Podcast
Questions and Answers
What is the function of the mucosa membrane in the stomach and intestines?
What is the function of the mucosa membrane in the stomach and intestines?
- Protection against corrosive acids
- Has epithelial folds for expansion and increasing surface area (correct)
- Release of water, acids, enzymes, buffers
- Serves as a barrier against bacteria
Which layer of the digestive tract is responsible for protecting tissues from corrosive acids and enzymes?
Which layer of the digestive tract is responsible for protecting tissues from corrosive acids and enzymes?
- Submucosa
- Mucosa (correct)
- Muscularis
- Serosa/adventitia
What is the main function of Excretion in the digestive system?
What is the main function of Excretion in the digestive system?
- Physical manipulation of solid foods
- Removal of wastes from body fluids (correct)
- Ingestion of food
- Chemical breakdown of food
What happens during Absorption in the digestive process?
What happens during Absorption in the digestive process?
Which part of the digestive system is involved in Mechanical processing?
Which part of the digestive system is involved in Mechanical processing?
What is the primary role of Secretion in the digestive system?
What is the primary role of Secretion in the digestive system?
Which layer of the digestive tract provides a nonspecific defense against bacteria?
Which layer of the digestive tract provides a nonspecific defense against bacteria?
What is the final step in the digestive process involving waste removal?
What is the final step in the digestive process involving waste removal?
What is the function of the afferent arteriole in the kidney?
What is the function of the afferent arteriole in the kidney?
Why does pressure increase in the kidneys due to the efferent arteriole?
Why does pressure increase in the kidneys due to the efferent arteriole?
What is Glomerular Filtration Rate (GFR) a measure of?
What is Glomerular Filtration Rate (GFR) a measure of?
How does Hydrostatic Pressure (HP) affect fluid movement?
How does Hydrostatic Pressure (HP) affect fluid movement?
What is Colloid Osmotic Pressure (COP) created by in the kidney environment?
What is Colloid Osmotic Pressure (COP) created by in the kidney environment?
When will water move out according to hydrostatic and colloid osmotic pressures?
When will water move out according to hydrostatic and colloid osmotic pressures?
What is Glomerular Hydrostatic Pressure (GHP) related to?
What is Glomerular Hydrostatic Pressure (GHP) related to?
What is Capsular Colloid Osmotic Pressure (CCOP) influenced by?
What is Capsular Colloid Osmotic Pressure (CCOP) influenced by?
What is the function of the greater omentum?
What is the function of the greater omentum?
What are compounds that do not dissociate called?
What are compounds that do not dissociate called?
Where do lingual tonsils situate?
Where do lingual tonsils situate?
In the context of fluid balance, what does excess gain require?
In the context of fluid balance, what does excess gain require?
What is the main function of the falciform ligament?
What is the main function of the falciform ligament?
Which of the following best describes electrolyte balance?
Which of the following best describes electrolyte balance?
What role do salivary glands play in the oral cavity?
What role do salivary glands play in the oral cavity?
What does the production of H+ ions being equal to their loss indicate in acid-base balance?
What does the production of H+ ions being equal to their loss indicate in acid-base balance?
Which factor results in a greater hold of water in muscle compared to adipose tissue?
Which factor results in a greater hold of water in muscle compared to adipose tissue?
What distinguishes the cheeks in the oral cavity?
What distinguishes the cheeks in the oral cavity?
How does the intracellular fluid volume compare to the plasma volume?
How does the intracellular fluid volume compare to the plasma volume?
Which part separates the oral nasal cavity and forms the roof of the mouth?
Which part separates the oral nasal cavity and forms the roof of the mouth?
What is the function of mesenteries in the abdominal cavity?
What is the function of mesenteries in the abdominal cavity?
Which body fluid compartment provides a constant environment?
Which body fluid compartment provides a constant environment?
'Orbicularis Oris' muscles are primarily found in which part of the oral cavity?
