postsynaptic acetylcholine receptors?
Which of the following signs is indicative of progressive muscular dystrophy, particularly Duchenne Muscular Dystrophy?
Which of the following signs is indicative of progressive muscular dystrophy, particularly Duchenne Muscular Dystrophy?
What is the most common infectious agent associated with septic arthritis in a sexually active young patient?
What is the most common infectious agent associated with septic arthritis in a sexually active young patient?
What is the goal serum uric acid level in the treatment of chronic gout?
What is the goal serum uric acid level in the treatment of chronic gout?
Which of the following is a treatment option to increase urinary uric acid excretion?
Which of the following is a treatment option to increase urinary uric acid excretion?
What is a primary characteristic of Acute Respiratory Distress Syndrome (ARDS)?
What is a primary characteristic of Acute Respiratory Distress Syndrome (ARDS)?
Which of the following causes can lead to direct lung injury in ARDS?
Which of the following causes can lead to direct lung injury in ARDS?
Which symptom is NOT associated with pneumonia?
Which symptom is NOT associated with pneumonia?
In assessing pediatric asthma, which question is least relevant?
In assessing pediatric asthma, which question is least relevant?
What factor would determine the severity of ARDS in relation to PaO2/fiO2 ratio?
What factor would determine the severity of ARDS in relation to PaO2/fiO2 ratio?
Which response does NOT describe a role of neutrophils in ARDS?
Which response does NOT describe a role of neutrophils in ARDS?
Which statement regarding wheezing in pediatric patients is accurate?
Which statement regarding wheezing in pediatric patients is accurate?
Which is NOT a typical clinical assessment question for wheezing in children?
Which is NOT a typical clinical assessment question for wheezing in children?
Which of the following is a characteristic of chronic asthma?
Which of the following is a characteristic of chronic asthma?
What indicates a status asthmaticus condition?
What indicates a status asthmaticus condition?
Which factor is NOT a predisposing factor for asthma?
Which factor is NOT a predisposing factor for asthma?
In COPD patients, which symptom is typically associated with chronic bronchitis?
In COPD patients, which symptom is typically associated with chronic bronchitis?
Which of the following is a diagnostic tool for confirming asthma?
Which of the following is a diagnostic tool for confirming asthma?
What distinguishes a 'Blue Bloater' phenotype in COPD?
What distinguishes a 'Blue Bloater' phenotype in COPD?
What is a common characteristic of cough variant asthma?
What is a common characteristic of cough variant asthma?
Which of the following is true regarding the pathology of COPD?
Which of the following is true regarding the pathology of COPD?
What is the primary cause of tuberculosis?
What is the primary cause of tuberculosis?
Which of the following lung function changes is characteristic of asthma diagnosis?
Which of the following lung function changes is characteristic of asthma diagnosis?
Which of the following accurately describes a characteristic of chronic asthma?
Which of the following accurately describes a characteristic of chronic asthma?
What defines Status Asthmaticus?
What defines Status Asthmaticus?
Which of the following factors is NOT a predisposing factor for asthma?
Which of the following factors is NOT a predisposing factor for asthma?
Which of the following is a primary symptom of COPD?
Which of the following is a primary symptom of COPD?
Which method is commonly used to confirm the diagnosis of asthma?
Which method is commonly used to confirm the diagnosis of asthma?
What is a distinguishing feature of 'Brittle Asthma'?
What is a distinguishing feature of 'Brittle Asthma'?
How is COPD primarily differentiated from asthma?
How is COPD primarily differentiated from asthma?
Which symptom would most likely be associated with pneumonia rather than asthma?
Which symptom would most likely be associated with pneumonia rather than asthma?
What sign might indicate cor pulmonale in a patient with COPD?
What sign might indicate cor pulmonale in a patient with COPD?
Which age group is least likely to have asthma as a primary diagnosis for wheezing?
Which age group is least likely to have asthma as a primary diagnosis for wheezing?
Which of the following factors is NOT part of Virchow’s triad concerning venous thromboembolism (VTE)?
Which of the following factors is NOT part of Virchow’s triad concerning venous thromboembolism (VTE)?
What is the primary method used to assess the probability of pulmonary embolism?
What is the primary method used to assess the probability of pulmonary embolism?
In the evaluation of pulmonary embolism, a negative D-dimer test indicates what?
In the evaluation of pulmonary embolism, a negative D-dimer test indicates what?
Which ECG finding is considered pathognomonic for right heart strain due to pulmonary embolism?
