Podcast
Questions and Answers
How does the regulation of pH occur within the respiratory system?
How does the regulation of pH occur within the respiratory system?
- By controlling the levels of sodium
- By adjusting the levels of bicarbonate
- By directly affecting the concentration of hydrochloric acid
- By releasing or retaining CO2 (correct)
What distinguishes external respiration from cellular respiration?
What distinguishes external respiration from cellular respiration?
- External respiration produces ATP, while cellular respiration consumes ATP.
- External respiration occurs in the mitochondria, while cellular respiration occurs in the cytoplasm.
- External respiration includes the breakdown of organic molecules, while cellular respiration involves gas exchange with the environment.
- External respiration involves gas exchange between cells and the environment, and cellular respiration involves intracellular reactions with oxygen. (correct)
How does the structure of the lower respiratory tract facilitate its function?
How does the structure of the lower respiratory tract facilitate its function?
- The unchanging diameter of the bronchi ensures consistent air velocity.
- The presence of cartilage in bronchioles allows for greater gas exchange.
- The decreasing amount of cartilage and increased smooth muscle allows for regulated airflow. (correct)
- The rigid structure of the trachea ensures maximum airflow during inhalation.
What is the functional consequence of sympathetic activation on the bronchioles?
What is the functional consequence of sympathetic activation on the bronchioles?
What is the primary functional difference between Type I and Type II alveolar cells?
What is the primary functional difference between Type I and Type II alveolar cells?
How does the relatively low pressure in the pulmonary circulation affect its function?
How does the relatively low pressure in the pulmonary circulation affect its function?
What is the relationship between volume and pressure as described by Boyle's Law, and how does this apply to respiration?
What is the relationship between volume and pressure as described by Boyle's Law, and how does this apply to respiration?
How does the maintenance of a negative intrapleural pressure contribute to normal respiratory function?
How does the maintenance of a negative intrapleural pressure contribute to normal respiratory function?
During inspiration, what directly causes air to enter the lungs?
During inspiration, what directly causes air to enter the lungs?
How does the elastic recoil of the lungs and the thoracic wall interact during normal breathing?
How does the elastic recoil of the lungs and the thoracic wall interact during normal breathing?
What would happen if the pressure in the intrapleural cavity equalized with the intrapulmonary pressure?
What would happen if the pressure in the intrapleural cavity equalized with the intrapulmonary pressure?
During expiration, what sequence of events leads to air moving out of the lungs?
During expiration, what sequence of events leads to air moving out of the lungs?
Which of the following components is not considered part of 'Work of Breathing'?
Which of the following components is not considered part of 'Work of Breathing'?
How is compliance of the lungs defined, and what factors affect it?
How is compliance of the lungs defined, and what factors affect it?
What is the functional significance of the lung's elastance?
What is the functional significance of the lung's elastance?
How does surfactant reduce surface tension in the alveoli, and why is this important for lung function?
How does surfactant reduce surface tension in the alveoli, and why is this important for lung function?
According to the Law of LaPlace, if two alveoli have different radii but the same surface tension, how does the pressure differ between them, and what prevents smaller alveoli from collapsing?
According to the Law of LaPlace, if two alveoli have different radii but the same surface tension, how does the pressure differ between them, and what prevents smaller alveoli from collapsing?
When would compliance be lowest?
When would compliance be lowest?
In what situations would compliance work increase?
In what situations would compliance work increase?
How would you define resistance?
How would you define resistance?
What is the result of restrictive disease?
What is the result of restrictive disease?
How does the respiratory system facilitate vocalization, one of its primary functions?
How does the respiratory system facilitate vocalization, one of its primary functions?
What structural feature of the trachea prevents its collapse during ventilation?
What structural feature of the trachea prevents its collapse during ventilation?
How do the intercostal muscles contribute to the mechanics of breathing?
How do the intercostal muscles contribute to the mechanics of breathing?
What is the role of pleural fluid in respiratory mechanics?
