Podcast
Questions and Answers
Which type of T-cells release inflammatory mediators that stimulate other inflammatory cells leading to tissue injury in RA?
Which type of T-cells release inflammatory mediators that stimulate other inflammatory cells leading to tissue injury in RA?
- Dendritic cells
- CD4+ T-cells (correct)
- CD8+ T-cells
- Natural Killer cells
Which cytokine is secreted by macrophages and stimulates resident synovial cells to secrete proteases that destroy hyaline cartilage in RA?
Which cytokine is secreted by macrophages and stimulates resident synovial cells to secrete proteases that destroy hyaline cartilage in RA?
- IL-17
- IL-1 (correct)
- TNF
- INF-γ
What is the function of RANKL expressed on activated T cells in RA?
What is the function of RANKL expressed on activated T cells in RA?
- Regulates synovial cell activation
- Stimulates bone resorption (correct)
- Inhibits bone resorption
- Stimulates bone formation
What is the significance of the presence of anti-CCP antibodies in RA?
What is the significance of the presence of anti-CCP antibodies in RA?
What is the function of IgM and IgA auto-antibodies that bind IgG Fc region in RA?
What is the function of IgM and IgA auto-antibodies that bind IgG Fc region in RA?
What is citrulline?
What is citrulline?
What is the significance of the presence of germinal centers with secondary follicles and plasma cells in RA?
What is the significance of the presence of germinal centers with secondary follicles and plasma cells in RA?
What is the typical duration of morning stiffness in rheumatoid arthritis?
What is the typical duration of morning stiffness in rheumatoid arthritis?
Which of the following is NOT a cytokine involved in the pathophysiology of RA?
Which of the following is NOT a cytokine involved in the pathophysiology of RA?
Which of the following is a characteristic wrist finding in rheumatoid arthritis?
Which of the following is a characteristic wrist finding in rheumatoid arthritis?
What is the approximate number of children affected by juvenile idiopathic arthritis in the US?
What is the approximate number of children affected by juvenile idiopathic arthritis in the US?
What is a common feature of systemic arthritis in juvenile idiopathic arthritis?
What is a common feature of systemic arthritis in juvenile idiopathic arthritis?
What is the typical joint distribution in juvenile idiopathic arthritis?
What is the typical joint distribution in juvenile idiopathic arthritis?
What is a complication of long-term use of anti-inflammatory drugs in rheumatoid arthritis?
What is a complication of long-term use of anti-inflammatory drugs in rheumatoid arthritis?
What is the prognosis of juvenile idiopathic arthritis?
What is the prognosis of juvenile idiopathic arthritis?
What is a characteristic feature of oligoarthritis in juvenile idiopathic arthritis?
What is a characteristic feature of oligoarthritis in juvenile idiopathic arthritis?
What is the primary characteristic of pannus formation in rheumatoid arthritis?
What is the primary characteristic of pannus formation in rheumatoid arthritis?
Which of the following cells are NOT typically found in the inflammatory infiltrate in rheumatoid arthritis?
Which of the following cells are NOT typically found in the inflammatory infiltrate in rheumatoid arthritis?
What is the consequence of osteoclastic activity in subchondral bone in rheumatoid arthritis?
What is the consequence of osteoclastic activity in subchondral bone in rheumatoid arthritis?
What is the typical distribution of joint involvement in rheumatoid arthritis?
What is the typical distribution of joint involvement in rheumatoid arthritis?
Which of the following joints are typically affected in rheumatoid arthritis?
Which of the following joints are typically affected in rheumatoid arthritis?
What is the consequence of ankylosis in rheumatoid arthritis?
What is the consequence of ankylosis in rheumatoid arthritis?
What is the typical course of joint damage in rheumatoid arthritis?
What is the typical course of joint damage in rheumatoid arthritis?
What is the characteristic of joint damage in rheumatoid arthritis?
What is the characteristic of joint damage in rheumatoid arthritis?
What is the typical age of onset for asymmetric juvenile idiopathic arthritis?
What is the typical age of onset for asymmetric juvenile idiopathic arthritis?
Which type of juvenile idiopathic arthritis is commonly associated with iridocyclitis and a positive ANA?
Which type of juvenile idiopathic arthritis is commonly associated with iridocyclitis and a positive ANA?
What is the characteristic of rheumatoid-factor positive polyarthritis?
What is the characteristic of rheumatoid-factor positive polyarthritis?
What is the characteristic of enthesitis-related arthropathy?
What is the characteristic of enthesitis-related arthropathy?
What is the hallmark of osteoarthritis?
What is the hallmark of osteoarthritis?
What percentage of the population have some radiological evidence of osteoarthritis by age 65?
What percentage of the population have some radiological evidence of osteoarthritis by age 65?
