Podcast
Questions and Answers
What is the primary reason β2 agonists should not be used as the sole therapeutic agents for patients with persistent asthma?
What is the primary reason β2 agonists should not be used as the sole therapeutic agents for patients with persistent asthma?
- They have no anti-inflammatory effects. (correct)
- They are more expensive than other medications.
- They are only effective for exercise-induced asthma.
- They can cause severe bronchoconstriction.
Which of the following is a long-acting β2 agonist (LABA)?
Which of the following is a long-acting β2 agonist (LABA)?
- Levalbuterol
- Salmeterol (correct)
- Albuterol
- Formoterol (correct)
Inhaled corticosteroids (ICS) primarily function by targeting what aspect of asthma?
Inhaled corticosteroids (ICS) primarily function by targeting what aspect of asthma?
- Reducing airway inflammation. (correct)
- Increasing airway smooth muscle contraction.
- Directly dilating bronchi.
- Enhancing β2 agonist effects.
What is a common adverse effect minimized by inhaled delivery of β2 agonists compared to systemic administration?
What is a common adverse effect minimized by inhaled delivery of β2 agonists compared to systemic administration?
When should salmeterol or formoterol not be used?
When should salmeterol or formoterol not be used?
Which of the following statements is true regarding LABA monotherapy?
Which of the following statements is true regarding LABA monotherapy?
What is a potential short-term treatment for severe persistent asthma?
What is a potential short-term treatment for severe persistent asthma?
Which of these is not a typical adverse effect of β2 agonists?
Which of these is not a typical adverse effect of β2 agonists?
What is a primary action of inhaled corticosteroids (ICS) in asthma treatment?
What is a primary action of inhaled corticosteroids (ICS) in asthma treatment?
Which alternative drug is a selective inhibitor of 5-lipoxygenase?
Which alternative drug is a selective inhibitor of 5-lipoxygenase?
Leukotriene modifiers are primarily used in asthma therapy to:
Leukotriene modifiers are primarily used in asthma therapy to:
What is the mechanism of action for cromolyn in asthma treatment?
What is the mechanism of action for cromolyn in asthma treatment?
Which of the following is true about leukotriene receptor antagonists?
Which of the following is true about leukotriene receptor antagonists?
How frequently must cromolyn be administered due to its short duration of action?
How frequently must cromolyn be administered due to its short duration of action?
Which statement about leukotrienes is correct?
Which statement about leukotrienes is correct?
What are common adverse effects of using cromolyn?
What are common adverse effects of using cromolyn?
What is the primary characteristic of asthma?
What is the primary characteristic of asthma?
Which of the following factors may trigger an asthma attack?
Which of the following factors may trigger an asthma attack?
What role do β2-adrenergic agonists play in asthma treatment?
What role do β2-adrenergic agonists play in asthma treatment?
What is the purpose of having a ‘quick-relief’ medication for asthma patients?
What is the purpose of having a ‘quick-relief’ medication for asthma patients?
Which statement accurately describes the mechanism of asthma airflow obstruction?
Which statement accurately describes the mechanism of asthma airflow obstruction?
What is the duration of relief provided by short-acting β2 agonists (SABAs)?
What is the duration of relief provided by short-acting β2 agonists (SABAs)?
Why are local delivery methods preferred for administering asthma medications?
Why are local delivery methods preferred for administering asthma medications?
What additional effect can β2-adrenergic agonists have that patients should be aware of?
What additional effect can β2-adrenergic agonists have that patients should be aware of?
What is the primary reason ipratropium is not recommended for routine treatment of acute bronchospasm in asthma?
What is the primary reason ipratropium is not recommended for routine treatment of acute bronchospasm in asthma?
Which of the following is a potential adverse effect of theophylline overdose?
Which of the following is a potential adverse effect of theophylline overdose?
Why is theophylline less commonly used in asthma treatment today?
Why is theophylline less commonly used in asthma treatment today?
What is the mechanism of action of omalizumab in the treatment of asthma?
What is the mechanism of action of omalizumab in the treatment of asthma?
For which patients is omalizumab indicated in asthma treatment?
