Podcast
Questions and Answers
What is the mechanism by which methotrexate exerts its effects in rheumatoid arthritis?
What is the mechanism by which methotrexate exerts its effects in rheumatoid arthritis?
- Inhibition of T cell apoptosis
- Inhibition of multiple intracellular enzymes (correct)
- Inhibition of DNA synthesis exclusively
- Inhibition of lysosomal stability
What is the primary characteristic of rheumatoid arthritis?
What is the primary characteristic of rheumatoid arthritis?
- Symmetric small joint inflammation (correct)
- Local muscle atrophy
- Rapid joint regeneration
- Asymmetric joint inflammation
Which of the following describes the mechanism of action of hydroxychloroquine?
Which of the following describes the mechanism of action of hydroxychloroquine?
- Decreased IgA and IgM production
- Stabilization of lysosomal membranes (correct)
- Activation of T cell response to antigens
- Inhibition of cytokine release from macrophages
Which immune cells are primarily involved in the pathophysiology of rheumatoid arthritis?
Which immune cells are primarily involved in the pathophysiology of rheumatoid arthritis?
Which drug requires administration of folic acid to prevent deficiency after its use?
Which drug requires administration of folic acid to prevent deficiency after its use?
What types of joints are mainly affected in rheumatoid arthritis?
What types of joints are mainly affected in rheumatoid arthritis?
What is the main adverse effect of methotrexate that requires patient monitoring?
What is the main adverse effect of methotrexate that requires patient monitoring?
How does cyclosporine specifically affect T cells?
How does cyclosporine specifically affect T cells?
Which of the following statements about symptoms of rheumatoid arthritis is true?
Which of the following statements about symptoms of rheumatoid arthritis is true?
What is a known but not fully understood aspect of the etiology of rheumatoid arthritis?
What is a known but not fully understood aspect of the etiology of rheumatoid arthritis?
What kind of joint deformities can occur in late cases of rheumatoid arthritis?
What kind of joint deformities can occur in late cases of rheumatoid arthritis?
Which soluble mediators are mentioned as causes of joint inflammation in rheumatoid arthritis?
Which soluble mediators are mentioned as causes of joint inflammation in rheumatoid arthritis?
What role does the immune system play in rheumatoid arthritis pathology?
What role does the immune system play in rheumatoid arthritis pathology?
What is the significance of detecting Cyclic Citrullinated Peptide antibodies in patients?
What is the significance of detecting Cyclic Citrullinated Peptide antibodies in patients?
Which of the following statements about Disease-Modifying Antirheumatoid Drugs (DMARDs) is true?
Which of the following statements about Disease-Modifying Antirheumatoid Drugs (DMARDs) is true?
Why are TNF-α inhibitors not recommended until after trying nonbiologic DMARDs?
Why are TNF-α inhibitors not recommended until after trying nonbiologic DMARDs?
Which of the following manifestations is least likely to be an extra-articular manifestation of rheumatoid arthritis?
Which of the following manifestations is least likely to be an extra-articular manifestation of rheumatoid arthritis?
What role do NSAIDs play in the management of rheumatoid arthritis?
What role do NSAIDs play in the management of rheumatoid arthritis?
Which of the following statements about the use of corticosteroids in RA management is incorrect?
Which of the following statements about the use of corticosteroids in RA management is incorrect?
Which TNF-α inhibitor is described as a recombinant protein?
Which TNF-α inhibitor is described as a recombinant protein?
What is a potential risk associated with the use of TNF-α inhibitors?
What is a potential risk associated with the use of TNF-α inhibitors?
Methotrexate must be taken daily to maintain its effectiveness.
Methotrexate must be taken daily to maintain its effectiveness.
The primary mechanism of action of sulfasalazine involves the inhibition of IgA and IgM production.
The primary mechanism of action of sulfasalazine involves the inhibition of IgA and IgM production.
Anakinra has a long half-life and can be given orally once a week.
Anakinra has a long half-life and can be given orally once a week.
Gold salts primarily inhibit the functions of human macrophages.
Gold salts primarily inhibit the functions of human macrophages.
Cyclophosphamide works by enhancing DNA synthesis in immune cells.
Cyclophosphamide works by enhancing DNA synthesis in immune cells.
