Podcast
Questions and Answers
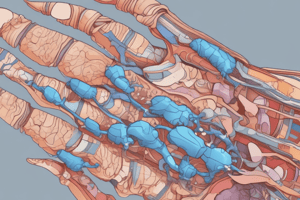
Which of the following is a characteristic of rheumatoid arthritis?
Which of the following is a characteristic of rheumatoid arthritis?
- It is a chronic autoimmune disease with systemic inflammation (correct)
- It is caused by impaired uric acid metabolism
- It is caused by excessive hyperuricemia due to increased core destruction during antineoplastic therapy
- It primarily manifests as hyperuricemia and acute arthritis seizures
What is the primary autoantibody found in 85% of patients with rheumatoid arthritis?
What is the primary autoantibody found in 85% of patients with rheumatoid arthritis?
- Antinuclear antibodies (ANA)
- Uric acid crystals
- Antineutrophil cytoplasmic antibodies (ANCA)
- Rheumatoid factor (RF), mostly IgM in the structure of IgG (correct)
Which drugs can reduce uric acid excretion and contribute to the development of gout?
Which drugs can reduce uric acid excretion and contribute to the development of gout?
- Antimalarial drugs
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Thiazide group diuretics (correct)
- Glucocorticoids
Which of the following drugs is indicated for the long-term treatment of hyperuricemia related to primary or secondary gout?
Which of the following drugs is indicated for the long-term treatment of hyperuricemia related to primary or secondary gout?
Which drug inhibits the phagocytosis of urate crystals, preventing recrystallization and leukocyte migration in acute gouty arthritis?
Which drug inhibits the phagocytosis of urate crystals, preventing recrystallization and leukocyte migration in acute gouty arthritis?
Which drug is an inhibitor of the xanthine oxidase enzyme, reducing the formation of uric acid?
Which drug is an inhibitor of the xanthine oxidase enzyme, reducing the formation of uric acid?
Which drug is used to lower urate levels better than allopurinol, but has no indication for gout?
Which drug is used to lower urate levels better than allopurinol, but has no indication for gout?
Which drug affects the proximal tubules in the kidneys, reducing the reabsorption of urates in the ultrafiltrate?
Which drug affects the proximal tubules in the kidneys, reducing the reabsorption of urates in the ultrafiltrate?
Which drug has an anti-inflammatory effect only in gouty arthritis, and is also beneficial in familial Mediterranean fever (FMF) and Behçet's syndrome?
Which drug has an anti-inflammatory effect only in gouty arthritis, and is also beneficial in familial Mediterranean fever (FMF) and Behçet's syndrome?
Which drug is obtained from the onion and seed of the Crocus (Colchicum autumnale) plant and has been used in the treatment of gout since ancient times?
Which drug is obtained from the onion and seed of the Crocus (Colchicum autumnale) plant and has been used in the treatment of gout since ancient times?
Which drug binds to TNF-α, causing its inactivation, and is used to treat rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, ankylosing spondylitis, Crohn's disease, psoriasis, and psoriatic arthritis?
Which drug binds to TNF-α, causing its inactivation, and is used to treat rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, ankylosing spondylitis, Crohn's disease, psoriasis, and psoriatic arthritis?
Which drug is observed to frequently cause M. Tuberculosis, hepatitis B virus, and invasive systemic fungal infections or the risk of their reactivation during treatment?
Which drug is observed to frequently cause M. Tuberculosis, hepatitis B virus, and invasive systemic fungal infections or the risk of their reactivation during treatment?
Which drug is used for the prophylaxis of gout attacks in people with gout or secondary hyperuricemia, and has no effect on uric acid metabolism or anti-inflammatory effect?
Which drug is used for the prophylaxis of gout attacks in people with gout or secondary hyperuricemia, and has no effect on uric acid metabolism or anti-inflammatory effect?
Which of the following drugs is NOT classified as a DMARD for rheumatoid arthritis treatment?
Which of the following drugs is NOT classified as a DMARD for rheumatoid arthritis treatment?
What is the main action of glucocorticoids in rheumatoid arthritis therapy?