'Orbicularis Oris' muscles are primarily found in which part of the oral cavity?
What remains relatively constant in terms of fluid balance?
What remains relatively constant in terms of fluid balance?
What type of epithelium lines the nasopharynx for the exchange of small amounts of air with auditory tubes?
What type of epithelium lines the nasopharynx for the exchange of small amounts of air with auditory tubes?
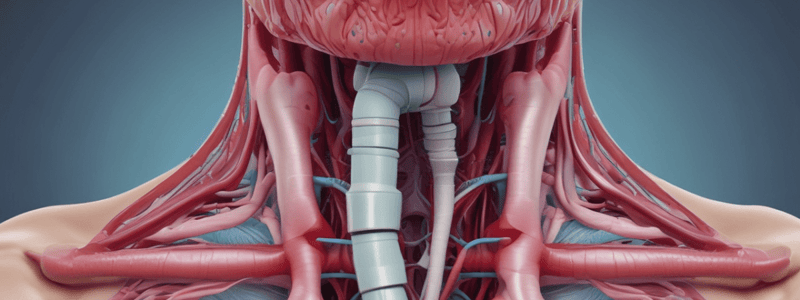
Which of the following is NOT part of the larynx?
Which of the following is NOT part of the larynx?
What is the function of the epiglottis during swallowing?
What is the function of the epiglottis during swallowing?
Which ligaments extend across the larynx between the thyroid and smaller cartilages?
Which ligaments extend across the larynx between the thyroid and smaller cartilages?
What is the main function of the true vocal cords in the larynx?
What is the main function of the true vocal cords in the larynx?
Which muscle type connects cartilages and structures in the throat?
Which muscle type connects cartilages and structures in the throat?
What causes variation in pitch related to tension in the vocal cords?
What causes variation in pitch related to tension in the vocal cords?
Which condition is characterized by viscous mucus impairing cilia and blocking air passageways?
Which condition is characterized by viscous mucus impairing cilia and blocking air passageways?
Where is the only layer present in capillaries located?
Where is the only layer present in capillaries located?
What happens when there is incompetence in the valves of veins?
What happens when there is incompetence in the valves of veins?
What is the function of peripheral veins' increased number of valves?
What is the function of peripheral veins' increased number of valves?
Which part of the heart's circulation carries 30-35% of the blood volume?
Which part of the heart's circulation carries 30-35% of the blood volume?
In what direction does blood flow from the right ventricle to lung arterioles in pulmonary circulation?
In what direction does blood flow from the right ventricle to lung arterioles in pulmonary circulation?
Which layer of blood vessels contains smooth muscle in both arteries and veins?
Which layer of blood vessels contains smooth muscle in both arteries and veins?
What differentiates venules from veins in terms of blood entry?
What differentiates venules from veins in terms of blood entry?
What defines pulmonary circulation in the heart's blood flow?
What defines pulmonary circulation in the heart's blood flow?
Which force encourages fluid to leave the glomerular capillaries and move into the capsular space?
Which force encourages fluid to leave the glomerular capillaries and move into the capsular space?
What does the Equilibrium Filtration Pressure (EFP) represent in the context of fluid dynamics in the kidneys?
What does the Equilibrium Filtration Pressure (EFP) represent in the context of fluid dynamics in the kidneys?
What is the main function of Myogenic Mechanism in regulating Glomerular Filtration Rate (GFR)?
What is the main function of Myogenic Mechanism in regulating Glomerular Filtration Rate (GFR)?
What is directly correlated with the body's systemic blood pressure?
What is directly correlated with the body's systemic blood pressure?
How does an increase in afferent arteriole diameter affect Glomerular Filtration Rate (GFR)?
How does an increase in afferent arteriole diameter affect Glomerular Filtration Rate (GFR)?
What could be a consequence of decreased Glomerular Filtration Rate (GFR) due to lowered systemic blood pressure?
What could be a consequence of decreased Glomerular Filtration Rate (GFR) due to lowered systemic blood pressure?