Which ECG finding is considered pathognomonic for right heart strain due to pulmonary embolism?
What is a common characteristic of primary spontaneous pneumothorax?
What is a common characteristic of primary spontaneous pneumothorax?
Which laboratory finding is likely to be elevated in patients with moderate-to-large pulmonary emboli?
Which laboratory finding is likely to be elevated in patients with moderate-to-large pulmonary emboli?
Which condition would NOT typically contribute to the elevation of D-dimer levels?
Which condition would NOT typically contribute to the elevation of D-dimer levels?
What distinguishes traumatic pneumothorax from spontaneous pneumothorax?
What distinguishes traumatic pneumothorax from spontaneous pneumothorax?
What is the typical room-air oxygen saturation level indicating hypoxemia?
What is the typical room-air oxygen saturation level indicating hypoxemia?
Which of the following statements about respiratory alkalosis is correct?
Which of the following statements about respiratory alkalosis is correct?
What is the primary mechanism by which reactivated disease occurs in individuals?
What is the primary mechanism by which reactivated disease occurs in individuals?
Which condition is NOT a likely cause for unilateral wheezing?
Which condition is NOT a likely cause for unilateral wheezing?
What genetic mutation is most commonly seen in cystic fibrosis patients?
What genetic mutation is most commonly seen in cystic fibrosis patients?
In which situation is a chest X-ray least likely to be indicated?
In which situation is a chest X-ray least likely to be indicated?
Which of the following conditions is most closely associated with chronic inflammation of the lungs?
Which of the following conditions is most closely associated with chronic inflammation of the lungs?
What factor most significantly increases the risk of lung cancer?
What factor most significantly increases the risk of lung cancer?
Which characteristic is indicative of Type 1 respiratory failure?
Which characteristic is indicative of Type 1 respiratory failure?
Which of the following findings is typically NOT associated with cystic fibrosis?
Which of the following findings is typically NOT associated with cystic fibrosis?
What is the main cause of airway secretions becoming extremely thick in cystic fibrosis?
What is the main cause of airway secretions becoming extremely thick in cystic fibrosis?
Which of the following does NOT typically contribute to respiratory failure?
Which of the following does NOT typically contribute to respiratory failure?
What is the most immediate treatment for a tension pneumothorax in an unstable patient?
What is the most immediate treatment for a tension pneumothorax in an unstable patient?
Which criterion is NOT a characteristic of stable patients with pneumothorax?
Which criterion is NOT a characteristic of stable patients with pneumothorax?
What is the primary initial step in managing a primary spontaneous pneumothorax?
What is the primary initial step in managing a primary spontaneous pneumothorax?
In which scenario would surgical management be indicated for pneumothorax?
In which scenario would surgical management be indicated for pneumothorax?
What is the main consequence of a tension pneumothorax on venous return?
What is the main consequence of a tension pneumothorax on venous return?
What is the anatomical site for needle decompression in a tension pneumothorax?
What is the anatomical site for needle decompression in a tension pneumothorax?
Which of the following is an indication for video-assisted thoracic surgery (VATS) in managing pneumothorax?
Which of the following is an indication for video-assisted thoracic surgery (VATS) in managing pneumothorax?
Which of the following is considered a potential complication of untreated tension pneumothorax?
Which of the following is considered a potential complication of untreated tension pneumothorax?
Study Notes
Connective Tissue Diseases and Rheumatology
- Labs for Assessing Connective Tissue Diseases (CTDs): Includes anti-nuclear antibody (ANA) testing; clinical diagnosis is crucial as labs are not definitive.
- ANA (Antinuclear Antibody): Broadly screens for CTDs, excluding RA; a positive result may indicate aging or various diseases, including HIV and malignancies.
- SLE: Involves specific antibodies like dsDNA. Disease activity is monitored via titers; Anti-smith has decreased sensitivity.
- RA vs. OA:
- Rheumatoid Arthritis (RA): Features symmetrical joint involvement, especially in hands. Characterized by cartilage loss, bone erosion, and involves synovium.
- Osteoarthritis (OA): Involves complex risk factors including obesity and age, with x-ray findings showing narrowed joint space and osteophytes.
- Rheumatoid Arthritis Symptoms: Morning stiffness lasting over an hour, symmetrical swelling in joints, potential for complications like Felty’s syndrome.
- Environmental Triggers for RA: Smoking and infections can exacerbate the condition.
