Podcast
Questions and Answers
What does a left-shifted oxygen saturation curve typically indicate?
What does a left-shifted oxygen saturation curve typically indicate?
- Decreased blood pH
- Decreased affinity of hemoglobin for oxygen
- Increased oxygen delivery to tissues
- Increased affinity of hemoglobin for oxygen (correct)
Which of the following molecules can outcompete oxygen for binding to hemoglobin?
Which of the following molecules can outcompete oxygen for binding to hemoglobin?
- Nitrous oxide ($N_2O$)
- Bicarbonate ($HCO_3^-$)
- Carbon monoxide ($CO$) (correct)
- Carbon dioxide ($CO_2$)
If a person has anemia but their oxygen saturation is measured at 100%, what is the most likely explanation?
If a person has anemia but their oxygen saturation is measured at 100%, what is the most likely explanation?
- They have a higher than normal concentration of hemoglobin
- Their hemoglobin is fully saturated, but they have a lower capacity to carry total oxygen (correct)
- They have an issue with their respiratory rate
- Their blood pH is higher than normal
What is the primary benefit of cooperative binding during hemoglobin binding?
What is the primary benefit of cooperative binding during hemoglobin binding?
What happens when someone’s oxygen saturation curve is shifted to the right?
What happens when someone’s oxygen saturation curve is shifted to the right?
What would be the effect on oxygen saturation in someone who is exercising compared to their saturation when resting, assuming no other change to variables?
What would be the effect on oxygen saturation in someone who is exercising compared to their saturation when resting, assuming no other change to variables?
Which of the following best describes 'homo' sites in respect to hemoglobin?
Which of the following best describes 'homo' sites in respect to hemoglobin?
What is the primary effect of having a low red blood cell (RBC) or hemoglobin (Hb) count on oxygen saturation?
What is the primary effect of having a low red blood cell (RBC) or hemoglobin (Hb) count on oxygen saturation?
What is the primary function of hemoglobin in relation to oxygen?
What is the primary function of hemoglobin in relation to oxygen?
If the oxygen saturation curve has a plateau, what does this indicate about the relationship between changes in partial pressure of oxygen (PO2) and oxygen saturation?
If the oxygen saturation curve has a plateau, what does this indicate about the relationship between changes in partial pressure of oxygen (PO2) and oxygen saturation?
Why does the binding affinity of hemoglobin for oxygen change as more oxygen molecules bind?
Why does the binding affinity of hemoglobin for oxygen change as more oxygen molecules bind?
What does the term 'cooperative binding' refer to in the context of hemoglobin and oxygen?
What does the term 'cooperative binding' refer to in the context of hemoglobin and oxygen?
In a typical scenario, around what percentage of hemoglobin is saturated with oxygen in the tissues near resting conditions?
In a typical scenario, around what percentage of hemoglobin is saturated with oxygen in the tissues near resting conditions?
What would cause the oxygen-hemoglobin dissociation curve to shift to the left?
What would cause the oxygen-hemoglobin dissociation curve to shift to the left?
What is meant by a 'right-shifted' hemoglobin saturation curve?
What is meant by a 'right-shifted' hemoglobin saturation curve?
Under what conditions would hemoglobin have the highest affinity for oxygen?
Under what conditions would hemoglobin have the highest affinity for oxygen?
Under what circumstances is it most difficult for hemoglobin to release oxygen?
Under what circumstances is it most difficult for hemoglobin to release oxygen?
What effect does increased levels of 2,3-BPG have on the hemoglobin saturation curve?
What effect does increased levels of 2,3-BPG have on the hemoglobin saturation curve?
How does a greater concentration of red blood cells or hemoglobin affect oxygen saturation potential?
How does a greater concentration of red blood cells or hemoglobin affect oxygen saturation potential?
What is the relationship between partial pressure of oxygen and hemoglobin saturation?
What is the relationship between partial pressure of oxygen and hemoglobin saturation?
What is the relationship between the partial pressure of oxygen (PO2) and the amount of oxygen bound to hemoglobin?
What is the relationship between the partial pressure of oxygen (PO2) and the amount of oxygen bound to hemoglobin?
What is the effect of decreased pH on the hemoglobin saturation curve, and where are you most likely to see that shift?
What is the effect of decreased pH on the hemoglobin saturation curve, and where are you most likely to see that shift?
When would you typically observe hemoglobin reaching 100% saturation?
