Podcast
Questions and Answers
Which of the following BEST describes respiratory physiology?
Which of the following BEST describes respiratory physiology?
- The study of gas exchange and transport within the body. (correct)
- The process of speech formation via vocal cord vibration.
- The study of the structural components of the lungs.
- The mechanics of microbial infection within the respiratory tract.
What is the primary role of alveoli in the respiratory system?
What is the primary role of alveoli in the respiratory system?
- Regulating blood pH through ion exchange.
- Producing surfactant to reduce surface tension.
- Filtering incoming air to remove pathogens.
- Facilitating gas exchange between air and blood. (correct)
Which of the following characteristics is UNIQUE to the trachea and primary bronchi?
Which of the following characteristics is UNIQUE to the trachea and primary bronchi?
- Structure provided by smooth muscle only.
- Semi-cartilaginous C-shaped rings. (correct)
- A complete ring of cartilage.
- Presence of smooth muscle.
How does the conducting zone of the respiratory system contribute to respiration?
How does the conducting zone of the respiratory system contribute to respiration?
How does the structure of bronchioles differ from that of the primary bronchi, and what is the functional significance of this difference?
How does the structure of bronchioles differ from that of the primary bronchi, and what is the functional significance of this difference?
What structural adaptation of alveoli facilitates efficient gas exchange?
What structural adaptation of alveoli facilitates efficient gas exchange?
How do Type II alveolar cells contribute to maintaining the integrity of the alveoli?
How do Type II alveolar cells contribute to maintaining the integrity of the alveoli?
Which of the following BEST describes the function of the respiratory membrane?
Which of the following BEST describes the function of the respiratory membrane?
What effect does contraction of the diaphragm have on thoracic volume and intrapulmonary pressure?
What effect does contraction of the diaphragm have on thoracic volume and intrapulmonary pressure?
Which muscles are primarily responsible for quiet inspiration at rest?
Which muscles are primarily responsible for quiet inspiration at rest?
How does forced expiration differ from quiet expiration?
How does forced expiration differ from quiet expiration?
What is the main function of the upper airway muscles?
What is the main function of the upper airway muscles?
How does the mucociliary escalator function to protect the respiratory system?
How does the mucociliary escalator function to protect the respiratory system?
How does smoking affect the mucociliary escalator and what is the consequence?
How does smoking affect the mucociliary escalator and what is the consequence?
How do macrophages in the alveoli protect the respiratory system?
How do macrophages in the alveoli protect the respiratory system?
What is the result of inhaling silica dust and asbestos on alveolar macrophages in the lungs, increasing the risk of pulmonary fibrosis?
What is the result of inhaling silica dust and asbestos on alveolar macrophages in the lungs, increasing the risk of pulmonary fibrosis?
What is the utility of spirometry in assessing lung function?
What is the utility of spirometry in assessing lung function?
Which of the following is TRUE regarding residual volume (RV)?
Which of the following is TRUE regarding residual volume (RV)?
How is Functional Residual Capacity (FRC) defined, and which volumes are summed to calculate it?
How is Functional Residual Capacity (FRC) defined, and which volumes are summed to calculate it?
What adjustments must be made when calculating alveolar ventilation compared to minute ventilation, and why are these adjustments essential?
What adjustments must be made when calculating alveolar ventilation compared to minute ventilation, and why are these adjustments essential?
How does alveolar ventilation respond to increased depth of breathing versus increased rate of breathing, and why?
How does alveolar ventilation respond to increased depth of breathing versus increased rate of breathing, and why?
In spirometry, what does the FEV1/FVC ratio represent, and how is it typically altered in obstructive lung diseases?
In spirometry, what does the FEV1/FVC ratio represent, and how is it typically altered in obstructive lung diseases?
What spirometric findings are typical in patients with restrictive lung disease, and why do these changes occur?
What spirometric findings are typical in patients with restrictive lung disease, and why do these changes occur?
How does the Helium Dilution Method measure lung volumes?
How does the Helium Dilution Method measure lung volumes?
Which statement accurately describes the conditions required for airflow during ventilation?
Which statement accurately describes the conditions required for airflow during ventilation?
How does an increase in the volume of the lungs affect alveolar pressure, according to Boyle's Law, and what is the consequence for airflow?
How does an increase in the volume of the lungs affect alveolar pressure, according to Boyle's Law, and what is the consequence for airflow?
What is the relationship between intrapleural pressure (PIP) and alveolar pressure (PALV) in maintaining lung inflation?
What is the relationship between intrapleural pressure (PIP) and alveolar pressure (PALV) in maintaining lung inflation?
What does transpulmonary pressure (PTP) represent, and how is it calculated?
What does transpulmonary pressure (PTP) represent, and how is it calculated?
Why is intrapleural pressure (PIP) normally negative, and what happens if it equals alveolar pressure?
Why is intrapleural pressure (PIP) normally negative, and what happens if it equals alveolar pressure?
In the context of airway resistance, where is resistance highest, and what airflow pattern contributes most to this resistance in the respiratory tract?
In the context of airway resistance, where is resistance highest, and what airflow pattern contributes most to this resistance in the respiratory tract?
