Podcast
Questions and Answers
In the context of respiratory physiology, increased thoracic cavity volume during inspiration directly leads to:
In the context of respiratory physiology, increased thoracic cavity volume during inspiration directly leads to:
- An increase in intrapulmonary pressure.
- Relaxation of intercostal muscles.
- Contraction of the diaphragm.
- A decrease in intrapulmonary pressure. (correct)
Which of the following best describes the primary function of surfactant in the respiratory system?
Which of the following best describes the primary function of surfactant in the respiratory system?
- Preventing the epiglottis from collapsing.
- Decreasing the surface tension of the alveoli. (correct)
- Increasing the surface tension of the alveoli.
- Facilitating gas exchange in the bronchioles.
A patient with a decreased level of consciousness begins to exhibit shallow, irregular breathing. Which of the following terms best describes this condition?
A patient with a decreased level of consciousness begins to exhibit shallow, irregular breathing. Which of the following terms best describes this condition?
- Apnea
- Hypoventilation (correct)
- Hyperventilation
- Dyspnea
What is the physiological consequence of atelectasis in the lungs?
What is the physiological consequence of atelectasis in the lungs?
A patient's arterial blood gas reveals an excessive amount of carbon dioxide in the bloodstream. Which condition does this indicate?
A patient's arterial blood gas reveals an excessive amount of carbon dioxide in the bloodstream. Which condition does this indicate?
In a patient experiencing hypoventilation, which of the following arterial blood gas imbalances is most likely to be observed?
In a patient experiencing hypoventilation, which of the following arterial blood gas imbalances is most likely to be observed?
What is the primary mechanism by which chemoreceptors in the medulla oblongata regulate respiration?
What is the primary mechanism by which chemoreceptors in the medulla oblongata regulate respiration?
Which statement accurately describes the process of diffusion in the context of oxygenation?
Which statement accurately describes the process of diffusion in the context of oxygenation?
What physiological factor has the most direct impact on the rate of diffusion in the lungs?
What physiological factor has the most direct impact on the rate of diffusion in the lungs?
Which of the following is a primary function of alveolar macrophages in the respiratory defense mechanism?
Which of the following is a primary function of alveolar macrophages in the respiratory defense mechanism?
During expiration, what change occurs in the intrapulmonary pressure relative to atmospheric pressure?
During expiration, what change occurs in the intrapulmonary pressure relative to atmospheric pressure?
In a healthy individual, which process is primarily responsible for the rhythmic control of respiration?
In a healthy individual, which process is primarily responsible for the rhythmic control of respiration?
Which of the following factors would most likely lead to a decreased oxygen-carrying capacity of the blood?
Which of the following factors would most likely lead to a decreased oxygen-carrying capacity of the blood?
A patient who has suffered a cervical spine injury at C4 is most at risk for:
A patient who has suffered a cervical spine injury at C4 is most at risk for:
How does cigarette smoking in adolescents primarily affect their respiratory health?
How does cigarette smoking in adolescents primarily affect their respiratory health?
How does regular exercise impact the efficiency of oxygen transport and utilization in the body?
How does regular exercise impact the efficiency of oxygen transport and utilization in the body?
Exposure to which of the following environmental factors is most associated with an increased risk of respiratory illnesses in children?
Exposure to which of the following environmental factors is most associated with an increased risk of respiratory illnesses in children?
A patient reports knifelike chest pain that worsens with inspiration. What type of pain should the nurse suspect?
A patient reports knifelike chest pain that worsens with inspiration. What type of pain should the nurse suspect?
Which assessment finding is indicative of dyspnea?
Which assessment finding is indicative of dyspnea?
What is suggested by hemoptysis with alkaline pH during a cough assessment?
What is suggested by hemoptysis with alkaline pH during a cough assessment?
Which of the following conditions is most likely indicated by the presence of nail clubbing?
Which of the following conditions is most likely indicated by the presence of nail clubbing?
During a physical examination, what does the finding of 'retractions' during chest wall movement indicate?
During a physical examination, what does the finding of 'retractions' during chest wall movement indicate?