When would you typically observe hemoglobin reaching 100% saturation?
What happens to the hemoglobin saturation curve during exercise?
What happens to the hemoglobin saturation curve during exercise?
Why is the binding of oxygen to hemoglobin considered 'cooperative'?
Why is the binding of oxygen to hemoglobin considered 'cooperative'?
What is the effect of a right shift in the oxygen-hemoglobin dissociation curve?
What is the effect of a right shift in the oxygen-hemoglobin dissociation curve?
What is the primary factor that determines the amount of oxygen being offloaded by hemoglobin?
What is the primary factor that determines the amount of oxygen being offloaded by hemoglobin?
How does the partial pressure of oxygen in the alveoli typically compare to that in the blood near the tissues?
How does the partial pressure of oxygen in the alveoli typically compare to that in the blood near the tissues?
What happens to the binding affinity of hemoglobin for oxygen after the first oxygen molecule binds?
What happens to the binding affinity of hemoglobin for oxygen after the first oxygen molecule binds?
If a hemoglobin molecule has less binding sites available, which condition is most likely?
If a hemoglobin molecule has less binding sites available, which condition is most likely?
What would you expect to see about oxygen's affinity to hemoglobin if there is a high partial pressure of carbon dioxide?
What would you expect to see about oxygen's affinity to hemoglobin if there is a high partial pressure of carbon dioxide?
Based on the saturation curve, if a tissue needs more oxygen, what mechanisms occur to increase O2 delivery?
Based on the saturation curve, if a tissue needs more oxygen, what mechanisms occur to increase O2 delivery?
What effect does increased PCO2 have on the hemoglobin saturation curve?
What effect does increased PCO2 have on the hemoglobin saturation curve?
Why is it important for most oxygen to remain bound to hemoglobin in blood circulation?
Why is it important for most oxygen to remain bound to hemoglobin in blood circulation?
What is the significance of the plateau in the oxygen-hemoglobin dissociation curve at high partial pressures of oxygen?
What is the significance of the plateau in the oxygen-hemoglobin dissociation curve at high partial pressures of oxygen?
A 'left shifted' hemoglobin curve indicates?
A 'left shifted' hemoglobin curve indicates?
Which of the following is a critical factor determining the amount of oxygen bound to hemoglobin?
Which of the following is a critical factor determining the amount of oxygen bound to hemoglobin?
Flashcards
Ligand
Ligand
A molecule that can bind to a specific site on another molecule, like how oxygen binds to hemoglobin.
Affinity
Affinity
The strength of the attraction between a ligand and its binding site. A higher affinity means the ligand binds more tightly.
Ligand
Ligand
A molecule that binds to a specific site on another molecule, like how oxygen binds to hemoglobin.
Affinity
Affinity
Signup and view all the flashcards
Anemia
Anemia
Signup and view all the flashcards
Oxygen Saturation
Oxygen Saturation
Signup and view all the flashcards
Oxygen Saturation Curve
Oxygen Saturation Curve
Signup and view all the flashcards
Left-shift in the oxygen saturation curve
Left-shift in the oxygen saturation curve
Signup and view all the flashcards
Oxygen Affinity
Oxygen Affinity
Signup and view all the flashcards
Oxygen Saturation Curve (Dissociation Curve)
Oxygen Saturation Curve (Dissociation Curve)
Signup and view all the flashcards
Plateau of the Oxygen Saturation Curve
Plateau of the Oxygen Saturation Curve
Signup and view all the flashcards
Linear Portion of the Oxygen Saturation Curve
Linear Portion of the Oxygen Saturation Curve
Signup and view all the flashcards
Right Shift of the Oxygen Saturation Curve
Right Shift of the Oxygen Saturation Curve
Signup and view all the flashcards
Left Shift of the Oxygen Saturation Curve
Left Shift of the Oxygen Saturation Curve
Signup and view all the flashcards
Oxygen Offloading
Oxygen Offloading
Signup and view all the flashcards
Oxygen Loading
Oxygen Loading
Signup and view all the flashcards
Cooperative Binding
Cooperative Binding
Signup and view all the flashcards
Polycythemia
Polycythemia
Signup and view all the flashcards
Hemoglobin Binding Competitor
Hemoglobin Binding Competitor
Signup and view all the flashcards
Oxygen Carrying Capacity
Oxygen Carrying Capacity
Signup and view all the flashcards
PO2
PO2
Signup and view all the flashcards
