Podcast
Questions and Answers
What is the primary function of Type I pneumocytes in the alveoli?
What is the primary function of Type I pneumocytes in the alveoli?
- Produce surfactant to reduce surface tension
- Support the structural integrity of the alveolar wall
- Facilitate gas exchange by forming a blood-air barrier (correct)
- Act as macrophages to remove pathogens
Which of the following structures are included in the acinus of the lung?
Which of the following structures are included in the acinus of the lung?
- Pleura, lobule, fissures
- Bronchus, bronchiole, alveoli
- Alveolar sac, interstitial fibroblasts, types I and II cells
- Terminal bronchiole, respiratory bronchiole, alveolar duct (correct)
What is the function of Type II pneumocytes in the alveoli?
What is the function of Type II pneumocytes in the alveoli?
- They facilitate blood flow in the alveolar capillaries
- They serve as immune cells
- They form a barrier for gas exchange
- They produce surfactant (correct)
How is the gas exchange barrier structured in the alveolus?
How is the gas exchange barrier structured in the alveolus?
What is the role of fibroblasts in the interstitial space of the alveoli?
What is the role of fibroblasts in the interstitial space of the alveoli?
What describes empysema in relation to lung anatomy?
What describes empysema in relation to lung anatomy?
What is the primary function of alveolar ducts?
What is the primary function of alveolar ducts?
What anatomical feature helps maintain the structure of alveoli during ventilation?
What anatomical feature helps maintain the structure of alveoli during ventilation?
What is the primary function of surfactant in the alveoli?
What is the primary function of surfactant in the alveoli?
Which cells are responsible for producing surfactant in the alveoli?
Which cells are responsible for producing surfactant in the alveoli?
What is the consequence of having low or no surfactant in the alveoli as described by LaPlace's law?
What is the consequence of having low or no surfactant in the alveoli as described by LaPlace's law?
What is the role of pulmonary alveolar macrophages?
What is the role of pulmonary alveolar macrophages?
Which type of blood vessels provides a low-pressure blood supply to the alveoli?
Which type of blood vessels provides a low-pressure blood supply to the alveoli?
Which layer of pleura covers the lungs?
Which layer of pleura covers the lungs?
What composes the pleural cavity?
What composes the pleural cavity?
What does interstitial fibrosis in conditions like ARDS indicate?
What does interstitial fibrosis in conditions like ARDS indicate?
Which structure functions to line the thoracic cavity?
Which structure functions to line the thoracic cavity?
What is the function of bronchiolar lymphatics?
What is the function of bronchiolar lymphatics?
What is the primary function of Clara cells found in terminal bronchioles?
What is the primary function of Clara cells found in terminal bronchioles?
What structural change occurs as the bronchi undergo branching?
What structural change occurs as the bronchi undergo branching?
Which component is NOT present in bronchioles?
Which component is NOT present in bronchioles?
As bronchioles narrow, what type of epithelium is primarily found?
As bronchioles narrow, what type of epithelium is primarily found?
What anatomical unit is defined as the structure distal to the last terminal bronchiole?
What anatomical unit is defined as the structure distal to the last terminal bronchiole?
What is a major consequence of bronchiectasis?
What is a major consequence of bronchiectasis?
Which of the following statements about the wall of the bronchus is true?
Which of the following statements about the wall of the bronchus is true?
Which type of tissue increases as bronchi undergo multiple branchings?
Which type of tissue increases as bronchi undergo multiple branchings?
Which of the following statements is false regarding respiratory bronchioles?
Which of the following statements is false regarding respiratory bronchioles?
What happens to goblet cells as one moves down the respiratory tract?
What happens to goblet cells as one moves down the respiratory tract?
Study Notes
Respiratory Epithelium
- Bronchi divide into bronchioles, then membranous bronchioles, and finally terminal bronchioles
- Conducting to respiring epithelium
- The respiratory system can be split into two sections: conducting and respiring
- Conducting portion serves to get air to the respiring portion
- Conducting system includes: trachea, bronchi, and bronchioles
- Trachea has cartilage rings that are C-shaped
- Bronchi start with cartilage rings which transition to smooth muscle
- Bronchioles contain no cartilage and have smooth muscle, lining with respiratory epithelium
Respiratory Bronchioles
- Respiratory bronchioles are the transition zone between the conducting airways and the gas-exchanging alveoli
- Branching occurs to form alveolar ducts and sacs
- Cilia in the respiratory bronchioles disappear distally
- Respiratory bronchioles have alveoli along their walls. Alveoli increase in number as the respiratory bronchioles get more distal.
Alveolar Ducts and Sacs
- Back-to-back alveolar openings along the walls of alveolar ducts
- Smooth muscle between alveolar openings looks like knobs.
- Alveolar ducts open into alveolar sacs
Acinus
- The acinus is the functional unit of the lung.
- Consists of the terminal bronchiole, respiratory bronchiole, alveolar duct, and alveolar sacs
Alveoli
- Tiny air sacs at the end of the respiratory bronchioles
- Walls are thin to allow for gas exchange between air and blood
- Separated by interalveolar septae, which contain capillaries.
- Lined by Type I cells (thin, flat squamous cells), Type II cells (produce surfactant), and alveolar macrophages
- Type I cells cover 95% of alveolar surface, Type II cells cover 5% of alveolar surface
Surfactant
- Surfactant is made by Type II pneumocytes and decreases surface tension in alveoli. This prevents alveoli from collapsing during expiration.
- Decreases surface tension in alveoli, requiring less pressure to keep them open
- If there is no or low surfactant, alveoli collapse.
- Composed of phospholipids and proteins
Pulmonary Alveolar Macrophages
- Found on the surface of alveoli and within the lumen of alveoli
- Derived from blood monocytes
- Remove debris and particles that escape mucus and cilia in the conducting portion of the respiratory tract
- Also called "dust cells"
Interstitium
- Connective tissue between the alveoli
- Consists of the basement membrane of the endothelial and epithelial cells, collagen and elastic fibers, fibroblasts and a few mononuclear cells
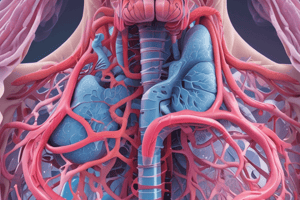
Respiratory Blood Supply
- The lung receives a dual arterial supply
- Pulmonary arteries are low pressure and branch alongside the bronchi and bronchioles
- Pulmonary arteries divide into capillary networks in the alveolar wall
- Bronchial arteries are high pressure and originate from the aorta
- Bronchial arteries branch alongside the bronchi to the respiratory bronchioles
Parietal and Visceral Pleura
- The outer surface of the lung and the inner surface of the thoracic cavity are covered by the pleura
- Parietal pleura lines the thoracic cavity
- Visceral pleura covers the lungs
- Serous membranes consist of simple squamous epithelial cells called mesothelium plus a thin layer of connective tissue
- The pleural cavity contains serous fluid made by the pleura
Clinical Correlations
- Injury to Type I pneumocytes can lead to pulmonary edema
- Smoking can lead to "smokers’ macrophages"
- Fibrosis in ARDS can cause thickened hyaline membranes and interstitial fibrosis
- Bronchiectasis is a condition where the airways are dilated, mucus secretion and inflammation are increased.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on the structure and function of the respiratory epithelium, including bronchi, bronchioles, and alveolar ducts. This quiz covers how air travels through the conducting and respiring portions of the respiratory system. Explore the key features from trachea to alveoli, and understand their transitions.