Which breathing pattern is characterized by periods of apnea followed by deep breathing, often associated with neurological conditions?
Which breathing pattern is characterized by periods of apnea followed by deep breathing, often associated with neurological conditions?
Risk for aspiration would classify as which nursing diagnosis?:
Risk for aspiration would classify as which nursing diagnosis?:
When planning care for a patient with ineffective airway clearance, what is a realistic timeframe for pulmonary secretions to return to baseline with intervention?
When planning care for a patient with ineffective airway clearance, what is a realistic timeframe for pulmonary secretions to return to baseline with intervention?
What is the primary rationale for humidification when administering oxygen therapy at flow rates greater than 4 L/min?
What is the primary rationale for humidification when administering oxygen therapy at flow rates greater than 4 L/min?
The purpose of nebulization in respiratory care is to do what?
The purpose of nebulization in respiratory care is to do what?
In managing a post-operative patient's airway, what is the primary reason for encouraging coughing and deep breathing exercises?
In managing a post-operative patient's airway, what is the primary reason for encouraging coughing and deep breathing exercises?
What is the primary goal of postural drainage as a component of chest physiotherapy?
What is the primary goal of postural drainage as a component of chest physiotherapy?
In what order should the nurse suction the patient's airway?
In what order should the nurse suction the patient's airway?
When is an oral airway contraindicated?
When is an oral airway contraindicated?
One goal of incentive spirometry is:
One goal of incentive spirometry is:
What is the primary purpose of supplemental oxygen therapy?
What is the primary purpose of supplemental oxygen therapy?
Why is it important to monitor the skin around the ears and nostrils of a patient using a nasal cannula?
Why is it important to monitor the skin around the ears and nostrils of a patient using a nasal cannula?
Why is it dangerous to administer oxygen via simple face mask at less than 5L/min?
Why is it dangerous to administer oxygen via simple face mask at less than 5L/min?
Which of the following is a key characteristic of a non-rebreather oxygen mask?
Which of the following is a key characteristic of a non-rebreather oxygen mask?
Which oxygen delivery system is most appropriate for delivering a precise concentration of oxygen to a patient?
Which oxygen delivery system is most appropriate for delivering a precise concentration of oxygen to a patient?
Which of the following is likely to be listed in the patient's history if they have COPD?
Which of the following is likely to be listed in the patient's history if they have COPD?
A patient with COPD is at risk for what?
A patient with COPD is at risk for what?
Which of the following is one of the purposes for oxygen saturation when stable at >90% during rest?
Which of the following is one of the purposes for oxygen saturation when stable at >90% during rest?
A nurse is caring for a patient whose temperature is 101.5 F. What does the nurse expect this patient to experience?
A nurse is caring for a patient whose temperature is 101.5 F. What does the nurse expect this patient to experience?
What assessment finding is the earliest sign of hypoxia?
What assessment finding is the earliest sign of hypoxia?
The nurse needs to closely monitor the oxygen status of an elderly patient undergoing anesthesia because of which age-related change?
The nurse needs to closely monitor the oxygen status of an elderly patient undergoing anesthesia because of which age-related change?
Which nursing intervention is most effective in preventing hospital acquired pneumonia in an elderly patient?
Which nursing intervention is most effective in preventing hospital acquired pneumonia in an elderly patient?
Flashcards
Upper Respiratory Tract
Upper Respiratory Tract
The nose, mouth, pharynx, epiglottis, larynx, and trachea.
Lower Respiratory Tract
Lower Respiratory Tract
The bronchi, bronchioles, alveolar ducts, alveoli, and lung lobes.
Ventilation
Ventilation
The process of moving gases into and out of the lungs.