Which combination of forces make up the Equilibrium Filtration Pressure (EFP) in the kidneys?
Which combination of forces make up the Equilibrium Filtration Pressure (EFP) in the kidneys?
What factor triggers smooth muscle contraction in afferent arterioles resulting in decreased blood flow and Glomerular Filtration Rate (GFR)?
What factor triggers smooth muscle contraction in afferent arterioles resulting in decreased blood flow and Glomerular Filtration Rate (GFR)?
What is the function of macula densa cells in the kidney?
What is the function of macula densa cells in the kidney?
Which cells release erythropoietin to stimulate the production of red blood cells?
Which cells release erythropoietin to stimulate the production of red blood cells?
What is the role of the juxtaglomerular cells in the kidney?
What is the role of the juxtaglomerular cells in the kidney?
Which system is activated when macula densa cells signal low solutes or glomerular filtration rate?
Which system is activated when macula densa cells signal low solutes or glomerular filtration rate?
What initiates a series of enzymatic reactions known as RAS?
What initiates a series of enzymatic reactions known as RAS?
Which cells in the kidney are responsible for determining the status of solute levels in the distal convoluted tubule?
Which cells in the kidney are responsible for determining the status of solute levels in the distal convoluted tubule?
What hormones are secreted by macula densa and juxtaglomerular cells?
What hormones are secreted by macula densa and juxtaglomerular cells?
What term is used to describe compounds that do not dissociate into ions?
What term is used to describe compounds that do not dissociate into ions?
Which body fluid compartment facilitates intracellular chemical reactions?
Which body fluid compartment facilitates intracellular chemical reactions?
What is the main factor that influences the greater hold of water in muscle compared to adipose tissue?
What is the main factor that influences the greater hold of water in muscle compared to adipose tissue?
In the context of fluid balance, what does excess loss require?
In the context of fluid balance, what does excess loss require?
What is the primary function of the extracellular fluid (ECF) compartment?
What is the primary function of the extracellular fluid (ECF) compartment?
What is the primary function of the phosphate buffer system?
What is the primary function of the phosphate buffer system?
In maintaining acid-base balance, what happens when there is a shortage of H+?
In maintaining acid-base balance, what happens when there is a shortage of H+?
How does the carbonic acid bicarbonate buffer system respond to excess H+?
How does the carbonic acid bicarbonate buffer system respond to excess H+?
What is the role of respiratory compensation in acid-base balance?
What is the role of respiratory compensation in acid-base balance?
If the blood pH exceeds normal limits, what would be the expected result on respiration?
If the blood pH exceeds normal limits, what would be the expected result on respiration?
What occurs during prolonged hyperventilation in relation to blood pH?
What occurs during prolonged hyperventilation in relation to blood pH?
How do the kidneys respond to an increase in blood pH?
How do the kidneys respond to an increase in blood pH?
What is the main function of carbolic acid Bicarbonate buffer system?
What is the main function of carbolic acid Bicarbonate buffer system?
What is the primary function of the Superior vena cava in the circulatory system?
What is the primary function of the Superior vena cava in the circulatory system?
Where do the Veins of the upper limb receive blood from according to the text?
Where do the Veins of the upper limb receive blood from according to the text?
In which part of the body are the Extensions of capillaries mentioned in the text?
In which part of the body are the Extensions of capillaries mentioned in the text?
What is the main source of blood for Inferior vena cava according to the provided text?
What is the main source of blood for Inferior vena cava according to the provided text?
Which part of the body receives blood supply from branches of subclavian arteries and descending thoracic aorta?
Which part of the body receives blood supply from branches of subclavian arteries and descending thoracic aorta?
Where do the Veins of the head and neck drain into according to the text?
Where do the Veins of the head and neck drain into according to the text?
What is one significant feature of the Systemic Circulation mentioned in the text?
What is one significant feature of the Systemic Circulation mentioned in the text?