Rheumatoid arthritis primarily affects large joints in a symmetrical manner.
Rheumatoid arthritis primarily affects large joints in a symmetrical manner.
The exact etiology of rheumatoid arthritis is well understood and solely attributed to genetic factors.
The exact etiology of rheumatoid arthritis is well understood and solely attributed to genetic factors.
Inflammation in rheumatoid arthritis is caused by activated T cells, B cells, and other immune cells.
Inflammation in rheumatoid arthritis is caused by activated T cells, B cells, and other immune cells.
Joint deformity in late cases of rheumatoid arthritis is characterized by the absence of symptoms.
Joint deformity in late cases of rheumatoid arthritis is characterized by the absence of symptoms.
Symptoms of rheumatoid arthritis are often more severe in the evening.
Symptoms of rheumatoid arthritis are often more severe in the evening.
Cytokines such as TNF-α and IL-1 are type of soluble mediators that contribute to joint inflammation in rheumatoid arthritis.
Cytokines such as TNF-α and IL-1 are type of soluble mediators that contribute to joint inflammation in rheumatoid arthritis.
Rheumatoid arthritis can lead to cartilage destruction and bone erosion due to an abnormal immune response.
Rheumatoid arthritis can lead to cartilage destruction and bone erosion due to an abnormal immune response.
Extra-articular manifestations of rheumatoid arthritis are rare and seldom observed.
Extra-articular manifestations of rheumatoid arthritis are rare and seldom observed.
Cyclic Citrullinated Peptide antibodies can be detected up to 5 years before the development of rheumatoid arthritis.
Cyclic Citrullinated Peptide antibodies can be detected up to 5 years before the development of rheumatoid arthritis.
Disease-Modifying Antirheumatoid Drugs (DMARDs) begin to show their effects within hours of administration.
Disease-Modifying Antirheumatoid Drugs (DMARDs) begin to show their effects within hours of administration.
Adalimumab and infliximab are examples of nonbiologic DMARDs.
Adalimumab and infliximab are examples of nonbiologic DMARDs.
Joint X-rays can show symptoms specific to rheumatoid arthritis such as joint swelling and bony erosions.
Joint X-rays can show symptoms specific to rheumatoid arthritis such as joint swelling and bony erosions.
Corticosteroids are intended for long-term therapy in the management of rheumatoid arthritis.
Corticosteroids are intended for long-term therapy in the management of rheumatoid arthritis.
Combinations of two DMARDs are generally less effective than using a single DMARD.
Combinations of two DMARDs are generally less effective than using a single DMARD.
NSAIDs are effective in preventing joint destruction due to rheumatoid arthritis.
NSAIDs are effective in preventing joint destruction due to rheumatoid arthritis.
Live virus vaccination is a contraindication for the use of TNF-α inhibitors.
Live virus vaccination is a contraindication for the use of TNF-α inhibitors.
What must be administered 24 hours after a dose of methotrexate to counteract possible deficiency?
What must be administered 24 hours after a dose of methotrexate to counteract possible deficiency?
How does leflunomide compare to methotrexate in terms of effectiveness for bone damage?
How does leflunomide compare to methotrexate in terms of effectiveness for bone damage?
What is the main mechanism by which gold salts function in the treatment of rheumatoid arthritis?
What is the main mechanism by which gold salts function in the treatment of rheumatoid arthritis?
Identify the key mechanism by which cyclosporine exerts its effects on T cells.
Identify the key mechanism by which cyclosporine exerts its effects on T cells.
Which drug is a competitive IL-1 receptor antagonist and requires daily subcutaneous administration?
Which drug is a competitive IL-1 receptor antagonist and requires daily subcutaneous administration?
What role do activated immune cells play in the pathophysiology of rheumatoid arthritis?
What role do activated immune cells play in the pathophysiology of rheumatoid arthritis?
Describe a common clinical manifestation of rheumatoid arthritis in small joints.
Describe a common clinical manifestation of rheumatoid arthritis in small joints.
What is a significant, yet unclear factor, contributing to the development of rheumatoid arthritis?
What is a significant, yet unclear factor, contributing to the development of rheumatoid arthritis?
What is the impact of cytokines like TNF-α and IL-1 in rheumatoid arthritis?