How does an increase in smooth muscle contraction typically alter airway resistance, and under what conditions might this occur?
How does an increase in smooth muscle contraction typically alter airway resistance, and under what conditions might this occur?
How is lung compliance defined, and what do high and low lung compliance indicate about lung function?
How is lung compliance defined, and what do high and low lung compliance indicate about lung function?
How do pulmonary fibrosis and emphysema affect lung compliance?
How do pulmonary fibrosis and emphysema affect lung compliance?
How does dipalmitoyl phosphatidylcholine (DPPC) in surfactant reduce surface tension in alveoli?
How does dipalmitoyl phosphatidylcholine (DPPC) in surfactant reduce surface tension in alveoli?
How does surfactant help prevent alveolar collapse, especially in smaller alveoli?
How does surfactant help prevent alveolar collapse, especially in smaller alveoli?
How does posture or gravity affect regional differences in ventilation within the lungs, and what explains these differences?
How does posture or gravity affect regional differences in ventilation within the lungs, and what explains these differences?
According to Dalton's Law, what determines the total pressure of a gas mixture, and how does this relate to partial pressures?
According to Dalton's Law, what determines the total pressure of a gas mixture, and how does this relate to partial pressures?
What does Fick's Law of Diffusion state regarding the transfer of a gas across a tissue sheet, and what factors influence this rate?
What does Fick's Law of Diffusion state regarding the transfer of a gas across a tissue sheet, and what factors influence this rate?
How does inspired air humidity influence the partial pressure of ऑक्सीजन in the alveoli?
How does inspired air humidity influence the partial pressure of ऑक्सीजन in the alveoli?
What factors affect the partial pressure of the gases in the alveoli?
What factors affect the partial pressure of the gases in the alveoli?
What happens to the PO2 and PCO2 in the alveolar air when perfusion is increased?
What happens to the PO2 and PCO2 in the alveolar air when perfusion is increased?
How does the body respond in alveoli so that air is directed to well ventilated alveoli?
How does the body respond in alveoli so that air is directed to well ventilated alveoli?
Oxygen transport and binding of what protein relies on the partial pressure of oxygen?
Oxygen transport and binding of what protein relies on the partial pressure of oxygen?
Which of the following happens with a lower percentage of carbon dioxide being bound and transported back to the lungs.
Which of the following happens with a lower percentage of carbon dioxide being bound and transported back to the lungs.
Which factors affect the binding affinity between oxygen and hemoglobin?
Which factors affect the binding affinity between oxygen and hemoglobin?
How does increased body temperatures shift O2 saturation levels and what results occurs?
How does increased body temperatures shift O2 saturation levels and what results occurs?
Which of the following components are part of chemical control and impact ventilation.
Which of the following components are part of chemical control and impact ventilation.
Flashcards
Respiratory Physiology
Respiratory Physiology
Bringing oxygen into the lungs and eliminating carbon dioxide from the tissue and from the system.
Respiratory System Organization
Respiratory System Organization
Components of the respiratory system that are found outside the lungs.
Alveoli
Alveoli
Fundamental unit of the respiratory system.
Upper Airways
Upper Airways
Signup and view all the flashcards
Conducting Zone
Conducting Zone
Signup and view all the flashcards
Conducting Zone Function
Conducting Zone Function
Signup and view all the flashcards
Respiratory Zone
Respiratory Zone
Signup and view all the flashcards
Alveoli
Alveoli
Signup and view all the flashcards
Type I Alveolar Cells
Type I Alveolar Cells
Signup and view all the flashcards
Surfactant
Surfactant
Signup and view all the flashcards
Type II Alveolar Cells
Type II Alveolar Cells
Signup and view all the flashcards
Ventilation
Ventilation
Signup and view all the flashcards
Gas Exchange
Gas Exchange
Signup and view all the flashcards
Respiratory Muscles
Respiratory Muscles
Signup and view all the flashcards
Inspiratory pump Muscles
Inspiratory pump Muscles
Signup and view all the flashcards
Expiratory pump Muscles
Expiratory pump Muscles
Signup and view all the flashcards
Tidal Volume
Tidal Volume
Signup and view all the flashcards
Expiratory Reserve Volume
Expiratory Reserve Volume
Signup and view all the flashcards
Inspiratory Reserve Volume
Inspiratory Reserve Volume
Signup and view all the flashcards
Residual Volume
Residual Volume
Signup and view all the flashcards
Total or Minute Ventilation
Total or Minute Ventilation
Signup and view all the flashcards
Tidal Volume Definition
Tidal Volume Definition
Signup and view all the flashcards
Total or Minute Ventilation Definition
Total or Minute Ventilation Definition
Signup and view all the flashcards
Alveolar Ventilation
Alveolar Ventilation
Signup and view all the flashcards
Spirometry
Spirometry
Signup and view all the flashcards
Forced Expiratory Volume (FEV1)
Forced Expiratory Volume (FEV1)
Signup and view all the flashcards
Forced Vital Capacity (FVC)
Forced Vital Capacity (FVC)
Signup and view all the flashcards
Obstructive Lung Disease
Obstructive Lung Disease
Signup and view all the flashcards
Restrictive Lung Disease
Restrictive Lung Disease
Signup and view all the flashcards
Boyle's Law
Boyle's Law
Signup and view all the flashcards
Pressure Gradients
Pressure Gradients
Signup and view all the flashcards
Intrapleural Pressure (PIP)
Intrapleural Pressure (PIP)
Signup and view all the flashcards
Alveolar Pressure (PALV)
Alveolar Pressure (PALV)
Signup and view all the flashcards
Forces that affect resistance to Air Flow
Forces that affect resistance to Air Flow
Signup and view all the flashcards
Laminar Airflow
Laminar Airflow
Signup and view all the flashcards
Translational Airflow
Translational Airflow
Signup and view all the flashcards
Turbulent Airflow
Turbulent Airflow
Signup and view all the flashcards
Lung Compliance
Lung Compliance
Signup and view all the flashcards
Static Properties of the Lung
Static Properties of the Lung
Signup and view all the flashcards
Dynamic Properties of the Lung
Dynamic Properties of the Lung
Signup and view all the flashcards
Study Notes
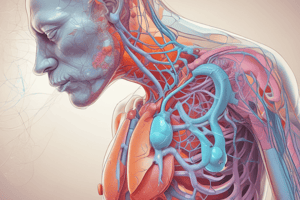
Respiratory Physiology
- Respiratory physiology studies how oxygen is brought into the lungs
- Notes how oxygen is delivered to the tissue
- Respiratory physiology studies how carbon dioxide is eliminated from the tissue and the system.