What distinguishes the Veins of the thorax and abdomen based on their drainage outlets?
What distinguishes the Veins of the thorax and abdomen based on their drainage outlets?
What is the specialized area in the heart composed of myocytes that can spontaneously depolarize called?
What is the specialized area in the heart composed of myocytes that can spontaneously depolarize called?
Which structure initiates each heartbeat and sets the pace for the heart's contractions?
Which structure initiates each heartbeat and sets the pace for the heart's contractions?
What term is used to describe the property of being able to spontaneously initiate depolarization in heart muscle cells?
What term is used to describe the property of being able to spontaneously initiate depolarization in heart muscle cells?
Why does the heart not require the central nervous system (CNS) to maintain its rhythm?
Why does the heart not require the central nervous system (CNS) to maintain its rhythm?
What happens when autorhythmic cells in the heart reach a specific threshold?
What happens when autorhythmic cells in the heart reach a specific threshold?
Which term best describes the rhythmic electrical activity produced by autorhythmic cells in the heart?
Which term best describes the rhythmic electrical activity produced by autorhythmic cells in the heart?
Where are the specialized pacemaker cells located that initiate each heartbeat in the heart's conduction system?
Where are the specialized pacemaker cells located that initiate each heartbeat in the heart's conduction system?
What characteristic allows autorhythmic cells in the heart to start an action potential without external stimulation?
What characteristic allows autorhythmic cells in the heart to start an action potential without external stimulation?
What is the main function of the RENIN-ANGIOTENSIN-ALDOSTERONE SYSTEM (RASS) in the kidney?
What is the main function of the RENIN-ANGIOTENSIN-ALDOSTERONE SYSTEM (RASS) in the kidney?
What triggers the release of renin in the kidneys?
What triggers the release of renin in the kidneys?
Where are the macula densa cells located within the kidney?
Where are the macula densa cells located within the kidney?
What is the primary function of juxtaglomerular cells in the kidney?
What is the primary function of juxtaglomerular cells in the kidney?
Which hormone is responsible for stimulating the production of red blood cells?
Which hormone is responsible for stimulating the production of red blood cells?
What enzymatic reactions are set off by renin in response to low solutes/GFR?
What enzymatic reactions are set off by renin in response to low solutes/GFR?
Where are juxtaglomerular cells predominantly found within the kidney?
Where are juxtaglomerular cells predominantly found within the kidney?
What do macula densa cells act as in the kidney environment?
What do macula densa cells act as in the kidney environment?
What might be the consequence of hypotension leading to hypo-perfusion of critical organs?
What might be the consequence of hypotension leading to hypo-perfusion of critical organs?
What is the primary function of lymphatics leaving nodes to form principal lymphatic trunks?
What is the primary function of lymphatics leaving nodes to form principal lymphatic trunks?
What is the role of lacteals in lymphatic capillaries?
What is the role of lacteals in lymphatic capillaries?
What causes lymphedema, resulting in limb swelling?
What causes lymphedema, resulting in limb swelling?
How does lymph flow through the lymphatic capillaries and vessels?
How does lymph flow through the lymphatic capillaries and vessels?
What is the main function of the skeletal muscle pump in the flow of lymph?
What is the main function of the skeletal muscle pump in the flow of lymph?
In what way does respiratory lymph flow contribute to the movement of lymph?
In what way does respiratory lymph flow contribute to the movement of lymph?
'Milking action' is a term associated with which process in the context of lymph flow?
'Milking action' is a term associated with which process in the context of lymph flow?
What is the main function of the countercurrent exchanger in the kidney system?
What is the main function of the countercurrent exchanger in the kidney system?
In the recycling of urea, what is the role of the medullary collecting system?
In the recycling of urea, what is the role of the medullary collecting system?
What drives the process of osmosis in renal filtration and urine concentration?
What drives the process of osmosis in renal filtration and urine concentration?
What is a key function of renal clearance measurement?
What is a key function of renal clearance measurement?