Diffusion
Diffusion
Signup and view all the flashcards
Perfusion
Perfusion
Signup and view all the flashcards
Work of breathing
Work of breathing
Signup and view all the flashcards
Surfactant
Surfactant
Signup and view all the flashcards
Atelectasis
Atelectasis
Signup and view all the flashcards
Hypoxia
Hypoxia
Signup and view all the flashcards
Hypercapnia
Hypercapnia
Signup and view all the flashcards
Hyperventilation
Hyperventilation
Signup and view all the flashcards
Hypoventilation
Hypoventilation
Signup and view all the flashcards
Cyanosis
Cyanosis
Signup and view all the flashcards
Chest physiotherapy
Chest physiotherapy
Signup and view all the flashcards
Nebulization
Nebulization
Signup and view all the flashcards
Nasal Cannula
Nasal Cannula
Signup and view all the flashcards
Simple face mask
Simple face mask
Signup and view all the flashcards
Non-rebreather mask
Non-rebreather mask
Signup and view all the flashcards
Venturi mask
Venturi mask
Signup and view all the flashcards
Asthma
Asthma
Signup and view all the flashcards
COPD
COPD
Signup and view all the flashcards
Oxygen therapy
Oxygen therapy
Signup and view all the flashcards
Cough, turn, deep breathe
Cough, turn, deep breathe
Signup and view all the flashcards
Study Notes
Respiratory Physiology
- Intercostal muscles are located in between ribs
- The lung is surrounded by a pleural sac, which has parietal pleura and visceral pleura
- The diaphragm is positioned at the bottom of lungs
Upper Respiratory Tract
- The upper respiratory tract includes the nose, mouth, pharynx, epiglottis, larynx, and trachea
Lower Respiratory Tract
- The lower respiratory tract includes the bronchi, bronchioles, alveolar ducts, and alveoli
- Lung lobes are also part of lower respiratory tract
Conducting Airways
- The trachea leads to the following:
- Bronchi
- Segmental bronchi
- Sub-segmental bronchi
- Bronchioles
- Alveolar ducts
- Alveoli
- Generations:
- Trachea- 0
- Bronchi - 8
- Segmental bronchi- 15
- Subsegmental bronchi - 21-22
- Alveolar Ducts - 24
- Alveoli - 28
Mechanism of Respiration - Inspiration
- The diaphragm descends and intercostal muscles contract, causing ribcage expansion
- Thoracic cavity volume increases, intrapulmonary volume increases causing decreased intrapulmonary pressure
- Air will enter nose/mouth
Mechanism of Respiration - Expiration
- Diaphragm rises and intercostal muscles will relax causing rib cages to descend.
- Thoracic cavity volume decreases leading to decreased intrapulmonary volume, causing increased intrapulmonary pressure
- Gas will flow out the lungs
Regulation of Respiration - Neural Regulation
- The central nervous system controls the respiratory rate, and rhythm
- The cerebral cortex regulates the voluntary control of respiration
Regulation of Respiration - Chemical Regulation
- The rate and depth of respirations are based on changes in the blood concentrations of CO₂ and O₂, and in hydrogen ion concentration (pH)
- Chemoreceptors in the medulla, aortic body and carotid body sense changes in the chemical content and stimulate neural regulators to adjust
Steps in Oxygenation
- Ventilation refers to the process of moving gases into and out of the lungs
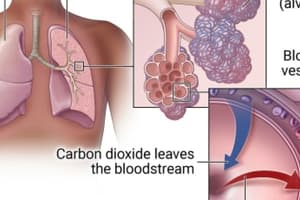
- Diffusion is the exchange of respiratory gases in the alveoli and capillaries
- Perfusion is the ability of the cardiovascular system to pump oxygenated blood to the tissues and return deoxygenated blood to the lungs
Respiratory Gas Exchange
- The thickness of the alveolar capillary membrane affects the rate of diffusion
- Oxygen transport is the combination of Lungs + cardiovascular (CV) system
- Hemoglobin carries O₂ and CO2
- Carbon dioxide transport
Respiratory Defense Mechanism
- Respiratory defense mechanisms include:
- Filtration of air
- Mucociliary clearance system
- Cough reflex
- Reflex bronchoconstriction
- Alveolar macrophages
Terminology
- Work of breathing is the effort required to expand and contract the lungs: inspiration and expiration
- Surfactant is a chemical produced in the lungs to maintain the surface tension of the alveoli and keep them from collapsing
- Atelectasis refers to a collapse of the alveoli that prevents normal exchange of oxygen and carbon dioxide
- Hypoxia refers to inadequate tissue oxygenation at the cellular level.