Functions of the Respiratory System
- Provides oxygen (O2) and eliminates carbon dioxide (CO2)
- This is involved in Homeostatic regulation of blood gases
- The respiratory system protects against microbial infection through a filtering action
- It regulates blood pH in coordination with the kidneys
- The respiratory system contributes to phonation
- It contributes to olfaction (sense of smell)
- It is also a reservoir for blood
Organization of the Respiratory System
- The respiratory system contains components that are found outside the lungs
- Lungs have a branched airway system
- The fundamental unit of the respiratory system is the alveoli
- Alveoli are embedded in a dense network and tissue characterized by the presence of smooth muscle tissue, smooth muscle cells and connective tissue
- The alveoli have a large number of capillaries
Upper Airways
- Air enters through the nasal cavity and oral cavity in the upper airway
- Pharynx: composed of the nasopharynx and the laryngopharynx
- Larynx: contains the vocal cords
- Trachea is part of the upper airways
Trachea & Lungs
- Order of air passage: larynx → trachea → two primary bronchi → lungs
- Trachea and primary bronchi are semi-cartilaginous
- The structure has a C-shaped ring (made of cartilage) in front and smooth muscle in the back
- This provides protection for the airway and gives elasticity
- Bronchi still have some cartilaginous structures but the air pathways are no longer C-shaped
- C-shaped rings of cartilage are replaced by plates of cartilage and smooth muscle in the Bronchi
- Bronchioles structure is provided by smooth muscle
Respiratory and Conducting Zones
- At each branch there is a reduction in the bronchiole size at each branch
- The tracheobronchial tree is classified and organized into two areas: conducting zone and respiratory zone
- The conducting zone contains the trachea, primary bronchi, bronchioles and terminal bronchioles
- It is called the conducting zone because in these areas there are no alveoli, and as a result no gas exchange occurs at the level of the conducting zone
- The conducting zone is an anatomical dead space, because it is not available for gas exchange
- The respiratory zone is further down in the branching of the airways and contains the alveoli
- Alveoli: initially sparse and not very numerous but become more and more numerous with the ramification or the branching
- Contains the respiratory bronchioles, alveolar ducts and alveolar sacs
- Gas is exchanged in the respiratory zone
- Air that enters the respiratory zone is available for gas exchange
- Terminal bronchioles are the smallest airways without alveoli
- Respiratory bronchioles have occasional alveoli
Respiratory and Conducting Zones Recap
- Respiratory bronchioles → sparse occasional alveoli
- Alveoli sacs → contain a large number of alveoli
Tracheobronchial tree
- Each branching is called a generation
- Begins at generation 0 at the trachea and arrives at generation 23 at the level of the alveolar sacs
- Both the diameter and the length of the airways at each generation decrease
- The diameter and length decrease from the level of the trachea to the alveolar sacs
- The number of branches at each specific generation level tends to increase
- Airways are smaller but more numerous towards the alveolar sacs
- The total cross sectional area, or the surface area, increases towards the alveolar sacs
Alveoli in the Lung
- Alveoli are tiny sacs with a very thin wall
- Highly vascularised → many capillaries are in contact with the alveolar surface
- Amount of blood in capillaries is variable and changes with metabolic demand
Alveoli: Type I alveolar cells
- Are flat epithelial cells
- The internal surface of the alveoli is lined with liquid that contains a surfactant
- A surfactant is very important for stabilization of the alveolar sac
- Type I alveolar cells do not divide; susceptible to inhaled or aspirated toxins
Alveoli: Type II alveolar cells
- Are not found frequently in the alveoli
- Functions: They
- Produce the surfactant which is very important for respiratory function
- Can act as progenitor cells, have the ability to replicate and differentiate into Type I alveolar cells, which are produced in the late stage of development and stop replicating; they cannot be replaced when damaged by inhaled toxic agents
- Type II aveolar cells have potential for fixing damaged alveoli
Alveoli Properties
- Are highly vascularized
- Capillaries are very small (allowing for only a single RBC at a time)
- Estimated that in less than 1 second a RBC passes through the pulmonary capillary system
- This is sufficient time for oxygen and carbon dioxide diffusion between the alveoli and the capillary cells
O2 and CO2 Transfer between Alveolar Air and Blood:
- Transfers diffuse through the respiratory membrane
- Oxygen diffuses from the alveoli to the blood stream and carbon dioxide diffuses from the blood stream to the alveoli