How does the micturition reflex contribute to urine ejection?
How does the micturition reflex contribute to urine ejection?
What is a common cause of adult urinary incontinence related to muscle weakness?
What is a common cause of adult urinary incontinence related to muscle weakness?
How does the vasa recta contribute to maintaining a concentration gradient in the medulla?
How does the vasa recta contribute to maintaining a concentration gradient in the medulla?
What effect does ADH have on water reabsorption in the medullary collecting duct?
What effect does ADH have on water reabsorption in the medullary collecting duct?
Which lymphatic organ secretes thymosin to stimulate cell division and T cell maturation?
Which lymphatic organ secretes thymosin to stimulate cell division and T cell maturation?
Which immune cells account for 25% of circulating White Blood Cells (WBCs) in the body?
Which immune cells account for 25% of circulating White Blood Cells (WBCs) in the body?
In which organ do plasma cells primarily develop from B cells to produce antibodies?
In which organ do plasma cells primarily develop from B cells to produce antibodies?
Which lymphoid organ is the largest collection of lymphoid tissue in the body and functions in the removal of microbes from blood?
Which lymphoid organ is the largest collection of lymphoid tissue in the body and functions in the removal of microbes from blood?
Which immune response involves T cells defending against abnormal and infected cells in the body?
Which immune response involves T cells defending against abnormal and infected cells in the body?
What is the primary function of the lymphocytes found in the lymph nodes during an immune response?
What is the primary function of the lymphocytes found in the lymph nodes during an immune response?
What triggers a cell-mediated attack against recipient tissue in graft versus host disease?
What triggers a cell-mediated attack against recipient tissue in graft versus host disease?
Which autoimmune disease is characterized by antibodies that mimic Thyroid Stimulating Hormone (TSH)?
Which autoimmune disease is characterized by antibodies that mimic Thyroid Stimulating Hormone (TSH)?
In autoimmune diseases involving antibody reactions, which condition involves antibodies preventing the binding of Acetylcholine (Ach) to its receptors?
In autoimmune diseases involving antibody reactions, which condition involves antibodies preventing the binding of Acetylcholine (Ach) to its receptors?
Which autoimmune disease involves T cells and macrophages attacking the myelin sheath of nerves?
Which autoimmune disease involves T cells and macrophages attacking the myelin sheath of nerves?
Which immune response fails to develop or is blocked in immunodeficiency diseases?
Which immune response fails to develop or is blocked in immunodeficiency diseases?
What do autoimmune disorders primarily target in the body?
What do autoimmune disorders primarily target in the body?
In immunotherapy for cancer, what is the goal of using antibodies like Herceptin?
In immunotherapy for cancer, what is the goal of using antibodies like Herceptin?
'Grafts' that lead to an immune response when transplanted between people (non-twins) are known as:
'Grafts' that lead to an immune response when transplanted between people (non-twins) are known as:
'Immunosuppression' in allograft recipients primarily targets which aspect of immunity?
'Immunosuppression' in allograft recipients primarily targets which aspect of immunity?
What is the principal type of hypersensitivity reaction characterized by IgE antibodies combining with antigens?
What is the principal type of hypersensitivity reaction characterized by IgE antibodies combining with antigens?
Which immune response involves the activation of T cells and B cells to inactivate pathogens and abnormal cells?
Which immune response involves the activation of T cells and B cells to inactivate pathogens and abnormal cells?
What is a common mediator involved in triggering anaphylactic shock by causing vasodilation of peripheral blood vessels?
What is a common mediator involved in triggering anaphylactic shock by causing vasodilation of peripheral blood vessels?
In autoimmune diseases, what is the purpose of producing IgG instead of IgE through desensitization?
In autoimmune diseases, what is the purpose of producing IgG instead of IgE through desensitization?
Which type of hypersensitivity reaction involves prolonged contraction of smooth muscles triggered by leukotrienes and prostaglandins?