- It is life threatening and if left untreated can lead to fatal cardiac dysrhythmias.
- The earliest sign is restlessness and changes in level of consciousness
- Hypercapnia is excessive CO2 in the bloodstream
- Hyperventilation is inadequate alveolar ventilation to meet the oxygen demand of the body or eliminate sufficient CO2
- Decreased CO2 means blood is more alkaline
- Hypoventilation is a state of ventilation in which the lungs remove CO2 faster than it is produced by cellular metabolism
- Increased CO2 means blood is more acidic
- Cyanosis involves Blue discoloration of the skin and mucous membranes caused by decreased hemoglobin in capillaries
- A late sign of hypoxia; observed in tongue, soft palate, and conjunctiva of the eye
Cardiovascular Physiology
- Myocardial pump includes two atria and two ventricles
- When the myocardium stretches, the strength of the subsequent contraction increases (Starling's law)
- Coronary artery circulation involves the coronary arteries supplying the myocardium with nutrients and remove wastes
- Myocardial blood flow is unidirectional through four valves
- S1: mitral and tricuspid close
- S2: aortic and pulmonic valves close
- Systemic circulation involves the arteries and veins delivering nutrients and oxygen and remove waste products
Critical Lab Values
- PaO2 values are:
- ≥70%: SpO2 ≥94% Significance: Adequate unless hemodynamically unstable or has difficulty releasing O₂ to the tissues
- 60%: SpO2 90% Significance: Adequate in almost all patients but with less error margin
- 55%: SpO2 88% Significance: Adequate with chronic hypoxemia, if no cardiac event
- 40%: SpO2 75% Significance: Inadequate but maybe acceptable short term basis (CO2 retention)
- <40%: SpO2 <75% Significance: Inadequate, tissue hypoxia and cardiac dysrhythmias is possible.
Blood Gas Normal Values - Arterial Blood Gases
- Assumes patient is ≤60 years of age and breathing room air.
- Values decrease with age.
- The same normal values when SpO2 are obtained by oximetry.
- Normal values at sea level:
- pH: 7.35-7.45
- PaO2: 80-100 mm Hg
- SaO2: >95%
- PaCO2: 35-45 mm Hg
- HCO3-: 22-26 mEq/L (mmol/L)
Blood Gas Normal Values - Venous Blood Gases
- Assumes patient is ≤60 years of age and breathing room air.
- Values decrease with age.
- The same normal values when SvO2 are obtained by oximetry.
- Normal values at sea level:
- pH: 7.32-7.43
- PvO2: 38-42 mm Hg
- SvO2: 60%-80%+
- PVCO2: 38-55 mm Hg
- HCO3-: 22-26 mEq/L (mmol/L)
Factors Affecting Oxygenation
- Physiological
- Developmental
- Lifestyle
- Environmental
Physiological Factors
- Any disorder that affects the body to meet oxygen demands affects oxygenation
- Respiratory and cardiac disorders
- Conduction disturbances such as dysrhythmias affecting oxygenation:
- stenosis
- regurgitation
- myocardial ischemia ( angina pectoris and myocardial infarction)
- altered cardiac output (heart failure (left or right))
- Conduction disturbances such as dysrhythmias affecting oxygenation:
- Decreased oxygen-carrying capacity:
- Anemia
- Carbon monoxide poisoning (CO)
- Hypovolemia:
- Shock and severe dehydration leads to extracellular fluid loss and reduced circulating blood volume leading to hypoxia which affects oxygenation.
- Decreased inspired oxygen concentration (FiO2)
- High altitude, hypoventilation (drug overdose) affects oxygenation
More Physiological Factors
- Increased metabolic rates affects oxygenation
- Seen in pregnancy, wound healing, exercise, and fever.