- Respiratory membrane is the respiratory surface made of the alveolar epithelial cell (Type I alveolar cells) and the pulmonary capillary endothelial cell
- The respiratory surface is composed of alveolar fluid (with surfactant), alveolar epithelium, basement membrane of alveolar epithelium, interstitial space, basement membrane of capillary endothelium, capillary endothelium
- The membrane is very thin, easily damaged
- Pneumocyte → one of the cells lining the alveoli of lung (type I and type II alveolar cells)
Respiratory Airflow (Ventilation) Production
- Ventilation consists of moving gas from the atmosphere to alveoli by bulk flow independent of gas composition
- Movement is generated due to changes in volume and pressure that will push, or will promote, movement from areas of high pressure to areas of low pressure
- Exchange of oxygen and carbon dioxide exists between the alveoli and the blood system by diffusion
- Occurs at the level of the respiratory membrane due to changes in pressure of oxygen and carbon dioxide between the alveoli and the blood
- Oxygen and carbon dioxide are transported through pulmonary and systemic circulation by bulk flow
- Oxygen and carbon dioxide exists between blood in tissue capillaries and cells in tissues by diffusion
- The differential pressure between the blood and the peripheral tissue will drive oxygen from the blood to the peripheral tissue and carbon dioxide will move from the peripheral tissue to the blood to be eliminated at the next respiratory process
- Cellular utilization of oxygen and production of carbon dioxide drives the system
Ventilation Mechanics
- CNS sends an excitatory drive to respiratory motor neurons that innervate the respiratory muscles
- Respiratory muscles contract
- Changes the thoracic volume, the thoracic pressure, and intrapulmonary pressures
- Changes involving pressure allow for gas movement
- Air flows in and out with the different muscle contractions and relaxations
Respiratory Muscles
- There are 3 categories of muscles involved in respiration: pump muscles, airway muscles and accessory muscles
- Pump muscles make changes in pressure and volume at the level of the lungs
- Two classes allows air to come in and out:
- Inspiratory → Active throughout inspiration, main muscle: diaphragm
- Expiratory → Active throughout expiration
- Airways muscles are located at the level of the airways and have an important role in keeping the upper airways open
- Airways muscles are mostly inspiratory but there are some that are active in expiration
- Accessory muscles facilitate respiration during (leg) exercising, when there is an increased metabolic drive
- Brain coordinates the activity of various muscle groups for breathing
Inspiratory Pump Muscles: Diaphragm
- The diaphragm is the most important muscle for respiration
- It is active during inspiration; a dome-shaped structure, which separates the lungs from the abdominal content
- When the diaphragm contracts, it moves down, allowing the abdominal content to be pushed down, and the rib cage to be pushed outward, or widened; overall effect is an increase in the thoracic volume when it contracts
Inspiratory Pump Muscles: External Intercostal Muscles
- External intercostals contract and lift the rib cage, and this action promotes a lateral increase in the thoracic volume
- They contribute to the expansion of the thorax
- The motion of the rib cage caused by contraction of the external intercostal muscles is very similar to the motion of a bucket handle, and is called the bucket handle motion.
Inspiratory Pump Muscles: Parasternal Intercostal Muscles
- Parasternal intercostals contract and pull sternum forward, which increases anterior posterior dimension of the rib cage
- The motion is described as pump handle motion
Expiratory Pump Muscles: Abdominals
- Inspiratory pump muscles are active all the time during inspiration (during inspiration at rest or during exercise)
- Expiratory pump muscles:
- Do not contract during expiration at rest and passive during inspiration
- Are active during the expiratory phase when you are making an effort to breathe in and out (ie. During stress, exercise, coughing)
- Deeper, faster breathing requires active contraction of abdominal & internal intercostal muscles to return the lung to its resting position (Exercise)
Expiratory Pump Muscles: Internal Intercostal Muscles
- Internal intercostals are expiratory pump muscles
- They are relaxed at rest and recruited during forced expiration
- Internal intercostals push the rib cage down to reduce the amount of air or reduce the volume of the thoracic cage
Accessory Inspiratory Muscles
- Are not commonly active during resting breathing
- Are active during exercise and forced respiration
Inspiration and Expiration
- Quiet inspiration (rest): diaphragm contracts, pushing the abdominal content down and expanding the thorax as air comes in. The external intercostals and parasternal intercostals also contributes.