Which type of hypersensitivity reaction involves prolonged contraction of smooth muscles triggered by leukotrienes and prostaglandins?
What is the immediate trigger for degranulation in anaphylactic reactions characterized by an immediate response?
What is the immediate trigger for degranulation in anaphylactic reactions characterized by an immediate response?
Study Notes
Nasopharynx
- Located from internal nares to soft palate
- Pseudostratified ciliated epithelium
- Exchanges small amounts of air with auditory tubes
Oropharynx
- Located from soft palate to hyoid bone
- Stratified squamous epithelium
- Contains palatine and lingual tonsils
Laryngopharynx
- Located from hyoid bone to esophagus
- Stratified epithelium
- Contains epiglottis, thyroid cartilage, and cricoid cartilage
- 2 pairs of smaller cartilages: arytenoid, corniculate, and cuneiform
Larynx
- Consists of 9 pieces of cartilage
- Epiglottis folds back to prevent food from entering trachea during swallowing
- Thyroid cartilage forms the Adam's apple
- Cricoid cartilage provides support and protects the glottis and trachea
Vocal Cords
- Upper ligaments: false vocal cords
- Lower folds: true vocal cords (principal structures in voice production)
- Tension in vocal cords affects pitch
Trachea
- Also known as the windpipe
- Located anterior to esophagus and attached to cricoid cartilage
- Branches into bronchi
- Semi-circular cartilaginous rings protect the airway
Bronchi
- Primary bronchi divide into secondary lobar bronchi
- Secondary bronchi branch into tertiary segmental bronchi
- Bronchioles: narrow, cartilage-free, and dominated by smooth muscle
- Diameter of passageway controlled by sympathetic and parasympathetic nervous systems
Digestive System
- Consists of a muscular tube (digestive tract) and accessory organs
- Functions: ingestion, mechanical processing, digestion, secretion, absorption, and excretion
Digestive Tract Layers
- Mucosa: protects tissues from corrosive acids and enzymes
- Submucosa: provides mechanical support
- Muscularis: contracts and relaxes to mix and propel food
- Serosa/Adventitia: outermost layer
Urinary Physiology
- Filtration: glomerular hydrostatic pressure (GHP) > capsular colloid osmotic pressure (CCOP)
- Balance: input = output
- Fluid balance: fluid gained = fluid lost
- Electrolyte balance: no net gain or loss of ions
Acid-Base Balance
- Regulated by buffer systems: protein, phosphate, and bicarbonate
- Respiratory compensation: exhalation of CO2 and H+ buffering
- Renal compensation: H+ excretion and bicarbonate ion reabsorption
Lymphatic System
- Components: vessels, fluid, lymphocytes, lymphoid tissues and organs
- Functions: production, maintenance, distribution of lymphocytes, return of fluid and solutes, and hormone and nutrient distribution
Lymphatic Vessels
- Capillaries: smallest vessels, absorb proteins and lipids
- Trunks and ducts: lymphatics unite to form principle lymphatic trunks
- Thoracic duct: main return of venous blood
Skeletal Muscle Pump
- Contractions compress lymphatic vessels, forcing lymph toward the heart### The Heart as a Pump
- Initiates each heartbeat through the sinoatrial (SA) node, which is located in the right atrial wall and has specialized pacemaker cells with an intrinsic rhythm called autorhythmicity.
- Autorhythmic cells spontaneously depolarize at a given rate, resulting in an action potential that starts when cells reach threshold.
Regulation of Blood Pressure
- BP drop: arterioles dilate, increasing blood flow and GFR (glomerular filtration rate).
- Vasoconstriction: decreases blood flow into the glomerulus.
- Vasodilation: increases blood flow into the glomerulus.
Renal Regulation
- Tubuloglomerular feedback: a localized response that regulates the size of afferent and efferent arterioles, depending on the functioning of macula densa cells and juxtaglomerular cells.
- Macula densa cells: chemoreceptors that determine the status of the filtrate in the distal convoluted tubule.