What is the impact of cytokines like TNF-α and IL-1 in rheumatoid arthritis?
In severe cases of rheumatoid arthritis, which additional joints may become affected?
In severe cases of rheumatoid arthritis, which additional joints may become affected?
What distinguishes the joint symptoms of rheumatoid arthritis from other types of arthritis?
What distinguishes the joint symptoms of rheumatoid arthritis from other types of arthritis?
Explain the significance of the term 'extra-articular manifestations' in rheumatoid arthritis.
Explain the significance of the term 'extra-articular manifestations' in rheumatoid arthritis.
What does the immune system's misidentification of joint structures as 'foreign' indicate in rheumatoid arthritis?
What does the immune system's misidentification of joint structures as 'foreign' indicate in rheumatoid arthritis?
What role do DMARDs play in the management of rheumatoid arthritis?
What role do DMARDs play in the management of rheumatoid arthritis?
What are the implications of detecting anti-CCP antibodies in a patient?
What are the implications of detecting anti-CCP antibodies in a patient?
Why are large doses of NSAIDs typically required in the management of rheumatoid arthritis?
Why are large doses of NSAIDs typically required in the management of rheumatoid arthritis?
What is a significant reason for the contraindications associated with TNF-α inhibitors?
What is a significant reason for the contraindications associated with TNF-α inhibitors?
How do biologic DMARDs, such as Adalimumab and Infliximab, function in treating rheumatoid arthritis?
How do biologic DMARDs, such as Adalimumab and Infliximab, function in treating rheumatoid arthritis?
What key advantage do combinations of DMARDs offer over single DMARD therapy?
What key advantage do combinations of DMARDs offer over single DMARD therapy?
What is the rationale behind using corticosteroids as a short-term therapy in rheumatoid arthritis management?
What is the rationale behind using corticosteroids as a short-term therapy in rheumatoid arthritis management?
Why should the administration of TNF inhibitors be delayed until after the use of a nonbiologic DMARD?
Why should the administration of TNF inhibitors be delayed until after the use of a nonbiologic DMARD?
Methotrexate is a folic acid antagonist with cytotoxic and immunosuppressant properties and is used in more than 60% of RA cases, inhibiting multiple intracellular ______.
Methotrexate is a folic acid antagonist with cytotoxic and immunosuppressant properties and is used in more than 60% of RA cases, inhibiting multiple intracellular ______.
Cyclophosphamide and azathioprine suppress immune function through their cytotoxic action by inhibiting ______ synthesis.
Cyclophosphamide and azathioprine suppress immune function through their cytotoxic action by inhibiting ______ synthesis.
Hydroxychloroquine decreases synthesis of ______ and RNA in inflammatory cells and also stabilizes lysosomal membranes.
Hydroxychloroquine decreases synthesis of ______ and RNA in inflammatory cells and also stabilizes lysosomal membranes.
Leflunomide suppresses pyrimidine synthesis and the functions of ______ cells.
Leflunomide suppresses pyrimidine synthesis and the functions of ______ cells.
Anakinra is a competitive ______ receptor antagonist and must be administered subcutaneously daily.
Anakinra is a competitive ______ receptor antagonist and must be administered subcutaneously daily.
Rheumatoid arthritis (RA) is characterized by symmetric small joint ______, swelling, and deformity.
Rheumatoid arthritis (RA) is characterized by symmetric small joint ______, swelling, and deformity.
The immune system mistakenly attacks joint structures as if they were ______ antigens.
The immune system mistakenly attacks joint structures as if they were ______ antigens.
In RA, the involvement of small joints most often includes the hands and ______.
In RA, the involvement of small joints most often includes the hands and ______.
The exact ______ of rheumatoid arthritis remains unclear, although genetic factors play an important role.
The exact ______ of rheumatoid arthritis remains unclear, although genetic factors play an important role.
Clinical manifestations of RA include swollen, painful joints with limited ______.
Clinical manifestations of RA include swollen, painful joints with limited ______.
In rheumatoid arthritis, affected joints tend to be especially worse in the ______.
In rheumatoid arthritis, affected joints tend to be especially worse in the ______.
The pathophysiology of rheumatoid arthritis involves activated immune cells including T cells and ______.
The pathophysiology of rheumatoid arthritis involves activated immune cells including T cells and ______.