- During exercising or deep breathing: stronger contraction of the diaphragm and recruitment of the accessory muscles, further expanding the thoracic cavity
Expiration
- Quiet expiration (rest): at resting level, the abdominal and intercostal muscles are not active
- During quiet resting expiration, no muscles are recruited (no active contraction of the respiratory muscles)
- The inspiratory muscles relax and air moves out of the lungs because of the recoil of the lungs
- During forced expiration, abdominal muscles contract intensely
- Causes the abdominal content to be pushed upward so that the diaphragm is moved even higher than its resting level and more air is expelled
- Internal intercostal muscles contract and push the rib cage down
Upper Airway Muscles
- Most of the upper airways muscles are inspiratory; only a few are also expiratory
- Upper airway muscles are usually active during inspiration
- The main function is to keep the upper airways open in order to maintain the airway and allow for gas exchange
Obstructive Sleep Apnea
- State-dependent: when you sleep, the activity of these muscles tends to be depressed
- Healthy patient: air passes through the nasal and oral cavities and the tone of the tongue is maintained
- Obstructive sleep apnea: tone of the upper respiratory muscles is depressed and they become a floppy muscle
- Reduction in upper airway patency during sleep, or a reduction in the openness of the airway
- Air cannot go in and out, especially during sleep, resulting in snoring and large drops in oxygen saturation in the blood
- Consequences of this pathology include daytime sleepiness, changes in oxygen saturation in the blood (leading to cognitive impairment) and cardiovascular risks, such as hypertension
- Obstructive sleep apnea occurs as the result of a problem with the neural control of breathing
- Due to lack of excitatory drive, which is needed to maintain the tone of the respiratory muscles, as well as an anatomical defect
- No drugs available for treatment, the solution is often a mechanical device that delivers a continuous positive airway pressure through a nasal or full facial mask to gently push air into the airways to keep the upper airway passages open
Filtering Action: Conducting Zone & Muco-ciliary Escalator
- Regions involved in the filtering action: Conducting zone and at the level of the alveoli
- The filtering action in the conducting zone is called the muco-ciliary escalator
- Two types of cells line the surface of the trachea:
- Goblet cells are sparse and produce mucus
- Ciliated cells form a layer of cells with cilia on the apical surface
- Both cell types function in a coordinated manner to entrap inhaled biological and inert particulates and remove them from the airways
Removal of Deposited Particles in the Tracheobronchial Tree
- Effective clearance of deposited particles in the tracheobronchial tree requires both ciliary activity and respiratory tract fluids
- Ciliated cells:
- Cilia are able to continuously move
- Ciliary movement has preferential direction
- They produce periciliary fluid that has a very low density (quite liquid)
- The fluid sits on the top of the ciliated cells and is called the SOL layer, a low density of the fluid that allows the cilia to move freely in this fluid
- Goblet cells produce a very dense, thick mucus called the gel layer, this gell ayer is distributed in patches
- Goblet cells function to trap particulates that enter the respiratory system during inhalation
- Particulates is eliminated through the cilia movements; the cilia move in the SOL layer and the tip of the cilia touches the mucus and pushes it continuously in one direction
- Cilia movement is downward in the nasopharynx and upward at the level of the trachea to eliminate mucus through the esophagus
Muco-ciliary Escalator Effects
- Changes in the composition or in the thickness of the sol layer and the gel layer will affect the muco-ciliary escalator
- Smoking reduces the activity of the cilia and increases the number of mucus-producing goblet cells
Filtering Action: Macrophages in Alveoli
- Macrophages in the alveoli are the last defence against eliminating particulates
- Smallest particulates in the alveoli attract the macrophages which phagocytose these particulates, digesting them and eliminating the risk of infection
- Silica dust or asbestos are very fine particulates
- Macrophages recognize silica dust or particulates as a foreign object and phagocytose them, but they cannot digest these
- Silica dust and asbestos then break/ kill the macrophages which then disintegrate, releasing chemotactic factors and promoting recruitment of fibroblasts into the alveoli
- This increases the introduction of collagen, a protein that gives stiffness to the lungs
- Inhaling silica dust and asbestos results in the development of pulmonary fibrosis, and the lungs that are not able to expand lose their elastic properties
Spirometry
- Measures the amount and rate of inspired and expired air in a pulmonary function test
- Pressure transduces measures pressure and detects or quantifies the amount of air that is inspired and expired at each breath
Lung Volumes and Capacities
- Tidal volume → the volume of air moved IN OR OUT of the respiratory tract (Breathed) during each ventilatory cycle
- Expiratory reserve volume → the additional volume of air that can be forcibly exhaled following a normal expiration; it can be accessed simply by expiring maximally to the Maximum Voluntary Expiration
- Inspiratory reserve volume → the additional volume of air that can be forcibly inhaled following a normal inspiration; it can be accessed simply by inspiring maximally, to the Maximum Possible Inspiration
- Residual volume → the volume of air remaining in the lungs after a Maximal Expiration; it cannot be expired no matter how vigorous or long the effort; RV cannot be measured with a spirometry test; RV = FRC - ERV
- Always a small volume of air remaining in the lungs, prevents the lung collapsing
Lung Volumes and Capacities Continued
- Capacities: measurements of lung volume, and correspond to the sum of 2 or more lung volumes
- Vital capacity (VC) → the maximal volume of air that can be forcibly exhaled after a Maximal Inspiration; VC = TV + IRV + ERV
- Inspiratory capacity (IC) → the maximal volume of air that can be forcibly inhaled; IC = TV + IRV
- Functional Residual Capacity (FRC) → the volume of air remaining in the lungs at the end of a normal expiration; FRC = RV + ERV
- Total Lung Capacity (TLC) → the volume of air in the lungs at the end of a Maximal Inspiration; TLC = FRC + TV + IRV = VC + RV
Lung Volume and capacities limitations
- Cannot measure the residual volume with the spirometry test. For that reason it isn't possible to measure all the capacities that have residual volume as a component of the capacity itself
- Cannot measure (with the spirometry test) the functional residual capacity or the total lung capacity
Lung Volume and Flow
- Volume of air moved IN OR OUT of the respiratory tract during each ventilator cycle (at rest) is 500 mL
- Volume that enters the lungs, or enters the respiratory system doesn't rach the alveoli but remains in the conductive zone (has no alveoli and there is no gas exchange)
- Total or minute ventilation → volume of air that is exchanged within a rate time, or within a minute
- Total/minute ventilation = tidal volume x respiratory frequency
- Not all of this volume of air is available for gas exchange; we must take into consideration the anatomical dead space
- Alveolar ventilation is given by the equation: (0.5 - 0.15) L x 15/min.