What is the role of pleural fluid in respiratory mechanics?
How does the mucociliary transport system protect the respiratory system?
How does the mucociliary transport system protect the respiratory system?
What would be the effect of destruction of cilia within the respiratory tract?
What would be the effect of destruction of cilia within the respiratory tract?
How does the branching structure of the bronchial tree contribute to efficient gas exchange?
How does the branching structure of the bronchial tree contribute to efficient gas exchange?
What is the primary function of hyaline cartilage in the trachea and larger bronchi?
What is the primary function of hyaline cartilage in the trachea and larger bronchi?
How does the sympathetic nervous system affect airway diameter and resistance, and through what mechanism?
How does the sympathetic nervous system affect airway diameter and resistance, and through what mechanism?
What structural changes occur in the respiratory tract as the airways branch from bronchi to bronchioles, and how do these changes affect airway function?
What structural changes occur in the respiratory tract as the airways branch from bronchi to bronchioles, and how do these changes affect airway function?
What are the key steps in the process of external respiration?
What are the key steps in the process of external respiration?
How does the total cross-sectional area of the pulmonary capillaries affect gas exchange efficiency?
How does the total cross-sectional area of the pulmonary capillaries affect gas exchange efficiency?
In the context of gas laws, how does Dalton's Law relate to the partial pressure of oxygen in the atmosphere?
In the context of gas laws, how does Dalton's Law relate to the partial pressure of oxygen in the atmosphere?
How does the concentration of surfactant in smaller alveoli contribute to alveolar stability, according to the Law of Laplace.
How does the concentration of surfactant in smaller alveoli contribute to alveolar stability, according to the Law of Laplace.
What is the relationship between airway resistance and airway diameter, and how is this relevant in conditions like asthma or COPD?
What is the relationship between airway resistance and airway diameter, and how is this relevant in conditions like asthma or COPD?
How would restrictive lung disease impact compliance?
How would restrictive lung disease impact compliance?
How does increased mucus production in the lower respiratory tract specifically affect airway resistance and the work of breathing?
How does increased mucus production in the lower respiratory tract specifically affect airway resistance and the work of breathing?
How would a pulmonary embolism that obstructs a major pulmonary artery affect alveolar ventilation and the partial pressure of carbon dioxide (PaCO2) in the affected region?
How would a pulmonary embolism that obstructs a major pulmonary artery affect alveolar ventilation and the partial pressure of carbon dioxide (PaCO2) in the affected region?
Which of the following scenarios would most likely result in a decrease in lung compliance?
Which of the following scenarios would most likely result in a decrease in lung compliance?
How does the respiratory system adapt to maintain efficient gas exchange during strenuous exercise, considering both ventilation and perfusion?
How does the respiratory system adapt to maintain efficient gas exchange during strenuous exercise, considering both ventilation and perfusion?
In a patient with severe emphysema, which of the following compensatory mechanisms is least likely to be effective in maintaining adequate arterial oxygen levels?
In a patient with severe emphysema, which of the following compensatory mechanisms is least likely to be effective in maintaining adequate arterial oxygen levels?
How does the structure of the alveolar-capillary interface optimize gas exchange, and what pathological changes would most significantly impair this process?
How does the structure of the alveolar-capillary interface optimize gas exchange, and what pathological changes would most significantly impair this process?
What is the consequence of equalizing intrapleural pressure with atmospheric pressure, and what condition might cause this equalization?
What is the consequence of equalizing intrapleural pressure with atmospheric pressure, and what condition might cause this equalization?
How does the parasympathetic nervous system influence airway diameter, and what receptor type mediates this effect?
How does the parasympathetic nervous system influence airway diameter, and what receptor type mediates this effect?
In the context of Dalton's Law, if the atmospheric pressure decreases (e.g., at high altitude), what happens to the partial pressure of oxygen (PO2), and how does this affect oxygen delivery to the tissues?
