Podcast
Questions and Answers
Which of the following scenarios would directly result from the respiratory system's role in regulating blood pH?
Which of the following scenarios would directly result from the respiratory system's role in regulating blood pH?
- Adjustments in breathing rate to compensate for metabolic acidosis. (correct)
- Improved vocal projection during public speaking.
- Increased oxygen delivery to muscles during exercise.
- Enhanced filtration of airborne particles in polluted environments.
A patient has difficulty warming and humidifying inhaled air. Which part of the respiratory system is MOST likely impaired?
A patient has difficulty warming and humidifying inhaled air. Which part of the respiratory system is MOST likely impaired?
- Trachea
- Nasal Cavity (correct)
- Bronchioles
- Larynx
If the diaphragm fails to contract, which of the following phases of breathing would be MOST affected?
If the diaphragm fails to contract, which of the following phases of breathing would be MOST affected?
- Vocalization
- Forced Expiration
- Inspiration (correct)
- Expiration
Which of the following BEST describes the relationship between external and internal respiration?
Which of the following BEST describes the relationship between external and internal respiration?
Which of the following changes would INCREASE the efficiency of external respiration?
Which of the following changes would INCREASE the efficiency of external respiration?
A person is experiencing a decreased tidal volume. Which of the following is the MOST likely consequence?
A person is experiencing a decreased tidal volume. Which of the following is the MOST likely consequence?
During a strenuous workout, which of the following responses is MOST likely to occur due to the respiratory system's function?
During a strenuous workout, which of the following responses is MOST likely to occur due to the respiratory system's function?
Damage to the larynx would MOST directly affect which of the following functions?
Damage to the larynx would MOST directly affect which of the following functions?
A patient with a tidal volume of 400 mL, a dead space of 160 mL, and a respiratory rate of 15 breaths per minute has what alveolar ventilation rate?
A patient with a tidal volume of 400 mL, a dead space of 160 mL, and a respiratory rate of 15 breaths per minute has what alveolar ventilation rate?
When a person takes a deep breath, which receptors prevent over-inflation of the lungs?
When a person takes a deep breath, which receptors prevent over-inflation of the lungs?
Which of the following is NOT a typical method of carbon dioxide transport in the blood?
Which of the following is NOT a typical method of carbon dioxide transport in the blood?
Why is the structure of the respiratory membrane essential for gas exchange?
Why is the structure of the respiratory membrane essential for gas exchange?
How do increased carbon dioxide levels in the blood affect the breathing rate, and why?
How do increased carbon dioxide levels in the blood affect the breathing rate, and why?
Which volume remains in the lungs even after a maximal exhalation?
Which volume remains in the lungs even after a maximal exhalation?
What is the primary function of surfactant in the alveoli?
What is the primary function of surfactant in the alveoli?
According to Dalton's Law, how do oxygen and carbon dioxide move during gas exchange in the lungs?
According to Dalton's Law, how do oxygen and carbon dioxide move during gas exchange in the lungs?
How does the Bohr effect influence oxygen transport?
How does the Bohr effect influence oxygen transport?
What is the Vital Capacity (VC) if a patient has a Tidal Volume (TV) of 500 mL, an Inspiratory Reserve Volume (IRV) of 3100 mL, and an Expiratory Reserve Volume (ERV) of 1200 mL?
What is the Vital Capacity (VC) if a patient has a Tidal Volume (TV) of 500 mL, an Inspiratory Reserve Volume (IRV) of 3100 mL, and an Expiratory Reserve Volume (ERV) of 1200 mL?
Flashcards
Respiratory System: Primary Function
Respiratory System: Primary Function
Facilitates gas exchange, provides O2, removes CO2.
Respiratory Organs
Respiratory Organs
Nasal Cavity, pharynx, larynx, trachea, bronchi, and lungs.
Inspiration
Inspiration
Air enters due to decreased pressure in the thoracic cavity.