For which patients is omalizumab indicated in asthma treatment?
How often is omalizumab administered subcutaneously?
How often is omalizumab administered subcutaneously?
What should be monitored when a patient is using theophylline chronically?
What should be monitored when a patient is using theophylline chronically?
In what scenario can ipratropium provide additional benefit when treating acute asthma exacerbations?
In what scenario can ipratropium provide additional benefit when treating acute asthma exacerbations?
Study Notes
Respiratory Disorders Overview
- Major respiratory disorders include asthma, chronic obstructive pulmonary disease (COPD), allergic rhinitis, and cough.
Asthma
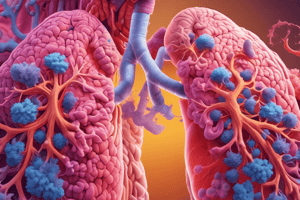
- Chronic inflammatory condition affecting airways, leading to bronchoconstriction, causing symptoms such as shortness of breath, cough, chest tightness, wheezing, and rapid respiration.
- Triggering factors include allergens, exercise, stress, and respiratory infections.
Pathophysiology
- Airflow obstruction arises from:
- Bronchial smooth muscle contraction
- Bronchial wall inflammation
- Increased mucus secretion
- Underlying airway hyperresponsiveness
Therapy Goals
- Key objectives are reducing symptom frequency and intensity, and improving patient quality of life.
- Patients must have quick-relief medication for acute symptoms.
- Long-term treatment focuses on reversing and preventing airway inflammation.
Drug Delivery Methods
- Methods include nasal mucosa delivery, inhalation to the lungs, or oral/parenteral routes for systemic absorption.
- Local delivery (inhalers, nasal sprays) minimizes systemic side effects.
β2 -Adrenergic Agonists
- Directly relax airway smooth muscle for quick relief of asthma symptoms.
- Short-acting β2 agonists (SABAs), e.g., albuterol and levalbuterol, provide relief within 5 to 30 minutes, lasting 4 to 6 hours.
Quick Relief with SABAs
- Essential for all asthma patients; however, not anti-inflammatory.
- Appropriate for intermittent asthma or exercise-induced bronchoconstriction.
Long-Term Control with LABAs
- Long-acting β2 agonists (LABAs) like salmeterol and formoterol provide bronchodilation for at least 12 hours.
- LABAs should not be used as monotherapy in chronic asthma; they require combination with inhaled corticosteroids (ICS).
Inhaled Corticosteroids (ICS)
- The first-line treatment for long-term asthma control.
- Effective for all degrees of persistent asthma in children and adults.
- ICS reduce airway inflammation and hyperresponsiveness when used regularly.
Alternative Drugs for Asthma Treatment
- Used when patients have poor control or adverse reactions to conventional therapies.
- Should be used alongside ICS, not as monotherapy.
Leukotriene Modifiers
- Work by inhibiting leukotriene production and blocking their receptor effects.
- Approved for asthma prevention; ineffective for immediate bronchodilation.
Cromolyn
- Prophylactic agent that prevents mast cell degranulation, but not useful for acute attacks.
- Requires frequent dosing, which can affect adherence.
Cholinergic Antagonists
- Ipratropium is useful for those intolerant to SABAs and provides additional benefit in acute situations.
Theophylline
- A bronchodilator with potential anti-inflammatory effects, now less commonly used due to its narrow therapeutic index.
- Requires monitoring and has significant drug interactions.
Monoclonal Antibody (Omalizumab)
- Targets human IgE to reduce allergic responses; used in patients with severe persistent asthma not controlled by other therapies.
- High cost and subcutaneous administration every 2 weeks limit its use; risk of rare anaphylactic reactions exists.
Case Study Context
- A 12-year-old girl with asthma develops cough and wheezing after exposure to a horse riding stable, highlighting the necessity for quick-relief medication in emergencies.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers key concepts related to the respiratory system, focusing on respiratory disorders such as asthma, chronic obstructive pulmonary disease (COPD), and allergic rhinitis. Understand the pathophysiology and symptoms associated with these conditions to deepen your knowledge of respiratory health.