Podcast
Questions and Answers
What primary immune response triggers the inflammation in rheumatoid arthritis?
What primary immune response triggers the inflammation in rheumatoid arthritis?
- Recognition of citrullinated self-antigens as foreign (correct)
- Misdirection of immune cells towards healthy tissues
- Deficiency of pro-inflammatory cytokines
- Apoptosis of immune cells
Which demographic group is most commonly diagnosed with rheumatoid arthritis?
Which demographic group is most commonly diagnosed with rheumatoid arthritis?
- Women aged 30 to 70 years (correct)
- Individuals under 30 years of age
- Men aged 70 years and older
- Children and adolescents
What is a characteristic feature of joints affected by rheumatoid arthritis?
What is a characteristic feature of joints affected by rheumatoid arthritis?
- Complete regeneration of cartilage
- Absence of inflammation
- Severe joint deformities and ankylosis (correct)
- Enhanced range of motion
Which environmental factor is associated with an increased risk of developing rheumatoid arthritis?
Which environmental factor is associated with an increased risk of developing rheumatoid arthritis?
What happens during a flare of rheumatoid arthritis?
What happens during a flare of rheumatoid arthritis?
What role do antigen-presenting cells (APCs) play in rheumatoid arthritis?
What role do antigen-presenting cells (APCs) play in rheumatoid arthritis?
Which of these statements about the pathophysiology of rheumatoid arthritis is true?
Which of these statements about the pathophysiology of rheumatoid arthritis is true?
Which reason best explains the significance of the HLA-DR variant alleles in rheumatoid arthritis?
Which reason best explains the significance of the HLA-DR variant alleles in rheumatoid arthritis?
What type of joint involvement is characteristic of rheumatoid arthritis?
What type of joint involvement is characteristic of rheumatoid arthritis?
Which genetic factor is primarily linked with an increased risk of developing rheumatoid arthritis?
Which genetic factor is primarily linked with an increased risk of developing rheumatoid arthritis?
Which modification of self-proteins is recognized as playing a role in the autoimmune response in rheumatoid arthritis?
Which modification of self-proteins is recognized as playing a role in the autoimmune response in rheumatoid arthritis?
What impact do cytokines like TNF, IL-1, and IL-6 have in the context of rheumatoid arthritis?
What impact do cytokines like TNF, IL-1, and IL-6 have in the context of rheumatoid arthritis?
Which autoantibodies play a significant role in the inflammation process associated with rheumatoid arthritis?
Which autoantibodies play a significant role in the inflammation process associated with rheumatoid arthritis?
What term describes the tumor-like growth in joints caused by the proliferation of synovial cells in rheumatoid arthritis?
What term describes the tumor-like growth in joints caused by the proliferation of synovial cells in rheumatoid arthritis?
What is one consequence of rheumatoid arthritis on bone health?
What is one consequence of rheumatoid arthritis on bone health?
What is the preferred disease-modifying antirheumatic drug (DMARD) for rheumatoid arthritis?
What is the preferred disease-modifying antirheumatic drug (DMARD) for rheumatoid arthritis?
What is the mechanism of action of abatacept in the treatment of rheumatoid arthritis?
What is the mechanism of action of abatacept in the treatment of rheumatoid arthritis?
What is the mechanism of action of rituximab in rheumatoid arthritis?
What is the mechanism of action of rituximab in rheumatoid arthritis?
What is the primary mechanism of action of anti-TNF agents (e.g., infliximab, adalimumab) in rheumatoid arthritis?
What is the primary mechanism of action of anti-TNF agents (e.g., infliximab, adalimumab) in rheumatoid arthritis?
Which statement correctly represents the mechanism of action of tofacitinib in the treatment of RA?
Which statement correctly represents the mechanism of action of tofacitinib in the treatment of RA?
Which molecule does tocilizumab specifically target in the treatment of rheumatoid arthritis?
Which molecule does tocilizumab specifically target in the treatment of rheumatoid arthritis?
What role do Janus kinases play in immune response signaling?
What role do Janus kinases play in immune response signaling?
What is a common effect of rituximab treatment in patients with rheumatoid arthritis?
What is a common effect of rituximab treatment in patients with rheumatoid arthritis?
Which of the following is NOT a target for currently used therapies in rheumatoid arthritis?
Which of the following is NOT a target for currently used therapies in rheumatoid arthritis?
What role do activated T helper cells play in the context of rheumatoid arthritis?
What role do activated T helper cells play in the context of rheumatoid arthritis?
Which of the following cytokines is primarily released by activated T cells in the synovium?
Which of the following cytokines is primarily released by activated T cells in the synovium?
What do anti-citrullinated protein antibodies specifically bind to in rheumatoid arthritis?
What do anti-citrullinated protein antibodies specifically bind to in rheumatoid arthritis?
What is the effect of the activation of the complement system by immune complexes in rheumatoid arthritis?
What is the effect of the activation of the complement system by immune complexes in rheumatoid arthritis?