Expiration
Expiration
Signup and view all the flashcards
External Respiration
External Respiration
Signup and view all the flashcards
Internal Respiration
Internal Respiration
Signup and view all the flashcards
Tidal Volume (TV)
Tidal Volume (TV)
Signup and view all the flashcards
Respiratory System: pH Regulation
Respiratory System: pH Regulation
Signup and view all the flashcards
Inspiratory Reserve Volume (IRV)
Inspiratory Reserve Volume (IRV)
Signup and view all the flashcards
Expiratory Reserve Volume (ERV)
Expiratory Reserve Volume (ERV)
Signup and view all the flashcards
Residual Volume (RV)
Residual Volume (RV)
Signup and view all the flashcards
Vital Capacity (VC)
Vital Capacity (VC)
Signup and view all the flashcards
Total Lung Capacity (TLC)
Total Lung Capacity (TLC)
Signup and view all the flashcards
Alveolar Ventilation Rate (AVR)
Alveolar Ventilation Rate (AVR)
Signup and view all the flashcards
Dead Space
Dead Space
Signup and view all the flashcards
Respiratory Centers
Respiratory Centers
Signup and view all the flashcards
Respiratory Membrane
Respiratory Membrane
Signup and view all the flashcards
Partial Pressure in Gas Diffusion
Partial Pressure in Gas Diffusion
Signup and view all the flashcards
Study Notes
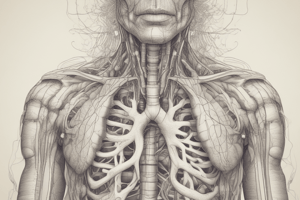
- The primary function of the respiratory system is gas exchange: delivering oxygen to the blood and removing carbon dioxide.
- The respiratory system regulates blood pH by controlling carbon dioxide levels.
- It enables vocalization for speech and sound production.
- Olfaction, or the sense of smell, is facilitated by air flowing over olfactory receptors in the nasal cavity.
- It offers defense against pathogens and particles with mucous and cilia.
- The respiratory system assists in thermoregulation through warming and humidifying inhaled air.
Locations and Functions of Respiratory Organs
- Nasal Cavity: Filters, warms, and moistens air and houses olfactory receptors.
- Pharynx: A passageway for air and food; involved in sound production.
- Larynx: Contains vocal cords and shields the trachea from food aspiration.
- Trachea: Conducts air to the bronchi and uses ciliated epithelium to trap particles.
- Bronchi and Bronchioles: Distribute air to the lungs. Bronchioles lead to alveoli for gas exchange.
- Lungs: The primary organs for respiration, facilitating gas exchange via alveoli.
Mechanics of Breathing
- Inspiration: The diaphragm contracts, increasing the thoracic cavity volume, reducing pressure and enabling air influx.
- Expiration: The diaphragm relaxes, decreasing thoracic cavity volume, increasing pressure, and forcing air out.
- Accessory muscles like intercostals aid in forced breathing.
- Breathing is managed by the medulla oblongata and pons in the brainstem.
- Normal breathing is rhythmic and involuntary but can be consciously controlled.
- Breathing is affected by lung compliance and airway resistance.
Internal vs. External Respiration
- External Respiration: Gas exchange occurs between alveoli and blood with O2 entering and CO2 exiting the blood.
- Internal Respiration: Gas exchange occurs between blood and tissues with O2 delivered to cells and CO2 collected.
- External respiration takes place in the lungs, while internal respiration occurs in systemic capillaries.
- Gas exchange efficiency depends on surface area, the thickness of the respiratory membrane, and partial pressures.
- Both respiration types are essential for cellular metabolism and homeostasis.
- Issues in either process lead to hypoxia (lack of oxygen) or hypercapnia (excess carbon dioxide)
Respiratory Air Volumes and Capacities
- Tidal Volume (TV): The air volume inhaled or exhaled during normal breathing; approximately 500 mL.
- Inspiratory Reserve Volume (IRV): The extra air that can be inhaled after a typical inhalation; approximately 3000 mL.
- Expiratory Reserve Volume (ERV): The additional air that can be exhaled after a normal exhalation; about 1200 mL.
- Residual Volume (RV): The air left in the lungs after maximum exhalation; about 1200 mL.