What is a risk factor for osteoarthritis?
What is a risk factor for osteoarthritis?
What is the characteristic of secondary osteoarthritis?
What is the characteristic of secondary osteoarthritis?
What is the primary reason for rapid joint destruction in infectious arthritis?
What is the primary reason for rapid joint destruction in infectious arthritis?
Which of the following is a risk factor for suppurative infectious arthritis?
Which of the following is a risk factor for suppurative infectious arthritis?
What is the primary mode of bacterial infection in suppurative infectious arthritis?
What is the primary mode of bacterial infection in suppurative infectious arthritis?
Which of the following organisms is commonly associated with suppurative infectious arthritis?
Which of the following organisms is commonly associated with suppurative infectious arthritis?
What is the typical clinical presentation of suppurative infectious arthritis?
What is the typical clinical presentation of suppurative infectious arthritis?
What is a common complication of suppurative infectious arthritis?
What is a common complication of suppurative infectious arthritis?
What is the primary cause of mycobacterial infectious arthritis?
What is the primary cause of mycobacterial infectious arthritis?
What is the mortality rate associated with Staph aureus septic arthritis?
What is the mortality rate associated with Staph aureus septic arthritis?
What is the characteristic of juvenile idiopathic arthritis that develops at an early age and is commonly associated with iridocyclitis and a positive ANA?
What is the characteristic of juvenile idiopathic arthritis that develops at an early age and is commonly associated with iridocyclitis and a positive ANA?
What is the characteristic of rheumatoid-factor positive polyarthritis?
What is the characteristic of rheumatoid-factor positive polyarthritis?
What is the characteristic of enthesitis-related arthropathy?
What is the characteristic of enthesitis-related arthropathy?
What is the primary characteristic of osteoarthritis?
What is the primary characteristic of osteoarthritis?
What percentage of the population have some radiological evidence of osteoarthritis by age 65?
What percentage of the population have some radiological evidence of osteoarthritis by age 65?
What is a risk factor for osteoarthritis?
What is a risk factor for osteoarthritis?
What is the characteristic of secondary osteoarthritis?
What is the characteristic of secondary osteoarthritis?
What is the hallmark of osteoarthritis?
What is the hallmark of osteoarthritis?
What is the primary reason for rapid joint destruction in infectious arthritis?
What is the primary reason for rapid joint destruction in infectious arthritis?
What is a characteristic feature of infectious arthritis caused by Borrelia burgdorferi?
What is a characteristic feature of infectious arthritis caused by Borrelia burgdorferi?
Which of the following is a risk factor for suppurative infectious arthritis?
Which of the following is a risk factor for suppurative infectious arthritis?
What is a common feature of viral infectious arthritis?
What is a common feature of viral infectious arthritis?
What is the primary mode of bacterial infection in suppurative infectious arthritis?
What is the primary mode of bacterial infection in suppurative infectious arthritis?
Which joints are commonly affected in Lyme arthritis?
Which joints are commonly affected in Lyme arthritis?
Which of the following organisms is commonly associated with suppurative infectious arthritis?
Which of the following organisms is commonly associated with suppurative infectious arthritis?
What is a common cause of infectious arthritis?
What is a common cause of infectious arthritis?
What is the typical clinical presentation of suppurative infectious arthritis?
What is the typical clinical presentation of suppurative infectious arthritis?
What is a common complication of suppurative infectious arthritis?
What is a common complication of suppurative infectious arthritis?
What is a characteristic of joint symptoms in infectious arthritis?
What is a characteristic of joint symptoms in infectious arthritis?
What is the primary cause of mycobacterial infectious arthritis?
What is the primary cause of mycobacterial infectious arthritis?
What is a common complication of suppurative infectious arthritis?
What is a common complication of suppurative infectious arthritis?
What is the mortality rate associated with Staph aureus septic arthritis?
What is the mortality rate associated with Staph aureus septic arthritis?
What is the role of HLA-DR4 allele in the pathogenesis of rheumatoid arthritis?
What is the role of HLA-DR4 allele in the pathogenesis of rheumatoid arthritis?
What is the process by which a microbial antigen resembles a self-antigen, leading to autoimmune response?
What is the process by which a microbial antigen resembles a self-antigen, leading to autoimmune response?
What type of cells are activated by Th17 and Th1 cytokines in rheumatoid arthritis?
What type of cells are activated by Th17 and Th1 cytokines in rheumatoid arthritis?
What is the characteristic morphologic feature within the joint in rheumatoid arthritis?
What is the characteristic morphologic feature within the joint in rheumatoid arthritis?
What is the role of citrullination in rheumatoid arthritis?
What is the role of citrullination in rheumatoid arthritis?
What is the result of prominent angiogenesis in the synovium during pannus formation?