- Must subtract the anatomical dead space of 150 mL (0.15 L) from the tidal volume of 0.5 L and multiply by the respiratory frequency of 15 per minute, this is how to calculate the alveolar ventilation
Ventilation: Recap
- Tidal volume is the volume of inspired air at each breath, equal to approximately 0.5 litres
- Total or minute ventilation is the total amount of air moved into the respiratory system per minute, calculated from the tidal volume multiplied by the respiratory frequency
- Alveolar ventilation is the amount of air moved into the alveoli per minute
- It is less than the minute ventilation as it depends on the anatomical dead space, and calculated by subtracting the anatomical dead space volume from the tidal volume, and multiplying by the respiratory frequency
- Tidal volume, or the air that comes into the respiratory system, is 500 mL or 0.5 L
Alveolar Ventilation
- Conducting airways have a volume of about 150 mL (volume of air that is left over from previous breath; no gas exchange in this region)
- About 1/3 of a normal breath is not available for gas exchange
- Exchange of gases with the blood occurs only in the alveoli
- At the end of expiration the lungs still have a specific amount of air
- When air goes in during an inspiratory effort, some of this air will enter the respiratory zone and will be available for gas exchange.
- This air is indicated as 350 mL in volume; it enters the respiratory zone and is available for gas exchange; a portion of this fresh atmosphere air from this inspiration will stay in the conductive airways (150mL) and will not be available for gas exchange
- When expiration occurs, there is elimination of the 350 mL of air that was present in the lungs and it was available for gas exchange, so it will be low in oxygen content and high in carbon dioxide levels when it is exhaled
- In contrast, the first part of the exhaled air, the 150 mL, will still be similar to the atmospheric air because it did not go through the gas exchange
- Alveoli ventilation is given by the difference of the tidal volume and the anatomical dead space multiplied by the frequency
- 𝑉𝐴 = (𝑉𝑇-𝑉𝐷) x frequency
- volume of the anatomic dead space is constant, independent from the volume inhaled at each respiration
Improvement of Alveoli and Alveolar Ventilation
- Deep slow breathing is prefered over shallow and fast breathing
- Divers inhale slowly and very deeply improving ventilation of the lung
- Deep and slow breathing increases alveoli ventilation, dedicating the majority of the minute ventilation to or available for gas exchange
- Deep breathing is more effective at increasing alveolar ventilation than is fast, shallow breathing
Spirometry Test – FEV1
- This measures the forced expiratory volume in 1 second and the forced vital capacity
- Ask the patient to make a maximal inspiration and then make an expiratory effort to exhale as much as they can and as fast as they can
- Two volumes can be determined in this test:
- Forced expiratory volume in 1 second (FEV-1) → forced expiratory volume is how much of the vital capacity volume that can be expelled in 1 second
- Forced vital capacity (FVC) → forced vital capacity is much the same as the vital capacity described earlier in the regular spirometry test
- Forced vital capacity (FVC) is about 5 litres in a healthy person
- A normal healthy person is able to expel in 1 second almost all of this volume
- 3 factors can be looked at in this test:
- Forced expiratory volume in 1 second (FEV-1): a healthy patient can normally expel most of the air from the lungs within 1 second
- Forced vital capacity (FVC): the total amount of air that is blown out in one breath after a max inspiration as fast as possible
- Ratio between the FEV-1 and FVC which represents the proportion of the amount of air that is blown out in 1 second
Diseases the Spirometry Test diagnose
- Is used to diagnose a patient for either an obstructive disease or a restrictive disease.