Chronic inflammation in RA can lead to cartilage destruction, bone erosion, and ______.
Chronic inflammation in RA can lead to cartilage destruction, bone erosion, and ______.
Detection of Cyclic Citrullinated Peptide antibodies is more specific than ______ and can be detected up to 10 years before the development of RA.
Detection of Cyclic Citrullinated Peptide antibodies is more specific than ______ and can be detected up to 10 years before the development of RA.
They prevent progression of the disease and slow joint destruction by modifying the immune ______.
They prevent progression of the disease and slow joint destruction by modifying the immune ______.
Adalimumab and infliximab are monoclonal antibodies that complex with ______ and prevent its interaction with T cells.
Adalimumab and infliximab are monoclonal antibodies that complex with ______ and prevent its interaction with T cells.
NSAIDs offer symptomatic relief of pain and inflammation but don't prevent joint ______.
NSAIDs offer symptomatic relief of pain and inflammation but don't prevent joint ______.
Combinations of two or more DMARDs are generally more ______ than a single drug.
Combinations of two or more DMARDs are generally more ______ than a single drug.
Acute and chronic infections are contraindications to the use of ______ inhibitors.
Acute and chronic infections are contraindications to the use of ______ inhibitors.
Corticosteroids are given as short-term therapy till ______ give their effect.
Corticosteroids are given as short-term therapy till ______ give their effect.
Joint X-ray can show joint swelling and bony ______ typical of RA.
Joint X-ray can show joint swelling and bony ______ typical of RA.
Match the following types of joint manifestations in rheumatoid arthritis with their descriptions:
Match the following types of joint manifestations in rheumatoid arthritis with their descriptions:
Match the following soluble mediators with their roles in rheumatoid arthritis pathophysiology:
Match the following soluble mediators with their roles in rheumatoid arthritis pathophysiology:
Match the following components of the immune system with their involvement in rheumatoid arthritis:
Match the following components of the immune system with their involvement in rheumatoid arthritis:
Match the following characteristics of rheumatoid arthritis with their correct descriptions:
Match the following characteristics of rheumatoid arthritis with their correct descriptions:
Match the following phases of rheumatoid arthritis with their features:
Match the following phases of rheumatoid arthritis with their features:
Match the following risk factors with their relevance to rheumatoid arthritis:
Match the following risk factors with their relevance to rheumatoid arthritis:
Match the following terms related to immune response in rheumatoid arthritis with their definitions:
Match the following terms related to immune response in rheumatoid arthritis with their definitions:
Match the following symptoms of rheumatoid arthritis with their typical characteristics:
Match the following symptoms of rheumatoid arthritis with their typical characteristics:
Match the following management strategies with their descriptions for rheumatoid arthritis (RA):
Match the following management strategies with their descriptions for rheumatoid arthritis (RA):
Match the following conditions with their corresponding extra-articular manifestations in rheumatoid arthritis:
Match the following conditions with their corresponding extra-articular manifestations in rheumatoid arthritis:
Match the following serological tests with their relevance in diagnosing rheumatoid arthritis:
Match the following serological tests with their relevance in diagnosing rheumatoid arthritis:
Match the following biologic DMARDs with their mechanism of action:
Match the following biologic DMARDs with their mechanism of action:
Match the following contraindications with their relevance to TNF-α inhibitors:
Match the following contraindications with their relevance to TNF-α inhibitors:
Match the following characteristics with their corresponding types of DMARDs:
Match the following characteristics with their corresponding types of DMARDs:
Match the following statements with their implications for RA management:
Match the following statements with their implications for RA management:
Match the following symptoms with their characteristics related to rheumatoid arthritis:
Match the following symptoms with their characteristics related to rheumatoid arthritis:
Match the following drugs with their primary mechanism of action:
Match the following drugs with their primary mechanism of action:
Match the following drugs with their administration route:
Match the following drugs with their administration route:
Match the following medications with their common adverse effects:
Match the following medications with their common adverse effects:
Match the following drugs with their classification:
Match the following drugs with their classification:
Match the following drugs with their specific effects on immune functions:
Match the following drugs with their specific effects on immune functions:
Study Notes
Definition of Rheumatoid Arthritis (RA)
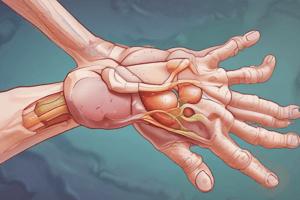
- Chronic inflammatory disease characterized by symmetrical small joint inflammation, swelling, and deformity.