- Conditions reducing chest wall movement affects oxygenation
- Seen in pregnancy and obesity
- Musculoskeletal abnormalities affects oxygenation
- Includes flail chest and cerebral palsy
- Neuromuscular Disease
- Guillain-Barre syndrome, myasthenia gravis, and poliomyelitis
- Central Nervous System
- Disease or trauma to medulla oblongata
- Cervical trauma to C3-C5 causes phrenic nerve damage (controls diaphragm movement)
Developmental Factors
- Infants and toddlers
- Immature immune system, frequent upper respiratory infections
- School-age children and adolescents
- Frequent upper respiratory infections
- Risk for cigarette smoking in adolescents
- Young and middle adults
- Cardiopulmonary risk factors such as unhealthy diets, lack of exercise, stress, smoking, illegal substances
- Older adults
- Risk for respiratory infections
- Decreased elastic recoil of lungs and stiffening of chest walls lead to more rounded and smaller lungs.
- Physiological changes through calcification of heart valves, SA nodes, and costal cartilages and atherosclerotic plaques. -Alveoli enlarget which decreases surface area for gas exchange
- Decreased functional cilia – which decreases cough mechanism
Lifestyle Factors
- Nutrition
- Obesity decreases lung expansion and increase tissue oxygen demands
- Malnourishment causes respiratory muscle wasting and decreased respiratory excursion
- Anemia occurs
- Exercise
- Increases efficiency of myocardial muscle
- Recommended for 30-60 minutes per day
- Smoking
- Nicotine causes vasoconstriction worsening peripheral vascular and coronary artery disease
- COPD
- Substance Abuse
- Alcohol depresses the respiratory center
- Inhalants cause direct lung damage
- Stress
- Body will respond with increase metabolic rate and oxygen demand
Environmental Factors
- Urban areas -Pollution
- Occupational pollutants -Asbestos, talcum powder, dust and airborne fibers
- Tobacco smoke causes a -Higher incidence of pneumonia, ear infections and asthma in children
Nursing Assesment - History
- Chest pain
- Angina Pectoris requires immediate thorough evaluations; also evaluate location, duration, radiation, and frequency of issues
- Men present with left side of chest with radiation to left arm
- Women present with less definitive symptoms: nausea, fatigue, breathlessness
- Pleuritic chest pain involves inflammation or infection of the pleural space, worsening with inspiration; knifelike lasting from minutes to hours
- Musculoskeletal pain is caused by costochondritis (from prolonged coughing episodes) or exercise; pain worsens with inspiration
- Angina Pectoris requires immediate thorough evaluations; also evaluate location, duration, radiation, and frequency of issues
- Fatigue is a subjective loss of endurance that may be an early sign of worsening chronic disease.
- Ask patients to rate on scale 0-10
- Dyspnea: difficult or uncomfortable breathing that is a Clinical sign of hypoxia that can occur with exertion, stress or respiratory infections
- Orthopnea is identified by the number of pillows needed to comfortable breathe
- Can present with the use of accessory muscles, nasal flaring or marked increased in rate and depth of respiration
- Ask patient to rate on scale 0-10
- Cough
- Productive or nonproductive sputum; note the color, blood-tinged, consistency, odor, and amount
- Hemoptysis involves bloody sputum with alkaline pH
- Hematemesis occurs in the Gl tract and has acidic pH
- When does the cough occur? note specific times of day.
- Coughing early morning or when rising may be caused by GERD or sinusitis
- Wheezing is a High pitched musical sound from narrowed airway
- Can be caused by asthma, acute bronchitis, or pneumonia
- Occurs inspiration, expiration or both -Determine if there are any precipitating factors: URI, allergens, exercise or stress
- Environmental or Geographical Exposures:
- Carbon monoxide (CO), Smoke, Occupational
- Smoking -Direct or indirect exposure to tobacco -Pack-year history (packages per day x years)
- Repiratory infections
- Frequency and duration of respiratory tract infection
- Average: 4 per year
- Vaccinations: pneumococcal, influenza
- HIV infection: opportunistic infections (P. carinii pneumonia)
Rest of Nursing Assessment - History
- Alleries
- Health Risks -History of lung cancer or cardiovascular disease
- TB exposure
- Medications
Physical Examination - Inspection
- Note Level of Consciousness
- Chest wall movement should be examined for retractions (sinking in of soft tissues of chest between intercostal space) and Accessory muscles
- Breathing pattern can take the form of Apnea, Paradoxical breathing (chest wall contracts during inspiration and expands during exhalation), Kussmaul respiration (metabolic acidosis), and Cheyne-Stokes respirations (periods of apnea with deep breathing)
- Patients in distress may take on a Tripod position
- Respirations should be observed a normal adult (12 to 20 regular breaths/min)
- Nail clubbing indicates prolonged oxygen deficiency, endocarditis, and congenital heart defects.