- Extrarticular Manifestations of RA: Include cardiovascular issues, various forms of vasculitis, and systemic effects like anemia.
- RA Treatment: NSAIDs as first-line; DMARDs like methotrexate, glucocorticoids for symptom management, and biologics for severe cases.
CREST Syndrome
- Definition: Limited scleroderma characterized by calcinosis, Raynaud's phenomenon, esophageal dysfunction, sclerodactyly, and telangiectasia.
- Complications: Can lead to pulmonary hypertension affecting heart and respiratory functions.
Gout
- Pathophysiology: Caused by uric acid accumulation, often due to renal excretion issues; acute, inflammatory arthritis defined by hyperuricemia (>6.8 mg/dL).
- Chronic Gout Treatment: Includes allopurinol; target serum uric acid less than 6 mg/dL. Tophi formation signifies aggravated condition.
Systemic Lupus Erythematosus (SLE)
- Key Features: Autoantibody disease with symptoms like butterfly rash, oral ulcers, and potential vasculitis presenting with purpura.
- Demographics: More common in women, especially African Americans.
- Lupus Treatment: IV/oral steroids, NSAIDs, hydroxychloroquine for arthritis, and cytotoxic immunosuppressants for severe organ damage.
Myasthenia Gravis
- Pathophysiology: Autoimmune disorder targeting acetylcholine receptors; characterized by muscle weakness, especially bulbar symptoms like ptosis and dysphagia.
- Presentation: Fatigue, respiratory failure; differentiated into generalized and ocular forms.
Duchenne Muscular Dystrophy
- Characteristics: Genetic condition affecting dystrophin; manifests with progressive weakness, often wheelchair dependence by ages 10-12.
- Diagnosis: Identified by elevated serum creatine kinase levels, presents with muscle fiber necrosis, and Gowers' sign.
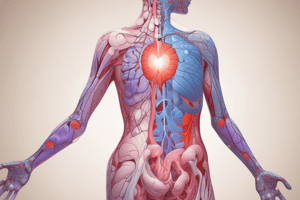
Respiratory System Overview
- Breathing Control: Involves the pulmonary, musculoskeletal, and cardiac systems’ coordination; structures include conducting and respiratory zones.
- Bronchospasm and Inflammation: Inflammation can cause constriction of airway smooth muscle; role of acetylcholine in promoting bronchoconstriction via muscarinic receptors.
- Acute Respiratory Distress Syndrome (ARDS): Characterized by severe hypoxemia, bilateral infiltrates, and cytokine release; arises from pulmonary or extrapulmonary indirect injury.
- Pneumonia Symptoms: Includes systemic symptoms like fever, cough, and purulent sputum; physical examination reveals crackles and pleural rubs.
Asthma and COPD
- Asthma: Chronic inflammatory disease characterized by reversible airways obstruction; common triggers include allergens and irritants.
- COPD: Includes conditions like chronic bronchitis and emphysema, characterized by chronic inflammation leading to airway obstruction; symptoms include dyspnea and chronic cough.
- Diagnosis: Utilizes lung function tests such as spirometry; distinctions between “pink puffer” (emphysema) and “blue bloater” (bronchitis) based on clinical presentation.
Pediatric Considerations
- Wheezing Assessment: Age of onset, episodic nature, and response to treatment are crucial in assessing wheezing in children; common causes vary with age group.### Asthma Clinical History
- Most prevalent chronic lung disease globally characterized by chronic airway inflammation and hyperactivity.
- Airway obstruction is typically reversible but can progress to irreversible if poorly managed.
- Predisposing factors include family history, specific genetic markers (e.g., ADAM33 gene), atopy, premature birth, obesity, and exposure to secondhand smoke, recreational drugs, and smoking.
Asthma Subtypes
- Chronic asthma leads to irreversible changes, low FEV1 levels, and dyspnea in older patients.
- Exacerbations are acute worsens triggered by specific stimuli.
- Status Asthmaticus represents a life-threatening state with poor response to treatment.
- Bronchospasm results in increased airway constriction.
- Brittle asthma features rapid, severe exacerbations.
- Steroid-resistant asthma does not respond to corticosteroids.
- Cough variant asthma presents primarily with a mild cough, lacking wheezing.
- Occupational asthma results from inhaling allergens at work.
Diagnosis of Asthma
- Confirmed by showing reversible airway obstruction through treatment response, PEFR recordings, and spirometry before and after bronchodilators.