- Juxtaglomerular cells: mechanoreceptors that detect stretching of the afferent arteriole and release renin when solutes/GFR are too low.
Renin-Angiotensin-Aldosterone System (RAS)
- Renin release: triggers a series of enzymatic reactions to regulate blood pressure.
- Erythropoietin: stimulates production of RBCs.
Countercurrent Systems
- Countercurrent multiplier system: fluid travels in opposite directions, with Na, K, and Ca actively transported from filtrate into interstitial fluid.
- Recycling of urea: medullary collecting system reabsorbs urea, concentrating it in the interstitial fluid.
- Countercurrent exchanger: maintains the concentration gradient in the medulla.
Urine Composition and Regulation
- Urine contains: water, Na, K, Cl, H, phosphate, sulfates, metabolic wastes, and small amounts of bicarbonate, Ca, and Mg.
- Renal clearance: measures the rate at which the kidneys remove a substance from the blood.
- Regulation of urine concentration: depends on the concentration gradient in the interstitial fluid.
Micturition Reflex
- Stretch receptors in the bladder wall stimulate the brain, leading to the contraction of the detrusor muscle and the relaxation of the internal and external sphincters.
- Voluntary relaxation of the external urethral sphincter causes the relaxation of the internal urethral sphincter, resulting in urination.
Urinary Incontinence
- Lack of voluntary control, resulting in the involuntary loss of urine.
- Types: stress, urge, overflow, and functional incontinence.
Overview of the Urinary System
- Filtration produces a filtrate resembling blood plasma.
- Reabsorption and secretion occur in the proximal convoluted tubule and other segments of the nephron.
- Final composition and concentration of urine are determined by the distal convoluted tubule and collecting ducts.
Fluid, Electrolyte, and Acid-Base Homeostasis
- Chemical bonds between molecules permit dissociation.
- Type II (cytotoxic) reaction: activates complement via the classical pathway, leading to cytolysis.
- Type III (immune complex) reaction: occurs when antigen is in excess, leading to inflammatory damage.
- Type IV (delayed cell-mediated) reaction: involves T cells and macrophages, resulting in an inflammatory response.
Immune System
- Primary lymphatic organs: bone marrow and thymus.
- Secondary lymphatic organs: spleen, lymph nodes, tonsils, etc.
- Thymus: develops and matures T cells, which attack foreign or abnormal cells.
- Lymphocytes: account for 25% of circulating WBCs, including T cells, B cells, and NK cells.
Lymphatic Organs
- Spleen: largest collection of lymphoid tissue, responsible for defense, hematopoiesis, RBC/platelet destruction, and blood reservoir.
- Lymph nodes: filter lymph, removing microbes and other injurious particles.
- Tonsils: masses of lymphoid tissue, protecting the pharynx from exterior threats.
Immune Response
- Purpose: to inactivate/destroy pathogens and/or abnormal cells.
- Involves coordinated activities of T cells and B cells.
- Cell-mediated immunity: defends against abnormal cells, infected cells.
- Antibody-mediated immunity: defends against antigens on body fluids.
Hypersensitivity
- Anaphylactic (Type I) reaction: an immediate response, involving IgE antibodies.
- Cytotoxic (Type II) reaction: triggered by the binding of antibodies to antigens on cell surfaces.
- Immune complex (Type III) reaction: occurs when antigen is in excess, leading to inflammatory damage.
- Cell-mediated (Type IV) reaction: involves T cells and macrophages, resulting in an inflammatory response.
Preventing Anaphylactic Reactions
- Skin tests: diagnose allergies by inoculating small amounts of antigen beneath the epidermis.
- Desensitization: series of injections gradually increasing doses of antigen, aiming to produce IgG instead of IgE.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on the anatomy of the respiratory system, including the structures from the nasopharynx to the larynx and their specific characteristics. Learn about the different types of epithelium, cartilages, and functions of each part.