What is the result of prominent angiogenesis in the synovium during pannus formation?
Which type of cells are typically found in the inflammatory infiltrate in rheumatoid arthritis?
Which type of cells are typically found in the inflammatory infiltrate in rheumatoid arthritis?
Which joints are most commonly affected in rheumatoid arthritis?
Which joints are most commonly affected in rheumatoid arthritis?
What is the consequence of osteoclastic activity in subchondral bone in rheumatoid arthritis?
What is the consequence of osteoclastic activity in subchondral bone in rheumatoid arthritis?
What is the consequence of environmental factors such as smoking in rheumatoid arthritis?
What is the consequence of environmental factors such as smoking in rheumatoid arthritis?
What is the role of macrophages in the joints of patients with rheumatoid arthritis?
What is the role of macrophages in the joints of patients with rheumatoid arthritis?
What is the typical distribution of joint involvement in rheumatoid arthritis?
What is the typical distribution of joint involvement in rheumatoid arthritis?
What is the characteristic of joint damage in rheumatoid arthritis?
What is the characteristic of joint damage in rheumatoid arthritis?
What is the consequence of ankylosis in rheumatoid arthritis?
What is the consequence of ankylosis in rheumatoid arthritis?
What is the typical course of joint damage in rheumatoid arthritis?
What is the typical course of joint damage in rheumatoid arthritis?
What is the characteristic of joint involvement in rheumatoid arthritis?
What is the characteristic of joint involvement in rheumatoid arthritis?
Flashcards are hidden until you start studying
Study Notes
Rheumatoid Arthritis (RA) - Pathophysiology
- CD4+ T-cells release inflammatory mediators that stimulate other inflammatory cells, leading to tissue injury
- Key cytokines involved:
- INF-γ (secreted by cells, activates macrophages and resident synovial cells)
- IL-17 (from cells, recruits neutrophils and monocytes)
- TNF and IL-1 (from macrophages, stimulates resident synovial cells to secrete proteases that destroy hyaline cartilage)
- RANKL (expressed on activated T cells, stimulates bone resorption)
RA - Pathophysiology Continued
- Joint synovium contains germinal centers with secondary follicles and plasma cells that secrete autoantibodies
- Anti-CCP (anti-citrullinated peptide) detected in serum in up to 70% of patients with RA
- IgM and IgA auto-antibodies that bind IgG Fc region (rheumatoid factor) detected in serum in up to 80% of patients with RA
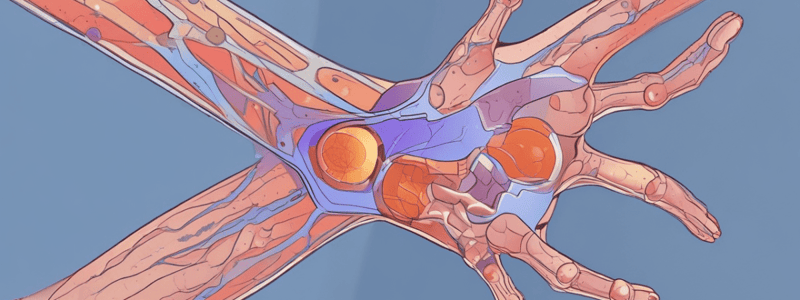
RA - Joint Morphology
- Pannus formation:
- Joint synovium becomes edematous and thickened
- Hyperplasia and proliferation result in transformation from smooth surface to one covered by villous, finger-like projections
- Prominent angiogenesis in the synovium
- Inflammatory cells infiltrate the pannus (CD4+ T helper cells, B cells, plasma cells, dendritic cells, and macrophages)
- Fibrinopurulent exudate is deposited on synovial and joint surfaces
- Osteoclastic activity in subchondral bone causes bony erosion around the joint
RA - Joint Destruction
- Ankylosis:
- Pannus forms a "bridge" between apposing bones, forming a fibrous ankylosis
- Eventual ossification results in a bony ankylosis that "fuses" bones across a joint
- Joint damage encompasses:
- Destruction of cartilage
- Destruction of bone next to the joint
- Damage to joint capsules, tendons, and ligaments
- Ankylosis (decreased range of motion)
Juvenile Idiopathic Arthritis (JIA)
- Heterogeneous group of disorders
- Occur prior to age 16 years and persist for at least 6 weeks
- Idiopathic – no clearly described etiology
- Shares some pathogenic features with RA
- Associated with HLA and PTPN22 gene variants
- 30,000 – 50,000 children affected in the US
Osteoarthritis (OA)
- Characterized by articular cartilage degeneration resulting in structural and functional synovial joint failure
- Can be primary or secondary
- Epidemiology:
- Very common: 80-90% of the population have some radiological evidence of osteoarthritis by age 65
- 50% are significantly affected by osteoarthritis by age 65
- Risk factors include:
- Age, genetics
- Trauma, repetitive use, obesity, other orthopedic disease
- Reproductive hormones
Infectious Arthritis
- Suppurative:
- Bacterial infection entering joints from distant sites via hematogenous spread
- Risk factors: deficiencies in complement factors C5-C9, immunodeficiencies, joint trauma, chronic arthritis, and IV drug use
- Organisms: N.gonorrhea, Chlamydia, Staphylococcus, Streptococcus, H.influenzae, E.coli, Salmonella