- Extra-articular manifestations are common and can affect systemic organs.
Pathophysiology
- Exact etiology is unclear; genetic factors significantly influence RA development.
- Immune system involvement includes activated T cells, B cells, polymorphonuclear leukocytes, macrophages, and the complement system.
- Production of soluble mediators (lysozymes, cytokines such as TNF-α and IL-1) leads to joint inflammation, cartilage destruction, bone erosion, and deformity.
Clinical Manifestations
Articular Manifestations
- Primarily affects small joints of hands and toes symmetrically; larger joints can be affected in severe cases.
- Symptoms include swelling, pain, limited mobility, and worsened symptoms in the morning.
- Late-stage complications lead to characteristic joint deformities.
Extra-Articular Manifestations
- RA can manifest in systemic organs, potentially causing pleural effusion, pericarditis, vasculitis, and anemia.
Diagnosis
- Serological tests detect abnormal "rheumatoid factor" antibodies in 80% of RA patients.
- Cyclic Citrullinated Peptide (anti-CCP) antibodies are more specific and can be identified up to 10 years before RA onset.
- Joint X-rays reveal characteristic joint swelling and bony erosions.
Management of RA
Symptomatic Treatment
- NSAIDs provide relief for pain and inflammation but do not prevent joint destruction.
- Corticosteroids are used short-term until DMARDs take effect.
Disease-Modifying Antirheumatoid Drugs (DMARDs)
- DMARDs are crucial and should be initiated early; effects may take 3 weeks to 3 months.
- They prevent disease progression and joint damage by altering immune reactions.
- Combination therapy with multiple DMARDs is more effective than single-drug treatment.
Biologic DMARDs: TNF-α Inhibitors
- These are key DMARDs due to TNF-α's role in RA pathogenesis.
- Drugs include Adalimumab and Infliximab (monoclonal antibodies), and Etanercept (recombinant protein).
- Contraindications include acute/chronic infections, live virus vaccinations, demyelinating disorders, severe heart failure, and recent malignancies.
- Guidelines recommend using these after one nonbiologic DMARD, typically methotrexate, has failed.
Specific DMARDs
-
Methotrexate: First-line treatment in over 60% of RA cases; folic acid antagonist with cytotoxic properties. Weekly dosing with needed folic acid supplementation due to adverse effects including hepatotoxicity and myelosuppression.
-
Hydroxychloroquine: Antimalarial drug that reduces DNA/RNA synthesis in inflammatory cells and stabilizes lysosomal membranes.
-
Sulfasalazine: Metabolizes into sulfapyridine and 5-aminosalicylic acid, inhibiting IgA/IgM production and suppressing T and B cell functions.
-
Immunosuppressants: Cyclophosphamide and azathioprine inhibit immune function through cytotoxicity. Cyclosporine specifically targets T cell function.
-
Gold salts: Administered IM or orally; inhibit macrophage function and decrease inflammatory cytokines.
-
Leflunomide: Suppresses pyrimidine synthesis, inhibiting T and B cell functions; comparable to methotrexate in preventing bone damage.
-
Anakinra: Competitive IL-1 receptor antagonist, requiring daily subcutaneous administration due to a short half-life.
Definition of Rheumatoid Arthritis (RA)
- Chronic inflammatory disease characterized by symmetrical small joint inflammation, swelling, and deformity.
- Extra-articular manifestations are common and can affect systemic organs.
Pathophysiology
- Exact etiology is unclear; genetic factors significantly influence RA development.
- Immune system involvement includes activated T cells, B cells, polymorphonuclear leukocytes, macrophages, and the complement system.
- Production of soluble mediators (lysozymes, cytokines such as TNF-α and IL-1) leads to joint inflammation, cartilage destruction, bone erosion, and deformity.
Clinical Manifestations
Articular Manifestations
- Primarily affects small joints of hands and toes symmetrically; larger joints can be affected in severe cases.
- Symptoms include swelling, pain, limited mobility, and worsened symptoms in the morning.