Physical Exam - Palpation
- Involves Thoracic excursion
- Should be examined for Fremitus, Thrills, Heaves
- Cardiac point of maximal impulse (PMI)
- Examine Peripheral Extremities for Capillary refills (<2-3 seconds), Peripheral pulses, and Skin temperature and color
Physical Exam - Auscultation
- Auscultate for Adventitious lung sounds and abnormal heart sounds (S3, S4, murmurs)
Nursing Diagnosis and Planning
- Activity intolerance, decreased cardiac output, and fatigue can lead to: -Impaired gas exchange, impaired spontaneous ventilation, or impaired verbal communication
- The following have the potential to cause ineffective airway clearance, ineffective breathing pattern, or ineffective health maintenance: -Risk for aspiration, risk for infection, risk for suffocation
- Risk for imbalanced fluid volume
Goals
- Focus on Ineffective airway clearance related to pulmonary secretions -Pulmonary secretions will return to baseline levels within 24 to 36 hours.
- Patient's oxygenation status will improve in 36 hours.
Implementation: Health Promotion
- Involve Vaccinations: Influenza and pneumococcal
- Practice a Healthy lifestyle by eliminating risk factors and eating right and doing regular exercise.
- Avoid Environmental pollutants, secondhand smoke, work chemicals, and pollutants
Acute Care Implementation
- Administer Pharmacological agents such as Bronchodilators, inhaled steroids, mucolytic, and low dose anti-anxiety medications
- Oxygen therapy protocols
- Use Physical techniques -Breathing techniques, Cough control, Relaxation techniques
Airway Management
- Maintain free Trachea, bronchi, and large airways from obstruction
- Involve Mobilization of pulmonary secretions and Maintian clear airways by coughing or suctioning Decreases recovery time and complications
- Provide Hydration to maintain thin easily removable secretions
- Maintain 1500-2500 ml/day unless contraindicated
- Use Humidification to make procedure necessary if patient is receiving oxygen (>4 L/min)
- Use Nebulization with moisture and medication to inspired air by mixing particles of varying size to the air
- Enhances mucociliary clearance for removal of mucus and cellular debris
Airway Management Techniques
- Coughing and Deep breathing postoperative after Q 2 hours while awake to prevent accumulation of secretions
- Cascade cough, Huff Cough, and Quad cough
- Acute phase of mucus production involves Deep breathing Q 2 hours while awake, Cough Q 1 hour while awake, and Cough Q 2 - 3 hours at night time
- Deep inhalation increases lung volume and airway diameter Allows air to move and pass through partially obstructed mucus plugs or foreign matter
- Chest physiotherapy (CPT)
- Postural drainage, chest percussion and vibration
- Is followed by coughing or suctioning of a patient who has the decreased ability to cough
- Recommended for patients with mucus production > 30 mL/day
Airway Management Techniques - Suctioning
-Use Sterile technique with oropharynx and trachea and suction oral secretions last
- Oropharyngeal and nasopharyngeal:
- Used when the patient can cough effectively but is not able to clear secretions
- Orotracheal and nasotracheal: -Used when the patient is unable to manage secretions
- Tracheal suctions are used with an artificial airway
Airways
- Oral airway prevents obstruction of the trachea by displacement of the tongue into the oropharynx
- Endotracheal and tracheal airways are for short-term use to ventilate, relieve upper airway obstruction, protect against aspiration, and clear secretions
- Tracheostomy is a long-term assistance where surgical incision is made into trachea
Maintenance and Promotion of Lung Expansion
- Encourages Ambulation, Positioning (reduces pulmonary stasis and maintains ventilation and oxygenation), and Incentive spirometry (encourages voluntary deep breathing)
- Utilize Noninvasive ventilation to maintain positive airway pressure and improves alveolar ventilation
The Process of Using Incentive Spirometry
- Hold the spirometer upright
- Place the mouth piece in mouth and seal lips tightly
- Breathe slowly as deeply as possible
- Notice yellow piston rises to top of column, yellow indicator reaches blue outlined area
- Hold breath as long as possible, then slowly exhale allowing piston to fall to the bottom of the column
- Rest for a few seconds and repeat 1-5 10 times every hour
- Postion the yellow indicator on the left side of spirometer to show your best efforts, use indicator as a goal during each slow deep breath
- After each set of 10 deep breaths, cough to be sure lungs are clear.