Obstructive Lung Disease
- Patients affected by obstructive lung disease have shortness of breath due to difficulty in exhaling all the air from their lungs
- Problem is with expiration, or with the ability to blow out the air from the lung, due to damage to the lungs or narrowing of the airways inside the lungs, and expired air comes out more slowly than normal
- Seen in patients affected by bronchial asthma, chronic obstructive pulmonary disease or cystic fibrosis
- In a Spirometry test,
- FEV-1 is significantly reduced in comparison to a normal calculation
- The process of expiration is also much slower, indicated by a lower slope of the graph in patients with obstructive pattern
- FVC, depending on the seriousness of the disease, can be normal or slightly reduced
- The ratio between FEV-1/FVC is also reduced (<0.7) with the following example
- Obstructive pattern ratio between FEV-1/FVC = 1.3/3.1 = 42 %
- Healthy person ratio between FEV-1/FVC = 4/5 = 80 %
- A normal healthy person, there is 80% of expulsion within the first second
Test for Obstructive Lung Disease
- Can be a diagnostic tool for patients with asthma who have continuous bronchospasms in the bronchi and an obstructive pattern of disease by performing this test before and after drug administration
- Improvement in the curve will tell if the drug is effective and reduces the bronchospasms
Restrictive Lung Disease
- Patient cannot fully fill their lungs because they are restricted from expanding
- Restrictive lung disease results from a condition causing stiffness in the lungs themselves. In other cases, stiffness of the chest wall, weak muscles, or damaged nerves may cause the restriction in lung expansion
- Spirometry test indicates that FVC is reduced
- The FVC is reduced in patients with restrictive pattern compared to normal because less air enters, so the IRV is much smaller than in a normal patient even though he has the full ability to expel air, the FEV-1 is reduced in comparison to a normal calculation Ratio between FEV-1/FVC will be similar to a normal healthy person, but the volume measured with FEV-1 and FVC will be reduced The disease is typical in patients affected by lung fibrosis, neuromuscular diseases or scarring of the lung tissue In lung fibrosis (asbestos and silica dust) there is an accumulation of collagen that makes the lung less elastic Reduced excitatory drive to the respiratory muscles in neuromuscular diseases like amyotrophic lateral sclerosis (ALS) and muscular dystrophy
Helium Dilution Method (Gas Dilution Technique)
- Spirometer cannot measure the air that remains in the lungs at the end of the forced expiration which is the residual volume
- Helium dilution method is used to measure the functional residual capacity (FRC = RV + ERV) or the amount of air that remains in the lungs at the end of a normal expiration
- Helium is an inert gas that is not taken up by the vascular system, but is confined to the lungs and able to move inside the respiratory system; concentration C2 is measured at the end of an expiratory effort (V2 = FRC) using the following equation V2 = V1 (C1-C2)/C2 measuring only communicating gas or ventilated lung volume
Mechanics of Ventilation
- Involve 2 classes of properties:
- Static properties of the lung that are present in the lungs when no air is flowing and are necessary to maintain lung and chest wall at a certain volume; intrapleural pressure (PIP), transpulmonary pressure (PPT), static compliance of the lung and surface tension of the lung
- Dynamic properties of the lung that are present when the lungs are changing volume and air is flowing in and out to permit airflow through Alveolar pressure, (main pressure necessary for generating airflow), dynamic lung compliance and airway and tissue resistance.
- Ventilation is the exchange of air between the atmosphere and the alveoli and occurs due to a change in that will pressure move air into and out of the lungs by bulk flow from a region of higher pressure to a region of lowers pressure
- Boyle's law maintains that for a fixed amount of an ideal gas that is kept at constant temperature, the pressure and the volume are inversely proportional where the product of pressure and volume will be a constant
Boyle's Law with air
- Gas molecules in a container (or alveolar space) continuously move and the space will be characterized by specific pressure and volume
- The pressure results from the continuous motion of the gas molecules in the container
- A reduction in the size/volume of the container will increase the pressure that the gas molecules exert
- During the expiratory phase of the lungs, this reduction in volume will generate an increase in alveolar pressure
- By increasing the size/volume of the container it will decrease the pressure that the gas molecules exert
- During the inspiratory phase of the lungs it will produce a decrease in alveolar pressure
Pressure Gradients
- Alveolar space in communication with the environment
- At rest conditions with no airflow, the atmospheric pressure will be equal to the alveolar pressure and a two space container, pressure in Area A and Area B will be equal An increase in Area B volume decreases pressure in Area B due to bulk flow properties that change in pressure
Ventilation Relationships: Volume and Pressure
To begin, in a two-space container, pressure in Area A (atmosphere) is equal to the pressure in Area B (alveoli) An increase in Area B volume decreases pressure in Area B due to bulk flow properties Gas molecules will move from a region that has a higher pressure: the atmosphere to a region that has a lower pressure: the alveoli This will occur until a new equilibrium A decrease in Area B volume increases pressure in Area B causing increased pressure in Area B compared to Area A and will move gas molecules from the region of high pressure to the region of low pressure: from the alveoli (Area B ) to the atmosphere (Area A) A change in volume, and then in pressure, produces airflow with flow generated by a difference in pressure between the atmosphere and the alveolar pressure Air moves via bulk flow from a region of high pressure to a region of low pressure Flow is measured as AP/R where P is preassure, where resistance is the pressure difference between 2 fixed points