What is the main action of glucocorticoids in rheumatoid arthritis therapy?
Which of the following is NOT a side effect of long-term glucocorticoid use?
Which of the following is NOT a side effect of long-term glucocorticoid use?
When can a response to DMARDs typically be first observed in rheumatoid arthritis treatment?
When can a response to DMARDs typically be first observed in rheumatoid arthritis treatment?
Which of the following DMARDs is considered the first choice in the treatment of rheumatoid arthritis?
Which of the following DMARDs is considered the first choice in the treatment of rheumatoid arthritis?
What mechanism do TNF-alpha blockers employ to alleviate rheumatoid arthritis symptoms?
What mechanism do TNF-alpha blockers employ to alleviate rheumatoid arthritis symptoms?
Which of the following is NOT a disease treated with methotrexate besides rheumatoid arthritis?
Which of the following is NOT a disease treated with methotrexate besides rheumatoid arthritis?
What is the typical weekly dose range of methotrexate when used for rheumatoid arthritis?
What is the typical weekly dose range of methotrexate when used for rheumatoid arthritis?
Which of the following best describes the role of monoclonal antibodies in rheumatoid arthritis therapy?
Which of the following best describes the role of monoclonal antibodies in rheumatoid arthritis therapy?
What is the primary function of methotrexate in the treatment of rheumatoid arthritis?
What is the primary function of methotrexate in the treatment of rheumatoid arthritis?
Which of the following is NOT a common side effect of methotrexate?
Which of the following is NOT a common side effect of methotrexate?
What is the main risk associated with the long-term use of glucocorticoids in rheumatoid arthritis treatment?
What is the main risk associated with the long-term use of glucocorticoids in rheumatoid arthritis treatment?
Which drug is considered a first-line treatment for rheumatoid arthritis and works by inhibiting dihydroorotate dehydrogenase, an enzyme involved in de novo pyrimidine synthesis?
Which drug is considered a first-line treatment for rheumatoid arthritis and works by inhibiting dihydroorotate dehydrogenase, an enzyme involved in de novo pyrimidine synthesis?
Which drug, used in the treatment of gout, works by inhibiting tubular reabsorption of urate and is often used in combination with other medications for gout management?
Which drug, used in the treatment of gout, works by inhibiting tubular reabsorption of urate and is often used in combination with other medications for gout management?
Which drug used in rheumatoid arthritis therapy can lead to hepatotoxicity independent of dose?
Which drug used in rheumatoid arthritis therapy can lead to hepatotoxicity independent of dose?
Which drug used in rheumatoid arthritis therapy requires ophthalmoscopic monitoring due to the risk of retinopathy?
Which drug used in rheumatoid arthritis therapy requires ophthalmoscopic monitoring due to the risk of retinopathy?
Which drug used in rheumatoid arthritis therapy is contraindicated in pregnancy?
Which drug used in rheumatoid arthritis therapy is contraindicated in pregnancy?
Which drug used in rheumatoid arthritis therapy is a sulfhydryl chelator primarily used against Wilson's disease and heavy metal poisoning?
Which drug used in rheumatoid arthritis therapy is a sulfhydryl chelator primarily used against Wilson's disease and heavy metal poisoning?
Which drug used in rheumatoid arthritis therapy binds to the IL-6 receptor and can cause tuberculosis, fungal, viral, and other opportunistic infections?
Which drug used in rheumatoid arthritis therapy binds to the IL-6 receptor and can cause tuberculosis, fungal, viral, and other opportunistic infections?
Which drug used in rheumatoid arthritis therapy inhibits CD28 binding and T-cell activation on T cells?
Which drug used in rheumatoid arthritis therapy inhibits CD28 binding and T-cell activation on T cells?
Which drug used in rheumatoid arthritis therapy is a 4-aminoquinoline-derived antimalarial drug?
Which drug used in rheumatoid arthritis therapy is a 4-aminoquinoline-derived antimalarial drug?
Which drug used in rheumatoid arthritis therapy is an interleukin-1 receptor antagonist?
Which drug used in rheumatoid arthritis therapy is an interleukin-1 receptor antagonist?