Hemoglobin Saturation Curve
Hemoglobin Saturation Curve
Signup and view all the flashcards
Oxygen Dissociation
Oxygen Dissociation
Signup and view all the flashcards
Left Shift
Left Shift
Signup and view all the flashcards
Right Shift
Right Shift
Signup and view all the flashcards
BPG (2,3-Bisphosphoglycerate)
BPG (2,3-Bisphosphoglycerate)
Signup and view all the flashcards
Sickle Cell Anemia
Sickle Cell Anemia
Signup and view all the flashcards
Normal Hemoglobin Saturation Curve
Normal Hemoglobin Saturation Curve
Signup and view all the flashcards
Alveolar PO2
Alveolar PO2
Signup and view all the flashcards
Percent Oxygen Saturation
Percent Oxygen Saturation
Signup and view all the flashcards
Oxygen Delivery
Oxygen Delivery
Signup and view all the flashcards
Increased Oxygen Demand
Increased Oxygen Demand
Signup and view all the flashcards
Tissue PO2
Tissue PO2
Signup and view all the flashcards
Right Shift during Exercise
Right Shift during Exercise
Signup and view all the flashcards
Study Notes
Chapter 13: The Respiratory System
- Respiration is the process of exchanging oxygen and carbon dioxide throughout the body
- Respiration involves three exchanges: air and lungs, lungs and blood, and blood and cells
- The respiratory system functions in gas transport in the blood and gas exchange between blood and cells
- The anatomy of the respiratory system reflects its physiological functions in gas exchange
Respiration
- Air and lungs exchange gases
- Lungs and blood exchange gases
- Blood and cells exchange gases
- Blood transport of gases (needs carriers like hemoglobin)
How Do Respiratory and Conducting Sections Differ?
- Airways are either conducting or respiratory
- Airways branch to reach alveoli
- Bigger airways contain more cartilage to prevent collapse
- Smaller airways are more numerous
- Conducting airways contain goblet cells, ciliated cells, clara cells, glands, cartilage, smooth muscle, and elastic fibers.
- Respiratory airways (alveoli) contain very thin epithelium for efficient gas exchange.
What Happens in the Conducting Airways?
- Mucociliary escalator helps warm and moisten airways, and clears foreign particulates
- Cilia in the bronchial epithelial wall moves mucus upwards towards the throat to clear the airways
The Airways in Cross Section
- Airways have muscle where inflammation can occur
- Airways have mucus glands
- Airways have cilia
Alveoli
- Alveoli are the primary site of gas exchange between air and blood
- Alveoli are tiny sacs in the lungs
- The alveoli wall is a single-layered epithelium to facilitate gas exchange
- Capillaries surround alveoli, allowing for efficient gas exchange between air and blood
Alveolar Cells
- Type I alveolar cells form the majority of the alveolar wall, facilitating rapid gas exchange.
- Type II alveolar cells produce surfactant which helps prevent alveolar collapse.
Arrangement of the Thorax (Muscle)
- Thoracic cavity, made of the rib cage, ribs, sternum, and diaphragm muscles work together to facilitate inhalation and exhalation.
- Accessory muscles of inspiration contract during forced inhalation.
- Muscles of expiration contract only during forced exhalation
Arrangement of Lungs in Pleural Sacs
- Lungs are in pleural sacs, containing fluid to reduce friction and tension.
- Pleural membranes help keep lungs close to the chest wall and reduce friction during breathing.
- Intrapleural pressure is always lower than alveolar pressure.
The Mechanics of Breathing: the role of Pleural pressure + Alveolar Pressure
- Atmospheric pressure is 760 mmHg
- Alveolar pressure is pressure in the alveoli
- Pleural pressure keeps the lungs attached to the chest wall
The Law of Laplace + Alveolar Stability
- Laplace's Law describes the pressure within a sphere.
- Surfactant reduces surface tension in the alveoli, thus preventing small alveoli from collapsing.
- Alveolar pressure is less in larger alveoli
- All alveoli in the same lung have the same pressure in normal breathing.
Pneumothorax
- Pneumothorax is a condition where air leaks into the pleural space; this causes lung collapse
Things that Make Respiration Possible
- Boyle's Law describes how pressure and volume are inversely proportional
- Gases move from higher to lower pressure.
- Lungs and thorax have compliance for expansion and recoil.
- Partial pressure gradients facilitate gas exchange.
Let's Put It All Together
- Inhalation involves expanding the thoracic cavity increasing volume and reducing intrapulmonary pressure.