- Late-stage complications lead to characteristic joint deformities.
Extra-Articular Manifestations
- RA can manifest in systemic organs, potentially causing pleural effusion, pericarditis, vasculitis, and anemia.
Diagnosis
- Serological tests detect abnormal "rheumatoid factor" antibodies in 80% of RA patients.
- Cyclic Citrullinated Peptide (anti-CCP) antibodies are more specific and can be identified up to 10 years before RA onset.
- Joint X-rays reveal characteristic joint swelling and bony erosions.
Management of RA
Symptomatic Treatment
- NSAIDs provide relief for pain and inflammation but do not prevent joint destruction.
- Corticosteroids are used short-term until DMARDs take effect.
Disease-Modifying Antirheumatoid Drugs (DMARDs)
- DMARDs are crucial and should be initiated early; effects may take 3 weeks to 3 months.
- They prevent disease progression and joint damage by altering immune reactions.
- Combination therapy with multiple DMARDs is more effective than single-drug treatment.
Biologic DMARDs: TNF-α Inhibitors
- These are key DMARDs due to TNF-α's role in RA pathogenesis.
- Drugs include Adalimumab and Infliximab (monoclonal antibodies), and Etanercept (recombinant protein).
- Contraindications include acute/chronic infections, live virus vaccinations, demyelinating disorders, severe heart failure, and recent malignancies.
- Guidelines recommend using these after one nonbiologic DMARD, typically methotrexate, has failed.
Specific DMARDs
-
Methotrexate: First-line treatment in over 60% of RA cases; folic acid antagonist with cytotoxic properties. Weekly dosing with needed folic acid supplementation due to adverse effects including hepatotoxicity and myelosuppression.
-
Hydroxychloroquine: Antimalarial drug that reduces DNA/RNA synthesis in inflammatory cells and stabilizes lysosomal membranes.
-
Sulfasalazine: Metabolizes into sulfapyridine and 5-aminosalicylic acid, inhibiting IgA/IgM production and suppressing T and B cell functions.
-
Immunosuppressants: Cyclophosphamide and azathioprine inhibit immune function through cytotoxicity. Cyclosporine specifically targets T cell function.
-
Gold salts: Administered IM or orally; inhibit macrophage function and decrease inflammatory cytokines.
-
Leflunomide: Suppresses pyrimidine synthesis, inhibiting T and B cell functions; comparable to methotrexate in preventing bone damage.
-
Anakinra: Competitive IL-1 receptor antagonist, requiring daily subcutaneous administration due to a short half-life.
Definition of Rheumatoid Arthritis (RA)
- Chronic inflammatory disease characterized by symmetrical small joint inflammation, swelling, and deformity.
- Extra-articular manifestations are common and can affect systemic organs.
Pathophysiology
- Exact etiology is unclear; genetic factors significantly influence RA development.
- Immune system involvement includes activated T cells, B cells, polymorphonuclear leukocytes, macrophages, and the complement system.
- Production of soluble mediators (lysozymes, cytokines such as TNF-α and IL-1) leads to joint inflammation, cartilage destruction, bone erosion, and deformity.
Clinical Manifestations
Articular Manifestations
- Primarily affects small joints of hands and toes symmetrically; larger joints can be affected in severe cases.
- Symptoms include swelling, pain, limited mobility, and worsened symptoms in the morning.
- Late-stage complications lead to characteristic joint deformities.
Extra-Articular Manifestations
- RA can manifest in systemic organs, potentially causing pleural effusion, pericarditis, vasculitis, and anemia.
Diagnosis
- Serological tests detect abnormal "rheumatoid factor" antibodies in 80% of RA patients.
- Cyclic Citrullinated Peptide (anti-CCP) antibodies are more specific and can be identified up to 10 years before RA onset.
- Joint X-rays reveal characteristic joint swelling and bony erosions.
Management of RA
Symptomatic Treatment
- NSAIDs provide relief for pain and inflammation but do not prevent joint destruction.
- Corticosteroids are used short-term until DMARDs take effect.
Disease-Modifying Antirheumatoid Drugs (DMARDs)
- DMARDs are crucial and should be initiated early; effects may take 3 weeks to 3 months.
- They prevent disease progression and joint damage by altering immune reactions.
