Podcast
Questions and Answers
What is the primary purpose of the respiratory membrane?
What is the primary purpose of the respiratory membrane?
- To facilitate gas exchange (correct)
- To protect the lungs from infections
- To produce pulmonary surfactant
- To filter air before it enters the lungs
The diffusion of gas is enhanced by a thick respiratory membrane.
The diffusion of gas is enhanced by a thick respiratory membrane.
False (B)
What two structures make up the respiratory membrane?
What two structures make up the respiratory membrane?
The wall of the alveolus and the wall of the pulmonary capillary.
Gas exchange occurs by ________ across the respiratory membrane.
Gas exchange occurs by ________ across the respiratory membrane.
Which factor is NOT mentioned as influencing the effectiveness of gas diffusion?
Which factor is NOT mentioned as influencing the effectiveness of gas diffusion?
Match the factors affecting gas diffusion with their descriptions:
Match the factors affecting gas diffusion with their descriptions:
Pulmonary surfactant primarily aids in gas exchange directly.
Pulmonary surfactant primarily aids in gas exchange directly.
Name one factor that determines the effectiveness of gas diffusion.
Name one factor that determines the effectiveness of gas diffusion.
What is the total thickness of the alveolar and capillary walls combined?
What is the total thickness of the alveolar and capillary walls combined?
Only oxygen (O2) needs to dissolve in the alveolar fluid before diffusion occurs.
Only oxygen (O2) needs to dissolve in the alveolar fluid before diffusion occurs.
How many alveoli are there approximately in the human lungs?
How many alveoli are there approximately in the human lungs?
Carbon dioxide (CO2) is approximately ___ times more soluble than oxygen (O2).
Carbon dioxide (CO2) is approximately ___ times more soluble than oxygen (O2).
Match the following components with their descriptions:
Match the following components with their descriptions:
The total surface area available for gas exchange in the lungs is approximately 75 m².
The total surface area available for gas exchange in the lungs is approximately 75 m².
What is the primary function of the alveoli in the lungs?
What is the primary function of the alveoli in the lungs?
The respiratory membrane consists of the ___ wall and the ___ wall.
The respiratory membrane consists of the ___ wall and the ___ wall.
What percentage of atmospheric pressure is contributed by nitrogen (N2)?
What percentage of atmospheric pressure is contributed by nitrogen (N2)?
The total atmospheric pressure is made up entirely of oxygen (O2).
The total atmospheric pressure is made up entirely of oxygen (O2).
What is the typical partial pressure of oxygen (PO2) in the lungs?
What is the typical partial pressure of oxygen (PO2) in the lungs?
In atmospheric air, the partial pressure of nitrogen is ___ mmHg.
In atmospheric air, the partial pressure of nitrogen is ___ mmHg.
Match the gas with its corresponding role in atmospheric pressure:
Match the gas with its corresponding role in atmospheric pressure:
What happens to the diffusion of oxygen (O2) when the partial pressures are equal?
What happens to the diffusion of oxygen (O2) when the partial pressures are equal?
The partial pressure of a gas contributes to its diffusion force.
The partial pressure of a gas contributes to its diffusion force.
What is the driving force for gas diffusion?
What is the driving force for gas diffusion?
The driving force for gas diffusion in the lungs is maintained through a ___ pressure gradient.
The driving force for gas diffusion in the lungs is maintained through a ___ pressure gradient.
What is the calculated partial pressure of nitrogen (PN2) at sea level (760 mmHg)?
What is the calculated partial pressure of nitrogen (PN2) at sea level (760 mmHg)?
What is primarily responsible for increasing the surface area of food in the stomach?
What is primarily responsible for increasing the surface area of food in the stomach?
Clinical conditions like Crohn’s disease do not affect the surface area for absorption in the small intestine.
Clinical conditions like Crohn’s disease do not affect the surface area for absorption in the small intestine.
What does cholera toxin chronically activate?
What does cholera toxin chronically activate?
The main function of villi in the small intestine is __________.
The main function of villi in the small intestine is __________.
Match the disease with its effect on intestinal absorption:
Match the disease with its effect on intestinal absorption:
Which of the following cells is primarily responsible for secreting mucous in the intestines?
Which of the following cells is primarily responsible for secreting mucous in the intestines?
Kwashiorkor is a form of malnutrition that occurs due to protein deficiency.
Kwashiorkor is a form of malnutrition that occurs due to protein deficiency.
What is the primary problem caused by diverticula in the intestines?
What is the primary problem caused by diverticula in the intestines?
Microvilli are found on the __________ of enterocytes.
Microvilli are found on the __________ of enterocytes.
What triggers the immune response in coeliac disease?
What triggers the immune response in coeliac disease?
Plicae circularis are small finger-like projections in the large intestine.
Plicae circularis are small finger-like projections in the large intestine.
What are the major two forms of malnutrition associated with starvation?
What are the major two forms of malnutrition associated with starvation?
__________ is the main factor in facilitating diffusion of gases across the respiratory membrane.
__________ is the main factor in facilitating diffusion of gases across the respiratory membrane.
Which of the following is a function of pepsinogen in the stomach?
Which of the following is a function of pepsinogen in the stomach?
Match the following absorption problems with their corresponding conditions:
Match the following absorption problems with their corresponding conditions:
What can occur when ventilation is compromised?
What can occur when ventilation is compromised?
Bronchoconstriction results in good ventilation.
Bronchoconstriction results in good ventilation.
What is the normal partial pressure of oxygen (PO2) in the alveoli?
What is the normal partial pressure of oxygen (PO2) in the alveoli?
Ventilation-perfusion matching helps to maintain a high level of ____ in the blood.
Ventilation-perfusion matching helps to maintain a high level of ____ in the blood.