What pathological structure results from the proliferation of synovial cells in rheumatoid arthritis?
What pathological structure results from the proliferation of synovial cells in rheumatoid arthritis?
What is the primary aim of treatment for rheumatoid arthritis?
What is the primary aim of treatment for rheumatoid arthritis?
What is the consequence of the inflammatory cascade in rheumatoid arthritis?
What is the consequence of the inflammatory cascade in rheumatoid arthritis?
Which of the following best describes rheumatoid factors?
Which of the following best describes rheumatoid factors?
Flashcards are hidden until you start studying
Study Notes
Rheumatoid Arthritis Overview
- Rheumatoid Arthritis (RA): A common autoimmune disease marked by chronic joint inflammation due to immune cell activity and pro-inflammatory cytokines.
- Typical Symptoms: Includes symmetrical polyarthritis, affecting five or more small joints (hands and feet) and possibly larger joints; often presents with morning stiffness lasting more than 30 minutes.
- Flare-ups: Sudden worsening of symptoms including swollen, warm, red, and painful joints.
Pathophysiology
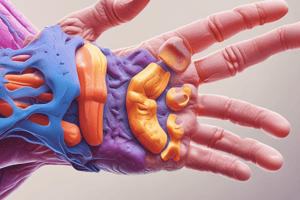
- Joint Damage: Inflammation leads to destruction of bone and cartilage, ankylosis (joint fusion), and severe joint deformities.
- Genetic Factors: Presence of HLA-DR variant alleles (HLA-DR1 and HLA-DR4) increases disease risk, exacerbated by environmental triggers such as smoking or pathogens.
- Citrullination: Modification of self-proteins like Type II collagen converts arginine to citrulline, causing the immune system to mistakenly attack these proteins.
Immune Response Mechanism
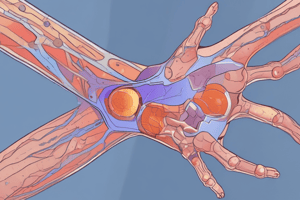
- Citrullinated Antigens: Recognized as foreign by antigen-presenting cells (APCs), activating T helper cells and leading to B cell proliferation producing autoantibodies (ACPAs) and rheumatoid factor (RF).
- Cytokine Release: Activated T-helper cells release Interferon-gamma and IL-17, stimulating macrophages and fibroblasts to release further pro-inflammatory cytokines (TNF, IL-1, IL-6).
- Synovial Inflammation: Pannus formation due to synovial cell proliferation leads to the erosion of bone and cartilage, contributing to joint space narrowing and ankylosis.
Consequences of RA
- Bone Health: Progression includes articular bone loss and systemic osteoporosis, with inhibited bone repair mechanisms.
- Pannus Formation: A "tumor-like growth" that results in cartilage and bone destruction, exacerbating inflammation.
Treatment Strategies
- cDMARDs: Conventional Disease-Modifying Anti-Rheumatic Drugs should be initiated immediately to delay disease progression.
- Combination Therapy: May involve two cDMARDs or adding biological DMARDs (bDMARD) or Janus kinase inhibitors (JAKi) if monotherapy is ineffective.
- NSAIDs or Glucocorticoids: Prescribed for their anti-inflammatory effects as needed.
Key Pharmacological Agents
- Methotrexate: Preferred DMARD; acts as a folic acid antagonist, inhibiting cytokine production. Notable side effects include mucosal ulceration and cytopenias, with folic acid as a supplement to alleviate gastrointestinal and hepatic adverse effects.
- TNF Biologics: Bind to TNF-α, blocking its interaction with receptors to reduce inflammatory response.
- Abatacept: Modulates T-cell activation by binding to CD80/CD86 on APCs, decreasing full T-cell activation.
- Rituximab: Monoclonal antibody targeting CD20; depletes B cells contributing to inflammation.
- Tocilizumab: Monoclonal antibody inhibiting IL-6 receptors, reducing IL-6 activity.
- JAK Inhibitors: Oral drugs disrupting signaling pathways in immune cells, thereby reducing local inflammation.
Exam Questions and Answers
- Typical Initial Presentation: Symmetrical polyarthritis involving five or more small joints.
- Genetic Factors: Increased risk associated with HLA-DR variant alleles.
- Autoimmune Response Modification: Citrullination of Type II collagen triggers immune response.
- Cytokine Role: Promote chronic inflammation and contribute to joint destruction.
- Autoantibodies: ACPAs and rheumatoid factor (RF) activate inflammation through complement activation.
- Tumor-like Growth: Pannus develops due to proliferating synovial cells.
- Bone Health Consequences: RA leads to articular bone loss and systemic osteoporosis.
Mechanism of Action of Drugs
- Abatacept: Modulates T-cell activation by binding to CD80/CD86 on APCs.
- Rituximab: Depletes CD20-positive B cells.
- Anti-TNF Agents: Neutralize TNF-alpha, blocking its interaction with receptors.
- Tofacitinib: Acts as a JAK inhibitor, disrupting immune signaling pathways.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.