- Combination therapy with multiple DMARDs is more effective than single-drug treatment.
Biologic DMARDs: TNF-α Inhibitors
- These are key DMARDs due to TNF-α's role in RA pathogenesis.
- Drugs include Adalimumab and Infliximab (monoclonal antibodies), and Etanercept (recombinant protein).
- Contraindications include acute/chronic infections, live virus vaccinations, demyelinating disorders, severe heart failure, and recent malignancies.
- Guidelines recommend using these after one nonbiologic DMARD, typically methotrexate, has failed.
Specific DMARDs
-
Methotrexate: First-line treatment in over 60% of RA cases; folic acid antagonist with cytotoxic properties. Weekly dosing with needed folic acid supplementation due to adverse effects including hepatotoxicity and myelosuppression.
-
Hydroxychloroquine: Antimalarial drug that reduces DNA/RNA synthesis in inflammatory cells and stabilizes lysosomal membranes.
-
Sulfasalazine: Metabolizes into sulfapyridine and 5-aminosalicylic acid, inhibiting IgA/IgM production and suppressing T and B cell functions.
-
Immunosuppressants: Cyclophosphamide and azathioprine inhibit immune function through cytotoxicity. Cyclosporine specifically targets T cell function.
-
Gold salts: Administered IM or orally; inhibit macrophage function and decrease inflammatory cytokines.
-
Leflunomide: Suppresses pyrimidine synthesis, inhibiting T and B cell functions; comparable to methotrexate in preventing bone damage.
-
Anakinra: Competitive IL-1 receptor antagonist, requiring daily subcutaneous administration due to a short half-life.
Definition of Rheumatoid Arthritis (RA)
- Chronic inflammatory disease characterized by symmetrical small joint inflammation, swelling, and deformity.
- Extra-articular manifestations are common and can affect systemic organs.
Pathophysiology
- Exact etiology is unclear; genetic factors significantly influence RA development.
- Immune system involvement includes activated T cells, B cells, polymorphonuclear leukocytes, macrophages, and the complement system.
- Production of soluble mediators (lysozymes, cytokines such as TNF-α and IL-1) leads to joint inflammation, cartilage destruction, bone erosion, and deformity.
Clinical Manifestations
Articular Manifestations
- Primarily affects small joints of hands and toes symmetrically; larger joints can be affected in severe cases.
- Symptoms include swelling, pain, limited mobility, and worsened symptoms in the morning.
- Late-stage complications lead to characteristic joint deformities.
Extra-Articular Manifestations
- RA can manifest in systemic organs, potentially causing pleural effusion, pericarditis, vasculitis, and anemia.
Diagnosis
- Serological tests detect abnormal "rheumatoid factor" antibodies in 80% of RA patients.
- Cyclic Citrullinated Peptide (anti-CCP) antibodies are more specific and can be identified up to 10 years before RA onset.
- Joint X-rays reveal characteristic joint swelling and bony erosions.
Management of RA
Symptomatic Treatment
- NSAIDs provide relief for pain and inflammation but do not prevent joint destruction.
- Corticosteroids are used short-term until DMARDs take effect.
Disease-Modifying Antirheumatoid Drugs (DMARDs)
- DMARDs are crucial and should be initiated early; effects may take 3 weeks to 3 months.
- They prevent disease progression and joint damage by altering immune reactions.
- Combination therapy with multiple DMARDs is more effective than single-drug treatment.
Biologic DMARDs: TNF-α Inhibitors
- These are key DMARDs due to TNF-α's role in RA pathogenesis.
- Drugs include Adalimumab and Infliximab (monoclonal antibodies), and Etanercept (recombinant protein).
- Contraindications include acute/chronic infections, live virus vaccinations, demyelinating disorders, severe heart failure, and recent malignancies.
- Guidelines recommend using these after one nonbiologic DMARD, typically methotrexate, has failed.
Specific DMARDs
-
Methotrexate: First-line treatment in over 60% of RA cases; folic acid antagonist with cytotoxic properties. Weekly dosing with needed folic acid supplementation due to adverse effects including hepatotoxicity and myelosuppression.
-
Hydroxychloroquine: Antimalarial drug that reduces DNA/RNA synthesis in inflammatory cells and stabilizes lysosomal membranes.