Ventilation Effects
- If there is no pressure difference or, if the alveolar pressure is equal to the atmospheric pressure, there will be no air flow
- During inspiration
- Increasing thoracic volume will increase lung volume and the alveolar space will reduce the alveolar pressure
- the alveolar pressure is less than atmospheric pressure, air will move from the atmosphere outside into the lungs
- During expiration
- There is a reduction in the volume of the lungs and this compresses the gas molecules that are present in the alveoli
- There is an increase in alveolar pressure since alveolar pressure is greater than the atmospheric pressure, the air will move from the alveoli into the atmosphere
Lungs and The Thoracic Wall
- They are closely connected to a double layer of pleural tissue
- Lungs are embedded inside this pleural tissue called visceral pleura
- The inside of the chest wall is lined by another pleural tissue called the parietal pleura
- Visceral pleura and the parietal pleura are separated by intrapleural fluid which intrapleural fluid allows the 2 pleural tissues to slide around at each inspiratory effort
Recoil of Lungs and Chest Wall
- Interaction between lungs and thoracic cage determines lung volume where lungs tends to collapse due to elastic recoil, the walls tend to expand pulling thoracic cage due to elastic recoil -At equilibrium, inward elastic recoil of lungs exactly balances outward elastic recoil of chest wall which does no occur by direct attachment but through the intrapleural space between visceral and parietal pleurae
Pressures of Air Movement
During inspiration and expiration air moves in and out of the lungs due to variations of the: - intrapleural pressure (PIP) Transpulmonary pressure (PTP) intrapleural space acts as a relative vacuum, the intrapleural pressure is always negative which fluctuatees during breathing with opposing direction Alveolar Pressure (PALV) where atmospheric glotiss is open when equal
Pressure of Alveolar Gas
- Governs gas exchnage between Lungs and Atmosphere
- PALV governs gas exchange between Lungs and Atmosphere as governed By:
- F = AP/R which is the dynamic element directly involved in producing air flow due to differences been Alveolar Atmospheric Pressure
- Transpulmonary Pressure (PIP) is the force responsible for keeping the alveoli open, expressed as the pressure gradient
across the alveolar wall
- PIP = PALV - Pip where should be PALV > Pip in order to maintain the lungs expanded in the thorax where PTP is static that determines lung volume where as PALV is dynamic in determining airflow
Volume Differences
- During an inspiratory effort when muscle contracts during thoracic expasion then the Intraplerual presure Will become subatomospheric, as lungs continue to expand then the differece gets even bigger- To get differeccial to go towards high pressure and low volume for proper lung function
Airway Resistance
- Airway resistance to flow is generally small.
- a small AP produces flow Forces that can affect resistance to air flow: -Inertia of the respiratory system (minimal) vs a strong force that reduces frsiction (which has to do with intrapleural tissue to make frcition low) to reduce resistamce of air Resistance has a lot to do with the air, and is equal amount of energy needed to generate flow
Factors that Affect Airflow Resistance
- The subject invests relatively energy in airflow RESISTANCE; characteristic to the small airways that are distal to terminal bronchioles (in small airways like more small airways are at that distal to the lungs) * Transision -most common
- Turbulent -no lungular Airflow-no longer smooth, will always produce high flow like pharnyx, no loner smoth like laminar
- The radius will reduce to what its supposted to be
Respiratory Tract and Airways
- The air has to be pushed hard to open the lungs to increase its size to a high pressue
- As we are in respiratory, resistance will be higher and be arragned in a parelle
Airway Resistance in Disease
- Respiratory resistance is minimal, small can be pathegical, which result overall resistamce, this makes it difficule for the sujbect Because as a contracftion at at smooth msucle the air will increase
Lung and Air Compliance
- Can be determined for both dynamic( the way we test it ) or Static (no air has to be passing) lung complance Is measued for testing for Lung complance or elaticisty How lung is expanided in pressure
- In this test for testing to lungs, there will be no ar going in or our.
- Lung Fibrosis (low complance) will mean the patinet has to work hrad to exmabd that is responsible will cause small a big changfe in lung valume
- Emphasima- (high coplanace- Small tranpumanlity means large changes, there elastic but not working.
Dynamic Complance
- Dynamic = to elastic and arwya reistsamce that counter to expansoon
##Pressumate Vlume Releartionshi
Infltaon curve in difffertn then dflation
- Medium and small will be collaped, air will be every so slow As pressue increases not as lung chanage will occur Al lwing to be expdanoasnauly. air flow inti the sacs
Hysterisis
- There has to deal with elasctictiy or a measure for both behavior
###Elasticit and Coplanace
- Surface area will reduce resistamce
###Lecture 4 recording 17: Surface Tension and the Role of Surfactant
- All the above will allow for the lungs to breath
###Air Surface Treatment
- At that treatmernt water on surfacr has to treat the elastics
- At that time surfactant is there To help that is closer in that time No pressure = no alievols
###Lecture 4 recording 18: Regional Differences in Ventilation
- No = air is diffetn Less pressire is mor negative then can be a better lung functioms Alvieols do start are more deflated-receive more ventilation
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.