Podcast
Questions and Answers
What is the primary cause of low PCO2 in ventilation-perfusion mismatching?
What is the primary cause of low PCO2 in ventilation-perfusion mismatching?
- Ventilatory response (correct)
- Alveolar hypoventilation
- Chronic hypoventilation
- Ventilation-perfusion ratios (VA/Q)
What is the characteristic of regions with low VA/Q in ventilation-perfusion mismatching?
What is the characteristic of regions with low VA/Q in ventilation-perfusion mismatching?
- They have normal ventilation and perfusion
- They have high oxygen content
- They qualitatively behave like right to left shunt (correct)
- They qualitatively behave like alveolar dead space
What is the effect of high VA/Q areas on oxygen content?
What is the effect of high VA/Q areas on oxygen content?
- They increase oxygen content (correct)
- They decrease oxygen content
- They have no effect on oxygen content
- They normalize oxygen content
What is the pH level in acute respiratory acidosis?
What is the pH level in acute respiratory acidosis?
What is the effect of chronic hypoventilation on pH levels?
What is the effect of chronic hypoventilation on pH levels?
What is the characteristic of ventilation-perfusion mismatching?
What is the characteristic of ventilation-perfusion mismatching?
What is the effect of low VA/Q areas on oxygen content?
What is the effect of low VA/Q areas on oxygen content?
What is the primary cause of high PCO2 in ventilation-perfusion mismatching?
What is the primary cause of high PCO2 in ventilation-perfusion mismatching?
What is the overall VA/Q ratio?
What is the overall VA/Q ratio?
What is the PAO2 in the normal lung?
What is the PAO2 in the normal lung?
What is the percentage of venous blood that passes through the lungs in normal right to left shunts?
What is the percentage of venous blood that passes through the lungs in normal right to left shunts?
What is the effect of a shunt on gas exchange?
What is the effect of a shunt on gas exchange?
What is the PACO2 in the normal lung?
What is the PACO2 in the normal lung?
What is the PaO2 in the dead space?
What is the PaO2 in the dead space?
What is the VA/Q ratio in the dead space?
What is the VA/Q ratio in the dead space?
What is the effect of a dead space on gas exchange?
What is the effect of a dead space on gas exchange?
What is the most likely reason for the low PaO2 and PaCO2 values in the blood gases provided?
What is the most likely reason for the low PaO2 and PaCO2 values in the blood gases provided?
What is the effect of a 20% shunt on arterial O2 content?
What is the effect of a 20% shunt on arterial O2 content?
Why does a moderate rise in CO2 content cause a very small rise in PCO2?
Why does a moderate rise in CO2 content cause a very small rise in PCO2?
What is the effect of increased ventilation on blood gases in a right to left shunt?
What is the effect of increased ventilation on blood gases in a right to left shunt?
What is the effect of breathing 100% oxygen on arterial PO2 in a right to left shunt?
What is the effect of breathing 100% oxygen on arterial PO2 in a right to left shunt?
What is the consequence of high pressure in the pulmonary circulation in Ventricular Septal Defect?
What is the consequence of high pressure in the pulmonary circulation in Ventricular Septal Defect?
What is the initial effect of Atrial Septal Defect and Ventricular Septal Defect on blood flow?
What is the initial effect of Atrial Septal Defect and Ventricular Septal Defect on blood flow?
Why can't you average the pressures in the calculation of the effect of a shunt on arterial O2 and CO2 contents?
Why can't you average the pressures in the calculation of the effect of a shunt on arterial O2 and CO2 contents?
What is the effect of hypoxic pulmonary vasoconstriction on blood flow?
What is the effect of hypoxic pulmonary vasoconstriction on blood flow?
What is the normal upper limit of the 'A-a' PO2 gradient in healthy young people?
What is the normal upper limit of the 'A-a' PO2 gradient in healthy young people?
Which of the following is NOT a mechanism leading to arterial hypoxia (low PaO2) that inevitably leads to an increase in PaCO2?
Which of the following is NOT a mechanism leading to arterial hypoxia (low PaO2) that inevitably leads to an increase in PaCO2?
What is the effect of systemic vasodilators on VA/Q matching?
What is the effect of systemic vasodilators on VA/Q matching?
What is the effect of increased pulmonary vascular resistance on the right heart?
What is the effect of increased pulmonary vascular resistance on the right heart?
What is the purpose of isotope ventilation and perfusion scans?
What is the purpose of isotope ventilation and perfusion scans?
What is the effect of regional VA/Q differences on disease localization?
What is the effect of regional VA/Q differences on disease localization?
What is the effect of hypoxic pulmonary vasoconstriction in the presence of global hypoxia?