- Blood tests may reveal eosinophilia and elevated specific IgE levels.
- Chest X-rays can be normal or show hyper-expansion during acute attacks.
- Expiratory obstruction is typically worse than inspiratory, leading to air trapping.
Chronic Obstructive Pulmonary Disease (COPD)
- Second most common lung disease, primarily caused by inhaled irritants leading to airway inflammation and changes over time.
- Common symptoms include progressive dyspnea, chronic productive cough (often with sputum), wheezing, and manifestations of cor pulmonale (e.g., edema, headaches).
- Clinical signs include tachypnea, use of accessory muscles, barrel chest, and decreased bilateral lung expansion.
- Distinction between types:
- Blue Bloater: primarily airway obstruction, chronic type 2 respiratory failure, cyanosis, and edema.
- Pink Puffer: emphysema dominant, muscle wasting, increased respiratory effort, no cyanosis or edema.
Diagnosing COPD
- Diagnosis relies on spirometry, demonstrating obstructive and irreversible changes.
- PEFR often indicates low variability during exacerbations.
- FEV1 decline over time is common; additional assessments may include the PSI risk stratification tool.
Tuberculosis (TB)
- 10% of latent infections may reactivate, primarily caused by Mycobacterium tuberculosis.
- Infection occurs through droplet transmission and primarily affects alveolar macrophages.
- TB presents in pulmonary or extrapulmonary forms, with a Ghon focus indicating infection in the lungs.
- 50% transmission risk occurs even with exposure to an infected individual; key reactivation risk factors include age, immunosuppression (HIV), malnutrition, and smoking.
Wheezing Evaluation
- Bilateral wheezing indicates conditions like asthma and COPD.
- Unilateral wheezing may result from foreign body aspiration, tumors, bronchial compression, or lymphadenopathy.
Chest X-ray Indications
- Used to evaluate conditions associated with various pulmonary diseases, aiding diagnosis.
Cystic Fibrosis
- Affects 4% of Caucasians; autosomal recessive gene causing CFTR mutations leading to thick secretions and lung inflammation.
- Common complications: recurrent infections (notably by Pseudomonas aeruginosa), pancreatic insufficiency, and infertility in males.
- Clinical signs include clubbed fingers, barrel chest, and failure to thrive in infants.
- Diagnosis confirmed via sweat test showing elevated chloride levels.
Lung Cancer Risk Factors
- Strongly linked to smoking, with risk correlating with exposure intensity over time.
- Environmental factors include secondhand smoke, air pollutants (asbestos, radon), and certain pre-existing lung diseases.
Chronic Hypoxemia and Hypercapnia
- Hypoxemia denotes insufficient blood oxygen, while hypercapnia indicates elevated blood carbon dioxide (CO2).
- Respiratory failure is categorized into:
- Type 1 (Hypoxemic): Characterized by low PaO2, common in acute lung diseases.
- Type 2 (Hypercapnic): High PaCO2, potentially coexisting with hypoxemia, often seen in COPD or drug overdose cases.
CPAP Therapy for OSA
- Continuous Positive Airway Pressure (CPAP) machines maintain airway patency during sleep by providing air pressure.
Pulmonary Embolism (PE) Origins and Evaluation
- PE results from thrombus or other substances obstructing pulmonary arteries, with venous stasis, hypercoagulability, and vascular damage as contributing factors (Virchow’s triad).
- Diagnosis often utilizes imaging alongside clinical assessment, pretest probability, and D-dimer levels.
Pneumothorax Types and Management
- Traumatic pneumothorax can be closed (blunt trauma) or open (penetrating injury); spontaneous pneumothorax arises from ruptured blebs.
- Tension pneumothorax is a life-threatening condition requiring immediate chest tube placement to alleviate pressure.
- Stable patients can often be monitored while unstable patients require urgent intervention to stabilize respiratory function.
Treatment Protocols for Pneumothorax
- Small, asymptomatic pneumothoraces can be monitored; large pneumothoraxes may require chest tube placement.
- Surgical interventions may be necessary for recurrent or unresponsive cases, including VATS for pleurodesis and management of underlying conditions.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
Prepare for your rheumatology exam with this comprehensive study guide focusing on labs to assess connective tissue diseases. Explore the complexities of diagnosing conditions such as SLE, RA, and Sjogren's, as well as the significance of anti-nuclear antibodies in clinical diagnosis. Ensure you're well-prepared with key insights into symptoms and differential diagnoses.