- Mycobacterial:
- Chronic progressive monoarticular infections caused by M.tuberculosis
- Occurs primarily in adults as a complication of adjacent osteomyelitis or disseminated from visceral site of infection
Rheumatoid Arthritis (RA)
- Citrullination of proteins can occur within joints, converting arginine amino acids to citrulline
- Proteins that can undergo citrullination include fibrinogen, type II collagen, alpha-enolase, and vimentin
- HLA-DR4 allele is associated with anti-citrulline antibody, and environmental factors like smoking may promote citrullination of self-proteins
Pathogenesis of RA
- Molecular mimicry occurs when a microbial antigen resembles a self-antigen, leading to activation of CD4+ cells that recognize self
- This process is thought to be important in the pathophysiology of autoimmune and hypersensitivity disorders, including RA
Joint Morphology in RA
- RA commonly affects the small joints of the hands and feet, particularly the metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints
- Characteristic morphologic features within the joint include formation of a pannus, which is a mass of edematous synovium, inflammatory cells, granulation tissue, and fibroblast growth causing articular cartilage erosion
Pannus Formation
- Joint synovium becomes edematous and thickened, with hyperplasia and proliferation resulting in transformation from a smooth surface to one covered by villous, finger-like projections into the joint
- Prominent angiogenesis occurs in the synovium
- Inflammatory cells, including CD4+ T helper cells, B cells, plasma cells, dendritic cells, and macrophages, infiltrate the pannus
- Fibrinopurulent exudate is deposited on synovial and joint surfaces
Joint Destruction in RA
- Ankylosis can occur, resulting in a "bridge" of fibrous tissue across the joint that limits range of motion
- Joint damage includes destruction of cartilage, bone, and joint capsules, tendons, and ligaments
- Greatest joint damage occurs in the first 4-5 years, with the younger the age of onset, often the more severe the course of disease
Osteoarthritis (OA)
- Characterized by articular cartilage degeneration, resulting in structural and functional synovial joint failure
- Can be primary or secondary, with primary OA occurring without an apparent initiating cause and secondary OA occurring due to joint deformity, prior injury, or underlying systemic disease
Epidemiology of OA
- Most common joint disease, with 80-90% of the population having some radiological evidence of OA by age 65
- About 5% of cases occur in younger patients, often due to secondary OA
Etiology of OA
- Risk factors include age, genetics, trauma, repetitive use, obesity, and other orthopedic disease
- Reproductive hormones, particularly estrogen, may also play a role
Infectious Arthritis
- Suppurative arthritis occurs when bacteria enter the joint from distant sites via hematogenous spread
- Risk factors include deficiencies in complement factors, immunodeficiencies, joint trauma, chronic arthritis, and IV drug use
- Organisms that can cause infectious arthritis include N. gonorrhea, Chlamydia, Staphylococcus, Streptococcus, H. influenzae, E. coli, and Salmonella
Clinical Features of Infectious Arthritis
- Sudden development of an acutely painful, swollen joint with limited range of motion
- Fever and leukocytosis
- Joint aspiration reveals purulent fluid and identification of the infectious organism
Complications and Prognosis of Infectious Arthritis
- Up to 50% of patients can have long-term joint pain after the infection resolves, even with quick recognition and treatment
- Since it is often associated with sepsis, it can also be associated with severe outcomes, including mortality
Mycobacterial Arthritis
- Chronic progressive monoarticular infections caused by M. tuberculosis
- Occurs primarily in adults as a complication of adjacent osteomyelitis or disseminated from visceral site of infection
- Insidious onset of increasing joint pain, with the hip, knee, and ankle joints commonly affected
Lyme Arthritis
- Caused by the spirochete Borrelia burgdorferi
- If untreated, up to 80% of patients will develop a migratory arthritis lasting weeks to months
- Joint pain is periodic, oligoarticular, and can affect the knees, shoulders, elbows, and ankles
Viral Arthritis
- Can occur with a variety of viral infections, including alphavirus, parovirus B19, rubella, Epstein-Barr, and Hepatitis B & C
- Clinical features include acute to subacute arthritis
- Joint symptoms can be caused by the virus itself or an autoimmune reaction triggered by the infection
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.