In the context of Dalton's Law, if the atmospheric pressure decreases (e.g., at high altitude), what happens to the partial pressure of oxygen (PO2), and how does this affect oxygen delivery to the tissues?
What is the functional role of the mucociliary escalator, and how does its impairment contribute to respiratory disease?
What is the functional role of the mucociliary escalator, and how does its impairment contribute to respiratory disease?
During exercise, the increase in ventilation is disproportionately greater than the increase in carbon dioxide production. What effect does this have on alveolar and arterial partial pressures of carbon dioxide?
During exercise, the increase in ventilation is disproportionately greater than the increase in carbon dioxide production. What effect does this have on alveolar and arterial partial pressures of carbon dioxide?
How does surfactant work to stabilize alveoli of different sizes, preventing collapse of smaller alveoli, and what law explains this phenomenon?
How does surfactant work to stabilize alveoli of different sizes, preventing collapse of smaller alveoli, and what law explains this phenomenon?
What is the primary mechanism by which the body responds to chronically elevated arterial carbon dioxide levels (PaCO2), and what are the potential long-term consequences of this adaptation?
What is the primary mechanism by which the body responds to chronically elevated arterial carbon dioxide levels (PaCO2), and what are the potential long-term consequences of this adaptation?
What is the interdependence of alveolar function, and how does the loss of elastic tissue in emphysema affect this interdependence?
What is the interdependence of alveolar function, and how does the loss of elastic tissue in emphysema affect this interdependence?
How does the pulmonary circulation's relatively low pressure affect fluid dynamics in the lungs, and what implications does this have for the formation of pulmonary edema?
How does the pulmonary circulation's relatively low pressure affect fluid dynamics in the lungs, and what implications does this have for the formation of pulmonary edema?
Flashcards
Respiratory System: Primary Functions?
Respiratory System: Primary Functions?
Exchange of gases, pH regulation, protection from pathogens, and vocalization.
External Respiration
External Respiration
The movement of gases between cells and environment.
What are airways?
What are airways?
The system of tubes and airways for air passage.
What are Alveoli?
What are Alveoli?
Signup and view all the flashcards
Lungs
Lungs
Signup and view all the flashcards
Hyaline cartilage
Hyaline cartilage
Signup and view all the flashcards
Pseudostratified columnar epithelium
Pseudostratified columnar epithelium
Signup and view all the flashcards
Bronchoconstriction
Bronchoconstriction
Signup and view all the flashcards
Bronchodilation
Bronchodilation
Signup and view all the flashcards
Type 1 Pneumocytes
Type 1 Pneumocytes
Signup and view all the flashcards
Pulmonary Circulation
Pulmonary Circulation
Signup and view all the flashcards
Air Flow Pressure
Air Flow Pressure
Signup and view all the flashcards
What is P_atm?
What is P_atm?
Signup and view all the flashcards
P_pl
P_pl
Signup and view all the flashcards
P_pul
P_pul
Signup and view all the flashcards
Opposing forces
Opposing forces
Signup and view all the flashcards
What is Ventilation?
What is Ventilation?
Signup and view all the flashcards
Airway resistance work
Airway resistance work
Signup and view all the flashcards
Compliance work
Compliance work
Signup and view all the flashcards
Compliance
Compliance
Signup and view all the flashcards
Elastance
Elastance
Signup and view all the flashcards
Elastic forces of lung
Elastic forces of lung
Signup and view all the flashcards
Elastic forces of lung
Elastic forces of lung
Signup and view all the flashcards
What is Surfactant?
What is Surfactant?
Signup and view all the flashcards
LaPlace's Law
LaPlace's Law
Signup and view all the flashcards
Resistive work
Resistive work
Signup and view all the flashcards
Obstructive disease
Obstructive disease
Signup and view all the flashcards
Restrictive disease
Restrictive disease
Signup and view all the flashcards
Study Notes
- Respiratory physiology includes the anatomy, mechanics of breathing, and compliance of the respiratory system.