- Exhalation involves decreasing the thoracic cavity volume increasing pressure and forcing air out.
Lung Volumes and Pressures
- Intrapulmonary pressure moves air into and out of the lungs
- Intrapulmonary pressure is lower during inspiration
Respiratory Cycle
- During inspiration, the volume of the thoracic cavity increases, and air moves into the lungs.
- During exhalation, the volume of the thoracic cavity decreases, and air moves out of the lungs.
The Role of Airway Diameter
- Airflow is proportional to pressure changes
- Resistance works against airflow and is inversely proportional to it.
- Airway diameter and resistance play an important role in respiration.
Now that We Have Gas in Lungs, How Do We Move it in the Body?
- Gases diffuse down partial pressure gradients
- Transport of gases.
Air is a Mixture
- Total pressure of a mixture is the sum of the partial pressures.
- Partial pressure is calculated by multiplying atmospheric pressure by the percentage of that gas in the air.
Review of the Respiratory Cycle
- Breathing is a process of inspiration and exhalation
- Inspiration is active and exhalation is passive, but both involve muscle contraction.
- Changes in chest size change the pressure inside the lungs, and air flows accordingly.
Let's Look at the Graphs Again!
- Alveolar pressure and flow rate have similar patterns
- A larger pressure gradient leads to faster airflow.
Why Does Air Change with Altitude?
- Air is always 21% oxygen
- Atmospheric pressure decreases with altitude, even though the proportion of gases remains the same.
These are Some Numbers to Know
- Lung function, pressure, volume, blood gas contents and exchange of the respiratory system.
How Is Oxygen Transported?
- Oxygen diffuses into red blood cells where it binds to hemoglobin; hemoglobin transports a vast majority of oxygen.
- Only a small percentage of oxygen is dissolved in plasma
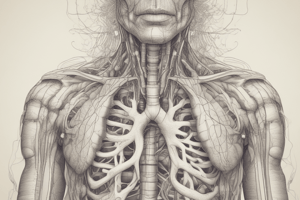
Hemoglobin
- Hemoglobin has four polypeptide chains per molecule
- Each hemoglobin molecule contains iron atoms which bind to oxygen
- Oxygen binding to hemoglobin is cooperative, meaning the binding of one oxygen molecule to Hb facilitates the binding of more.
- Hemoglobin's conformation changes allow for oxygen binding and release.
Oxygen Saturation Curves
- Hemoglobin's oxygen-binding affinity changes according to factors like pH, temperature, and the presence of certain molecules
- When pH decreases (more acidic), the curve shifts to the right (lower affinity) and releases more O2
- When pH increases (more basic), the curve shifts to the left (higher affinity) and binds more O2.
- The shape of the curve highlights how hemoglobin's affinity for oxygen changes with various levels.
How Can Someone Have 100% Saturation but Poor Oxygen Content?
- Someone with lots of Hb but low red blood cell or Hb count may have normal saturation, but poor oxygen content.
- Hemoglobin saturation, or the percentage of hemoglobin bound to oxygen, can be 100% but oxygen transport still may be impaired
Oxygen Saturation Curve
- The relationship between oxygen levels and hemoglobin saturation varies with factors such as pH, temperature, and concentration of certain substances like 2,3-bisphosphoglycerate
- Binding changes allow for oxygen release in tissues where it's needed more.
Hemoglobin Saturation Curves Again
- Conditions such as high carbon dioxide concentrations, low pH, elevated temperature, and the presence of BPG shift the oxygen-hemoglobin dissociation curve to the right, resulting in a lower affinity for oxygen. Conversely, a shift to the left indicates an increase affinity for oxygen.
- Blood and tissue pH, temperature and 2,3-BPG levels influence the position of the curve.
Oxygen Gets Stored in Hemoglobin
- Oxygen is stored in the blood in the form of oxyhemoglobin, but oxygen needs to be released into tissues.
- Oxygen release is affected by factors such as PCO2, pH, temperature, and 2,3-BPG concentrations
What About Carbon Dioxide?
- Carbon dioxide transport involves three mechanisms: dissolved in plasma, bound to Hb and bicarbonate ion.
- Carbonic anhydrase in red blood cells converts CO2 to bicarbonate, which is then transported out of the cell, maintaining the pH balance.
Told You It Was Complicated!
- Carbon dioxide transport mechanisms in the respiratory system.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.