-
Sulfasalazine: Metabolizes into sulfapyridine and 5-aminosalicylic acid, inhibiting IgA/IgM production and suppressing T and B cell functions.
-
Immunosuppressants: Cyclophosphamide and azathioprine inhibit immune function through cytotoxicity. Cyclosporine specifically targets T cell function.
-
Gold salts: Administered IM or orally; inhibit macrophage function and decrease inflammatory cytokines.
-
Leflunomide: Suppresses pyrimidine synthesis, inhibiting T and B cell functions; comparable to methotrexate in preventing bone damage.
-
Anakinra: Competitive IL-1 receptor antagonist, requiring daily subcutaneous administration due to a short half-life.
Definition of Rheumatoid Arthritis (RA)
- Chronic inflammatory disease characterized by symmetrical small joint inflammation, swelling, and deformity.
- Extra-articular manifestations are common and can affect systemic organs.
Pathophysiology
- Exact etiology is unclear; genetic factors significantly influence RA development.
- Immune system involvement includes activated T cells, B cells, polymorphonuclear leukocytes, macrophages, and the complement system.
- Production of soluble mediators (lysozymes, cytokines such as TNF-α and IL-1) leads to joint inflammation, cartilage destruction, bone erosion, and deformity.
Clinical Manifestations
Articular Manifestations
- Primarily affects small joints of hands and toes symmetrically; larger joints can be affected in severe cases.
- Symptoms include swelling, pain, limited mobility, and worsened symptoms in the morning.
- Late-stage complications lead to characteristic joint deformities.
Extra-Articular Manifestations
- RA can manifest in systemic organs, potentially causing pleural effusion, pericarditis, vasculitis, and anemia.
Diagnosis
- Serological tests detect abnormal "rheumatoid factor" antibodies in 80% of RA patients.
- Cyclic Citrullinated Peptide (anti-CCP) antibodies are more specific and can be identified up to 10 years before RA onset.
- Joint X-rays reveal characteristic joint swelling and bony erosions.
Management of RA
Symptomatic Treatment
- NSAIDs provide relief for pain and inflammation but do not prevent joint destruction.
- Corticosteroids are used short-term until DMARDs take effect.
Disease-Modifying Antirheumatoid Drugs (DMARDs)
- DMARDs are crucial and should be initiated early; effects may take 3 weeks to 3 months.
- They prevent disease progression and joint damage by altering immune reactions.
- Combination therapy with multiple DMARDs is more effective than single-drug treatment.
Biologic DMARDs: TNF-α Inhibitors
- These are key DMARDs due to TNF-α's role in RA pathogenesis.
- Drugs include Adalimumab and Infliximab (monoclonal antibodies), and Etanercept (recombinant protein).
- Contraindications include acute/chronic infections, live virus vaccinations, demyelinating disorders, severe heart failure, and recent malignancies.
- Guidelines recommend using these after one nonbiologic DMARD, typically methotrexate, has failed.
Specific DMARDs
-
Methotrexate: First-line treatment in over 60% of RA cases; folic acid antagonist with cytotoxic properties. Weekly dosing with needed folic acid supplementation due to adverse effects including hepatotoxicity and myelosuppression.
-
Hydroxychloroquine: Antimalarial drug that reduces DNA/RNA synthesis in inflammatory cells and stabilizes lysosomal membranes.
-
Sulfasalazine: Metabolizes into sulfapyridine and 5-aminosalicylic acid, inhibiting IgA/IgM production and suppressing T and B cell functions.
-
Immunosuppressants: Cyclophosphamide and azathioprine inhibit immune function through cytotoxicity. Cyclosporine specifically targets T cell function.
-
Gold salts: Administered IM or orally; inhibit macrophage function and decrease inflammatory cytokines.
-
Leflunomide: Suppresses pyrimidine synthesis, inhibiting T and B cell functions; comparable to methotrexate in preventing bone damage.
-
Anakinra: Competitive IL-1 receptor antagonist, requiring daily subcutaneous administration due to a short half-life.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers part 4 of drug therapy related to rheumatoid arthritis (RA). It includes definitions and characteristics of RA, focusing on its chronic inflammatory nature, joint inflammation, swelling, and deformities. It also touches on extra-articular manifestations associated with the disease.