What is the effect of hypoxic pulmonary vasoconstriction in the presence of global hypoxia?
What is the primary reason why high VA/Q areas do not compensate for the low VA/Q areas in their effects on arterial blood gases?
What is the primary reason why high VA/Q areas do not compensate for the low VA/Q areas in their effects on arterial blood gases?
What is the effect of gravity on VA/Q in the lungs?
What is the effect of gravity on VA/Q in the lungs?
What is the characteristic of pure right to left shunts in terms of VA/Q?
What is the characteristic of pure right to left shunts in terms of VA/Q?
What is the effect of ventilation-perfusion mismatching on arterial PO2 in response to O2 enriched inspired air?
What is the effect of ventilation-perfusion mismatching on arterial PO2 in response to O2 enriched inspired air?
What is the relationship between Q and VA in l/min-1 per unit lung volume?
What is the relationship between Q and VA in l/min-1 per unit lung volume?
What is the effect of high VA/Q areas on alveolar PO2?
What is the effect of high VA/Q areas on alveolar PO2?
What is the response to O2 enriched inspired air in terms of arterial PO2 in pure right to left shunts?
What is the response to O2 enriched inspired air in terms of arterial PO2 in pure right to left shunts?
What is the effect of ventilation-perfusion mismatching on normal upright lung?
What is the effect of ventilation-perfusion mismatching on normal upright lung?
Study Notes
Shunt, Dead Space, and VA/Q
- VA/Q = 0.8, indicating incomplete gas exchange
- Shunt: blood that bypasses alveolar gas exchange, resulting in no oxygenation and no CO2 removal
- Dead space: ventilated areas with no perfusion, resulting in no gas exchange
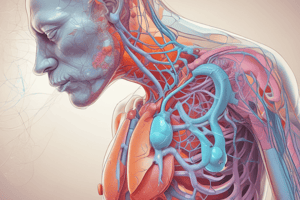
Right-to-Left Shunts
- Normal right-to-left shunts: >98% of venous blood passes through the lungs, but a small amount from bronchial veins and Thebesian veins bypasses gas exchange
- Abnormal right-to-left shunts: occur in conditions like collapsed lung, pneumonia, and congenital heart diseases
- Atrial Septal Defect (ASD) and Ventricular Septal Defect (VSD) can cause right-to-left shunts, leading to low arterial oxygen content and PO2
Effect of Shunts on Arterial O2 and CO2 Contents
- Shunt effect: a weighted average of contents in the shunted and unshunted blood
- Calculating the effect on PO2 and PCO2 using dissociation curves
- O2 content: a moderate fall in O2 content causes a large fall in PO2
- CO2 content: a moderate rise in CO2 content causes a small rise in PCO2
Effect of Increased Ventilation or FIO2 on Right-to-Left Shunts
- Stimulates chemoreceptors, leading to increased ventilation
- Ventilated areas lose more CO2, but gain little extra O2 (haemoglobin already saturated)
- Shunt blood remains unaffected
- Final blood gases: low PaO2, normal or low PaCO2
Ventilation-Perfusion Mismatching
- Inequalities in VA/Q lead to both dead space and shunt effects
- Regions with high VA/Q (dead space) and low VA/Q (shunt) cannot be balanced
- Low O2 content and high CO2 content in arterial blood
Response to O2 Enriched Inspired Air
- Pure right-to-left shunts: minimal improvement in arterial PO2
- Ventilation-perfusion mismatching: marked improvement in arterial PO2 due to increased PO2 in under-ventilated areas
Regional VA/Q Differences
- Gravity affects perfusion and ventilation, resulting in higher VA/Q at the top of the lungs
- Accounts for the PO2 A-a difference
Hypoxic Pulmonary Vasoconstriction
- Pulmonary blood vessels vasoconstrict in response to hypoxia
- Diverts blood flow from poorly ventilated areas to well-ventilated areas, improving VA/Q matching and arterial oxygenation
- Not helpful in global hypoxia, as it increases pulmonary vascular resistance and load on the right heart
Assessment of Ventilation-Perfusion Mismatching
- Isotope ventilation and perfusion scans
- Measuring alveolar dead space and shunt effect using inert gases and modified Bohr and shunt equations
- From "A-a" PO2 gradient, which increases with age
Mechanisms Leading to Arterial Hypoxia
- Hypoventilation, shunt, dead space, and ventilation-perfusion mismatching
- Only hypoventilation inevitably leads to increased PaCO2, while other causes usually lead to normal or reduced PaCO2.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This quiz assesses understanding of ventilation-perfusion ratio, shunt, dead space, and gas exchange in respiratory physiology. Calculate VA and Q values and interpret PAO2 and PICO2 levels.