- If you have incision, support your incision when coughing placing pillow firmly agaisnt
- Once you are able to get out of bed safely, take frequent walks and practice the cough
Maintenance and Promotion of Oxygenation
- Involves Oxygen therapy to prevent or relieve hypoxia
- Implement Safety precautions
- Supply oxygen throguh Tanks or wall-piped system
- Delivery occurs through -Nasal cannula -Oxygen mask
Delivery of Oxygen
- Nasal Cannulas can use a flow rate up to 6 L/min at a FIO2 range of 24-40% oxygen
- Flow rates >4 L/min must need humidifier
- Be aware of skin breakdown over ears and nostrils from cannula and tight application
- Oxygen Masks: Simple Face Mask is a short-term oxygen source -Has a Flow rate of 6 to 10 L/min -Levels below 5 L/min will cause rebreathing of CO2 -FIO2 ranges from 40-60% -Contraindicated for patients with conditions with CO2 retention such as COPD
- Oxygen Masks: Non-Rebreather has a flow rate of 10 L minimum
- FIO2 range is 60-80%.
- Valve between the bag and mask prevents exhaled air from returning into bag, this reduces rebreathing
- Bag should at least 1/3 to 1/2 full on inspiration -Deflated bag = breathing in large amount of exhaled CO2
- Oxygen Masks: Venturi masks have
- a Flow rate of 4 to 12 L/min depending on flow meter selected
- FIO2 range of 24-60%
Common Respiratory Diseases - Atelectasis and Asthma
- Atelectasis: Collapse of full or partial lung (alveoli)
- Most common cause from postsurgical procedures
- Encourage deep breathing and incentive spirometer usage
- Asthma involves a chronic inflammatory disorder of airways
- Leads to reversible episodes of wheezing, breathlessness, chest tightness and cough
- Triggered by allergies, exercise, cigarette smoking, and GERD
Common Respiratory Diseases - COPD
- Chronic Obstructive Pulmonary Disease (COPD) is generally progressive -Has irreversible airflow limitations during forced exhalation due to loss of elastic recoil with an airflow is obstructed by mucous hypersecretion, mucosal edema, and bronchospasm
- Its Risk factors are cigarette smoking, Age >40 years, >10 years of smoking, and occupational chemical and dust, and air pollution.
- COPD has two types involving chronic bronchitis and emphysema
- Oxygen therapy includes:
- a treatment to maintain Oxygen saturation >90% during rest, exercise and sleep.
- PaO2 greater than 60 mmHg
- Increasing O2 saturation may lead to increased levels of CO2 and worsening outcomes
- Treatments involve Antibiotics or other therapies to Increase exercise capacity and Improve overall survival
Questions
- Patients with a temperature of 101.5 F have rapid breathing owing to increased metabolic demands
- The earliest sign of hypoxia is restlessness
- Nurses need to closely monitor the oxygen status of an elderly patient undergoing anesthesia because decreased lung defense mechanisms may cause ineffective airway clearance
- Assist patient to cough, turn, and deep breathe every 2 hours to prevent hospital acquired pneumonia in an elderly patient
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.