Which drug used in rheumatoid arthritis therapy is metabolized by bacteria in the intestinal flora to sulfapyridine and 5-aminosalicylic acid?
Which drug used in rheumatoid arthritis therapy is metabolized by bacteria in the intestinal flora to sulfapyridine and 5-aminosalicylic acid?
Which drug used in rheumatoid arthritis therapy is a human-mouse chimeric monoclonal IgG1 that binds to the CD-20 molecule on the surface of B lymphocytes?
Which drug used in rheumatoid arthritis therapy is a human-mouse chimeric monoclonal IgG1 that binds to the CD-20 molecule on the surface of B lymphocytes?
Which drug used in rheumatoid arthritis therapy is at least as effective as methotrexate and sulfasalazine in improving disability and the progression of radiological symptoms of RA?
Which drug used in rheumatoid arthritis therapy is at least as effective as methotrexate and sulfasalazine in improving disability and the progression of radiological symptoms of RA?
Which drug used in rheumatoid arthritis therapy can cause dermatitis, mucous membrane inflammation and anaphylactoid reaction?
Which drug used in rheumatoid arthritis therapy can cause dermatitis, mucous membrane inflammation and anaphylactoid reaction?
Which drug used in rheumatoid arthritis therapy requires ophthalmoscopic monitoring due to the risk of retinopathy?
Which drug used in rheumatoid arthritis therapy requires ophthalmoscopic monitoring due to the risk of retinopathy?
Which drug used in rheumatoid arthritis therapy is a human-mouse chimeric monoclonal IgG1 that binds to the CD-20 molecule on the surface of B lymphocytes?
Which drug used in rheumatoid arthritis therapy is a human-mouse chimeric monoclonal IgG1 that binds to the CD-20 molecule on the surface of B lymphocytes?
Which drug used in rheumatoid arthritis therapy is metabolized in the intestinal flora and can cause nausea, vomiting, headache, and skin rash?
Which drug used in rheumatoid arthritis therapy is metabolized in the intestinal flora and can cause nausea, vomiting, headache, and skin rash?
Which drug used in rheumatoid arthritis therapy inhibits T-cell activation and is used in the treatment of moderate to severe rheumatoid arthritis and juvenile arthritis that does not respond to TNF antagonist and other DMARDs?
Which drug used in rheumatoid arthritis therapy inhibits T-cell activation and is used in the treatment of moderate to severe rheumatoid arthritis and juvenile arthritis that does not respond to TNF antagonist and other DMARDs?
Which drug used in rheumatoid arthritis therapy is at least as effective as methotrexate and is used in active rheumatoid arthritis and psoriatic arthritis?
Which drug used in rheumatoid arthritis therapy is at least as effective as methotrexate and is used in active rheumatoid arthritis and psoriatic arthritis?
Which drug used in rheumatoid arthritis therapy is a recombinant humanized IgG1 that is used to treat moderate-to-severe active rheumatoid arthritis in patients who do not respond to TNF-alpha antagonist treatment?
Which drug used in rheumatoid arthritis therapy is a recombinant humanized IgG1 that is used to treat moderate-to-severe active rheumatoid arthritis in patients who do not respond to TNF-alpha antagonist treatment?
Which drug used in rheumatoid arthritis therapy is an interleukin-1 receptor antagonist used in rheumatoid arthritis, Still's disease, and gout?
Which drug used in rheumatoid arthritis therapy is an interleukin-1 receptor antagonist used in rheumatoid arthritis, Still's disease, and gout?
Flashcards are hidden until you start studying
Study Notes
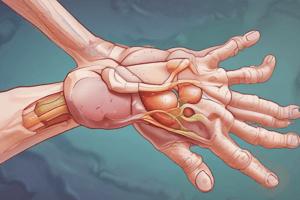
Rheumatoid Arthritis Drug Treatment Overview
- Symptom-modifying drugs and disease-modifying antirheumatic drugs (DMARDs) are used in the treatment of rheumatoid arthritis.
- Glucocorticoids are used in severe cases of rheumatoid arthritis to prevent T lymphocytes from secreting cytokines and inhibit the formation of antibodies by B lymphocytes.