Respiratory System: Primary Functions
- Exchange of gases between the atmosphere and the blood occurs.
- Regulation of pH is achieved by releasing or retaining CO2.
- Protection from inhaled pathogens
- Vocalization
Cellular vs. External Respiration
- Cellular respiration is the intracellular reaction of O₂ with organic molecules to produce CO2 and ATP.
- External respiration involves the movement of gases between cells and the environment.
- The four processes of external respiration are:
- Ventilation between the atmosphere and air sacs (alveoli) in the lungs.
- Exchange of O₂ and CO2 between air in the alveoli and blood in the pulmonary capillaries.
- Transport of O₂ and CO2 by the blood between the lungs and tissues.
- Exchange of O₂ and CO2 between the blood in systemic capillaries and tissue cells.
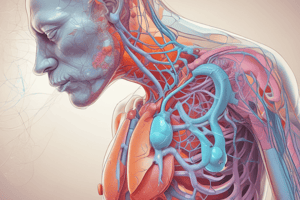
General Anatomy
- The respiratory system is divided into the upper and lower respiratory tracts.
- The upper respiratory tract consists of the mouth, nasal cavity, pharynx, and larynx.
- The lower respiratory tract includes the trachea, bronchioles, and branches.
Respiratory Functions
- Passageway for air
- Warms the air
- Adds water vapor to dry gas exchange surface
- Filters out foreign materials like dust and viruses
Lower Respiratory Tract functions
- Pull air in from upper respiratory tract
- Absorb oxygen
- Release carbon dioxide
- The three main components of the respiratory system are:
- Airways: system of tubes/airways
- Alveoli: structures for gas exchange
- Bones and Muscles of thorax and abdomen that assist in ventilation
Lungs and Thoracic Cage
- Lungs are spongy tissue with volume that is mostly air-filled spaces.
- Airways connect to the lungs via the trachea and bronchi.
- The thoracic cage consists of:
- Bones: ribs, sternum, and vertebrae
- Muscles: intercostals, sternocleidomastoid, and scalenes
Pleural Membranes
- The pleural membranes are a double-walled membranous sac that covers each lung.
- One side is attached to the lung, and the other is attached to the ribs and muscles.
- The inside of the pleural sac contains pleural fluid, which provides a moist, slippery surface for breathing.
- It ensures that the two layers stick together so that they slide over each other easily yet still stick to each other.
Lower Respiratory Tract: Trachea
- Structurally, the trachea is 12cm long and 2.5cm in diameter.
- Located anterior to the esophagus and has a unique structure.
- Responsible for air humidification, filtration, and warming.
- Contains Hyaline cartilage (C-shaped) and smooth muscle (m. trachealis).
- Contains Pseudostratified ciliated columnar epithelium (PSCC)
- PSCC components ensure mucus is produced, trapping pathogens.
- Smoking irritates and destroys cilia, impairing mucociliary transport.
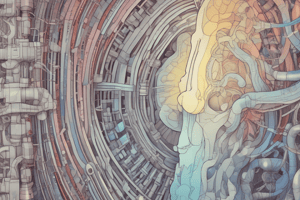
Lower Respiratory Tract: Bronchial Tree
- The bronchial tree is a series of tubes that carry air.
- Mainstem bronchi are left and right and separate distal to the trachea.
- Bronchi branch repeatedly about 22 times, becoming smaller, and the amount of cartilage decreases.
- Eventually replaced with more smooth muscle.
- Bronchi have some cartilage, while bronchioles have no cartilage.
- Divisions increase which makes smaller tubes.
- Nerves increase surface area maximizing the amount of gas exchange.
Control of Airflow
- Bronchoconstriction is the constriction of smooth muscle in bronchioles, which leads to a smaller radius and more resistance to airflow and is influenced by parasympathetic input through muscarinic receptors.