- Vital Capacity (VC): The total air exhaled after maximal inhalation, calculated as TV + IRV + ERV.
- Total Lung Capacity (TLC): The total lung volume, calculated as VC + RV.
Alveolar Ventilation Rate Calculation
- Alveolar ventilation rate (AVR) measures fresh air volume reaching the alveoli per minute.
- Calculation: AVR = (Tidal Volume - Dead Space) x Respiratory Rate.
- Dead space refers to non-gas exchange locations like the trachea and bronchi.
- Example: With TV=500 mL, Dead Space=150 mL, Respiratory Rate=12 breaths/min, AVR = (500 mL - 150 mL) x 12 = 4200 mL/min.
- AVR is essential for determining respiratory efficiency and health.
- AVR is affected by body position, lung disease, and physical activity.
Nonrespiratory Air Movements
- Coughing: Forceful air expulsion to clear airways.
- Sneezing: Similar to coughing but clears nasal passages, expelling irritants.
- Yawning: A deep inhalation to boost oxygen and stretch lung tissue.
- Hiccupping: Involuntary diaphragm contractions causing sudden air intake.
- Laughing and Crying: Rapid breathing changes affecting emotional states.
- These movements protect or signal physiological responses.
Control of Breathing
- Breathing is mainly managed by respiratory centers in the brainstem (medulla and pons).
- Chemoreceptors monitor carbon dioxide, oxygen, and pH levels in the blood.
- Increased carbon dioxide boosts breathing to expel CO2 and increase oxygen intake.
- Stretch receptors in the lungs prevent over-inflation during deep breaths.
- Voluntary control is possible via the cerebral cortex for activities like speaking or singing.
- Control center disorders can lead to conditions like sleep apnea or hyperventilation.
Structure and Function of the Respiratory Membrane
- The respiratory membrane includes alveolar epithelium, capillary endothelium, and fused basement membranes.
- It's very thin (0.5 micrometers) for efficient gas exchange.
- Alveoli have a large surface area (about 70 square meters) that enhances gas diffusion.
- Surfactant from type II alveolar cells lowers surface tension, preventing alveolar collapse.
- The membrane is important for maintaining the balance of oxygen and carbon dioxide in the blood.
- Pulmonary edema thickens the membrane, impairing gas exchange.
Importance of Partial Pressure in Gas Diffusion
- Gas exchange depends on partial pressures, per Dalton's Law.
- Oxygen and carbon dioxide diffuse from higher to lower partial pressure areas.
- In the lungs, oxygen's partial pressure is higher in alveoli than in blood, so it diffuses into the blood.
- Carbon dioxide diffuses from the blood (higher partial pressure) to the alveoli (lower partial pressure).
- Gas exchange efficiency is affected by altitude and lung health.
- Understanding partial pressures helps manage altitude sickness or respiratory failure.
Transport of Oxygen and Carbon Dioxide
- Oxygen primarily binds to hemoglobin in red blood cells for transport (98.5%).
- The rest of the oxygen is dissolved in plasma (about 1.5%).
- Carbon dioxide is transported dissolved in plasma (7%), bound to hemoglobin (23%), and as bicarbonate ions (70%).
- Carbonic anhydrase in red blood cells helps convert carbon dioxide to bicarbonate.
- The Bohr effect: Increased carbon dioxide and decreased pH enhance oxygen release from hemoglobin.
- Understanding these mechanisms is important for treating respiratory and circulatory disorders.
Gas Exchange in Pulmonary and Systemic Circuits
- In the pulmonary circuit, blood is oxygenated in the lungs; oxygen enters the blood, and carbon dioxide exits.
- In the systemic circuit, oxygen-rich blood is delivered to tissues, where oxygen is released and carbon dioxide is collected.
- Gas exchange efficiency depends on blood flow, ventilation-perfusion coupling, and alveolar health.
- Pulmonary embolism disrupts gas exchange by blocking blood flow.
- Understanding these processes helps diagnose and treat respiratory and cardiovascular diseases.
- Case studies of conditions like COPD and asthma show impaired gas exchange impacting overall health.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.