- Glucocorticoids have immediate effects, slow down the formation of new bone erosions, and improve extra-articular symptoms, but long-term use carries risks that outweigh benefits.
- Side effects of glucocorticoids include Cushing-like symptoms, adrenal cortex atrophy, intolerance to infection and stress, GI ulcers and bleeding, glucose intolerance, and muscle weakness.
- DMARDs do not immediately affect symptoms and physical signs of the disease and often have a late therapeutic efficacy, with response beginning 3-4 months after starting treatment.
- Methotrexate and sulfasalazine are the best-tolerated DMARDs, and other options include chloroquine, hydroxychloroquine, gold compounds, penicillamine, azathioprine, cyclophosphamide, cyclosporine, leflunomide, cytokine modulators, and monoclonal antibodies.
- Methotrexate suppresses inflammation by inhibiting the formation of neutrophils, macrophages, dendritic cells, and lymphocytes.
- Monoclonal antibodies are produced by plasma cells formed by the proliferation of uniform cells stimulated against a single antigenic determinant.
- TNF-alpha blockers, such as adalimumab, etanercept, golimumab, infliximab, and certolizumab pegol, bind to TNF-α and cause its inactivation.
- Methotrexate is the first choice DMARD in the treatment of rheumatoid arthritis, used in 50-70% of patients at lower doses (15-25mg per week) than those required for cancer chemotherapy.
- Methotrexate is used to treat rheumatoid arthritis, juvenile chronic arthritis, psoriasis, psoriatic arthritis, ankylosing spondylitis, polymyositis, dermatomyositis, Wegener's granulomatosis, giant cell arteritis, and systemic lupus erythematosus (SLE).
- Common side effects of methotrexate include nausea and mucous membrane irritation.
Rheumatoid Arthritis Drugs: Key Points
- Chloroquine phosphate and hydroxychloroquine sulfate are 4-aminoquinoline-derived antimalarial drugs used as backup treatment for rheumatoid arthritis and lupus erythematosus.
- Gold compounds, including oro and sodium orothiomalate, are used in patients who do not respond to classical anti-inflammatory drugs, and their side effects include dermatitis and mucous membrane inflammation.
- Penicillamine, a sulfhydryl chelator, is effective against some types of rheumatoid arthritis, with common side effects being itching, skin rashes, and taste disturbances.
- Anakinra, an interleukin-1 receptor antagonist, is used in rheumatoid arthritis, Still's disease, gout, and other conditions when other treatments are ineffective, with therapeutic effects seen in 4-6 weeks for rheumatoid arthritis.
- Leflunomide, at least as effective as methotrexate, is used in active rheumatoid arthritis and psoriatic arthritis, with therapeutic effects appearing after 4-6 weeks.
- Prior to leflunomide treatment, complete blood counts and liver enzyme tests should be performed, and effective contraception is necessary during treatment and for two years after discontinuation.
- Sulfasalazine is metabolized in the intestinal flora and used in juvenile chronic arthritis, ankylosing spondylitis, and associated uveitis, with common side effects being nausea, vomiting, headache, and skin rash.
- Rituximab, a human-mouse chimeric monoclonal IgG1, is used in the treatment of chronic lymphocytic leukemia and B-cell non-Hodgkin lymphoma, in combination with methotrexate in patients not responding to other drugs.
- Abatacept inhibits T-cell activation and is used in the treatment of moderate to severe rheumatoid arthritis and juvenile arthritis that does not respond to TNF antagonist and other DMARDs.
- Tocilizumab, a recombinant humanized IgG1, is used to treat moderate-to-severe active rheumatoid arthritis in patients who do not respond to TNF-alpha antagonist treatment, and can cause opportunistic infections and a decrease in neutrophil and platelet count.
- Rheumatoid arthritis drugs can cause leukopenia, anemia, stomatitis, GI ulcer, alopecia, and hepatotoxicity, and folic acid and leukoverin reduce side effects but also effectiveness.
- Ocular disorders and neuropsychiatric disorders are dose-dependent side effects of chloroquine phosphate and hydroxychloroquine sulfate, with ophthalmoscopic monitoring necessary.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.