- Bronchodilation is the relaxation of smooth muscle in bronchioles, which leads to an increased radius and less resistance to airflow due to sympathetic activation of B₂ receptors by epinephrine/norepinephrine.
Lower Respiratory Tract: Respiratory Bronchiole
- Cartilage rings gradually decrease in size and number as branches divide, while the mucous membrane becomes thinner.
- The terminal bronchioles turn into respiratory bronchioles
- Respiratory bronchioles consist of smooth muscle, elastic tissue, and thin mucous membranes
- Further divide into alveolar ducts.
Lung Lobule
- A lung lobule contains alveoli and is the final destination of air.
- Primary function is gas exchange, done through a Single layer of cells line each alveolus
- Close association with capillary network, almost always continuous with sheet of blood in contact with air filled alveoli
- Very little room between alveoli for rapid diffusion
Internal Structure of Alveoli
- There are two types of cells:
- Type 1 Alveolar Cells: 95% of the surface and is very thin: facilitates diffusion of gases.
- Type II Alveolar Cells: Thicker cells that create surfactant, which removes excess fluid.
Pulmonary Circulation
- Pulmonary circulation has high flow and low pressure due to
- Shorter length of blood vessels in the pulmonary circuit
- Large total cross-sectional area of blood vessels
- Cardiac output is 5L/min, meaning that this value of blood is going through the lungs/minute.
Mechanics of Breathing
- Gas Laws
Gas Laws
- Air is similar to blood because both are fluids.
- Air is compressible
- These laws govern the properties of gases. - Ideal Gas Law and Boyle's Law: P₁V₁ = P₂V₂
- Both equations express the inverse relationship between volume and pressure.
Dalton's Law: Air is a Mixture of Gases
- The total pressure exerted by a mixture of gases is equal to the sum of the pressures exerted by each individual gas
- Partial pressure is the pressure exerted by an individual gas.
- Partial pressure of a gas = Patm x % of gas in atmosphere.
- Oxygen makes up 21% of air. Normal atmospheric pressure is 760 mmHg.
- Poxygen = 760 mmHg x 21% oxygen, Poxygen = 760 mmHg x 0.21 = 160 mmHg
Mechanics of Breathing
- Air flow occurs when a pressure gradient is present
- Flows from an area of high pressure to an area of low pressure.
- Diffusion of a single gas moves from areas of high partial pressure to areas of low partial pressure.
- The movement of air into the lungs is influenced by pressure gradients.
Pressure Relationships in the Thoracic Cavity
- Patm is the pressure of gases in the atmosphere, equal to 760mmHg or 1atm.
- Ppl is the pressure in the pleural cavity, approximately 756mmHg or -4mmHg.
- Ppul pressure is exerted by the alveoli in the lungs.
- Ppul must be greater than Ppl or lungs will collapse.
Basic Principles
- Air always travels from an area of high pressure to an area of low pressure.
- As volume increases, pressure decreases (Boyle's Law).
- Atmospheric pressure
- Intrapulmonary pressure and volume
- Intrathoracic pressure and volume
- Intrapleural pressure
Negative Pleural Pressure: Opposing Forces
- Influenced by the elastic recoil of lungs
- Thoracic wall is always trying to expand, while the pleura is pulled in opposite directions causing intraplerual space = negative pressure
- The Pleura is pushed to to thoracic wall
- Intrapleural space = negative pressure
- Pleural fluid contains water, creating a hydrostatic force btween the layers that makes the lungs and visceral pleura move with the thoracic wall
Before Inspiration
- No air moving and thoracic wall is stationary
- Patm= Pintrapulmonary
- Ppl = negative
Inspiration
- The diaphragm contracts and moves inferiorly.
- External intercostals contract and move the ribs up and out.
- Muscles cause extra force pulling the thoracic wall out which overcomes the elastic recoil force of the lungs
- Causes thoracic wall to expand
Inspiration: Greater Negative Pressure
- Increases the volume in the thoracic cavity
- The extra muscular force pulling on the pleura creates greater negative pleural pressure.
- Ensures the lungs stick to the moving thoracic wall and increases the volume of the lungs.
- Because the lungs have a lower pressure than the atmosphere, air rushes into the lungs (Patm > Pintrapulmonary).
Inspiration Sequence of Events
- Inspiratory muscles contract (diaphragm descends; rib cage rises).
- Thoracic cavity volume increases.
- Lungs are stretched, and intrapulmonary volume increases.
- Intrapulmonary pressure drops (to -1 mm Hg).
- Air (gases) flows into lungs down its pressure gradient until intrapulmonary pressure is 0 (equal to atmospheric pressure).
Intrapulmonary and Intraplural Pressures
- At rest, no net difference between Ppul and Patm
- During inspiration there is negative pressure
- During expiration there is positive pressure
Expiration Sequence of Events
- Inspiratory muscles relax (diaphragm rises; rib cage descends due to recoil of costal cartilages).
- Thoracic cavity volume decreases.
- Elastic lungs recoil passively; intrapulmonary volume decreases.
- Intrapulmonary pressure rises (to +1 mm Hg).
- Air (gases) flows out of lungs down its pressure gradient until intrapulmonary pressure is 0.
Work of Breathing
- Ventilation is the bulk flow of air from the atmosphere to the alveoli
- Respiratory cycle consists of inspiration followed by and expiration
- Work of breathing encompasses the required work to:
- Expand the lungs against elastic forces (compliance work).
- Overcome the viscosity of the lung and chest wall structures (tissue resistance work).
- Overcome airway resistance during the movement of air into the lung (airway resistance work).
Factors that affect ventilation
- Compliance: How easily the lungs can inflate
- Elastance: ability to resist being deformed
- Lungs must have a natural elastic fiber
Elastic Properties of the Lung
- Compliance = △Volume/△Pressure
- Forces:Elastic forces of the lung tissue
- Elastic forces caused by
- Fluid that lines the walls
Compliance
- Lowest at maximal inspiratory volumes Lowest at maximal inspiratory volumes
- Lower in children
- Highest in large lungs
Compliance Diagram of the Lung
- The differences in compliance between the air-filled and water-filled lung is a result of different surfaces
Surface tension
- LePlace's Law: States that the pressure inside of a bubble formed by thin fluid is a function of:
- Surface tension/ Radius of the bubble
Surface Tension
- Surface tension is the ratio of pressure:P = 2T/r (where P = pressure, T = surface tension, r = radius).
- The smaller bubble will have higher pressure due to surface tension
Surface tension in Alveoli
- Alveoli are lined with a thin layer of water, and water has a high surface tension. Which means small alveoli have high pressure and wont inflate
Surface Tension in Alveoli and Surfactant
- Type 2 Alveolar Cells release surfactant to disrupt cohesive properties of water
- Surfactants reduce surface tension.
- Reduces the pressure in the alveolus
Surfactant
- Surfactant is more concentrated in smaller alveoli
- Reduces the surface tension of smaller alveoli more than large ones
- Results in an equalization of pressure across all alveoli
- Alveoli inflate uniformly
Compliance Work
- Balanced during the end of normal expiration (FRC)
- Increased with exercise
- Increased by diseases that cause fibrous of the lungs (CF)
Resistive Work
- Resistance = Pressure/Flow
- Increased by exercise
- Increased caused by diseases that restrict airflow
Airway Resistance
- Velocity of flow increases turbulence
- Increases resistance
- Velocity = Flow/Cross Sectional Area
Obstructive vs Restrictive Disease
- Obstructive disease: Resistive work is increased because the airways are obstructed, such as in asthma, emphysema, chronic bronchitis, and COPD.
- Restrictive disease: Elastic work is increased because the lung is stiff and non-compliant, as seen in interstitial lung disease, obesity hypoventilation syndrome, scoliosis, and cystic fibrosis.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.