Match the following conditions with their effects on ventilation:
Match the following conditions with their effects on ventilation:
Which statement is true regarding maternal and fetal oxygen levels?
Which statement is true regarding maternal and fetal oxygen levels?
Alveolar PO2 levels can drop significantly without causing hypoxaemia.
Alveolar PO2 levels can drop significantly without causing hypoxaemia.
What physiological mechanism helps redirect blood vessels in the pulmonary system?
What physiological mechanism helps redirect blood vessels in the pulmonary system?
When blood passes through the alveoli with a PO2 of 40 mmHg, it indicates ____ oxygen levels.
When blood passes through the alveoli with a PO2 of 40 mmHg, it indicates ____ oxygen levels.
What effect does poor ventilation have on oxygen levels?
What effect does poor ventilation have on oxygen levels?
What happens in a lung region when there is a decrease in CO2 concentration?
What happens in a lung region when there is a decrease in CO2 concentration?
Increased CO2 concentration leads to the dilation of bronchioles.
Increased CO2 concentration leads to the dilation of bronchioles.
What is the primary effect of a greater blood flow than airflow in the lungs?
What is the primary effect of a greater blood flow than airflow in the lungs?
When airflow is greater than blood flow, there is _____ of local pulmonary artery smooth muscle.
When airflow is greater than blood flow, there is _____ of local pulmonary artery smooth muscle.
Match the following scenarios with their respective effects:
Match the following scenarios with their respective effects:
What balance is achieved when CO2 concentration is high in a lung region?
What balance is achieved when CO2 concentration is high in a lung region?
Airway resistance increases when blood flow is greater than airflow.
Airway resistance increases when blood flow is greater than airflow.
What is the partial pressure of oxygen (PO2) in the region with constricted blood flow?
What is the partial pressure of oxygen (PO2) in the region with constricted blood flow?
Under conditions of increased blood flow, local airways experience _____ of smooth muscle.
Under conditions of increased blood flow, local airways experience _____ of smooth muscle.
What is the effect of small blood flow in a lung region?
What is the effect of small blood flow in a lung region?
Flashcards
Gastric ulcer base
Gastric ulcer base
The part of a gastric ulcer that is free of tissue damage.
Surface area (digestion)
Surface area (digestion)
The crucial importance of a large surface area within the digestive system for effective breakdown and absorption of food.
Mastication
Mastication
The mechanical breakdown of food in the mouth.
Small intestine's surface area
Small intestine's surface area
Signup and view all the flashcards
Plicae circularis
Plicae circularis
Signup and view all the flashcards
Villus
Villus
Signup and view all the flashcards
Microvilli
Microvilli
Signup and view all the flashcards
Coeliac disease
Coeliac disease
Signup and view all the flashcards
Diverticulitis
Diverticulitis
Signup and view all the flashcards
Cholera toxin
Cholera toxin
Signup and view all the flashcards
CFTR Cl- channel
CFTR Cl- channel
Signup and view all the flashcards
Kwashiorkor and Marasmus
Kwashiorkor and Marasmus
Signup and view all the flashcards
Respiratory membrane diffusion
Respiratory membrane diffusion
Signup and view all the flashcards
Alveolar Wall
Alveolar Wall
Signup and view all the flashcards
Capillary Wall
Capillary Wall
Signup and view all the flashcards
Respiratory Membrane
Respiratory Membrane
Signup and view all the flashcards
Surface Area for Gas Exchange
Surface Area for Gas Exchange
Signup and view all the flashcards
Solubility of Gases
Solubility of Gases
Signup and view all the flashcards
Oxygen Diffusion
Oxygen Diffusion
Signup and view all the flashcards
Carbon Dioxide Diffusion
Carbon Dioxide Diffusion
Signup and view all the flashcards
Haemoglobin
Haemoglobin
Signup and view all the flashcards
Alveolus
Alveolus
Signup and view all the flashcards
Pulmonary Capillary
Pulmonary Capillary
Signup and view all the flashcards
Diffusion
Diffusion
Signup and view all the flashcards
Driving Force for Diffusion
Driving Force for Diffusion
Signup and view all the flashcards
Partial Pressure Gradient
Partial Pressure Gradient
Signup and view all the flashcards
Diffusion Distance
Diffusion Distance
Signup and view all the flashcards
Pulmonary Surfactant
Pulmonary Surfactant
Signup and view all the flashcards
Partial Pressure
Partial Pressure
Signup and view all the flashcards
What drives gas diffusion?
What drives gas diffusion?
Signup and view all the flashcards
PN2 in the atmosphere
PN2 in the atmosphere
Signup and view all the flashcards
Alveolar PO2
Alveolar PO2
Signup and view all the flashcards
How does PO2 affect diffusion?
How does PO2 affect diffusion?
Signup and view all the flashcards
Why is partial pressure important?
Why is partial pressure important?
Signup and view all the flashcards
How is partial pressure maintained?
How is partial pressure maintained?
Signup and view all the flashcards
What happens when partial pressure is equal?
What happens when partial pressure is equal?
Signup and view all the flashcards
Oxygen concentration in blood
Oxygen concentration in blood
Signup and view all the flashcards
What is the role of the respiratory membrane?
What is the role of the respiratory membrane?
Signup and view all the flashcards
Ventilation-Perfusion Matching
Ventilation-Perfusion Matching
Signup and view all the flashcards
Constricted Bronchioles
Constricted Bronchioles
Signup and view all the flashcards
Dilated Bronchioles
Dilated Bronchioles
Signup and view all the flashcards
Blood Flow (Perfusion)
Blood Flow (Perfusion)
Signup and view all the flashcards
Airflow (Ventilation)
Airflow (Ventilation)
Signup and view all the flashcards
PO2
PO2
Signup and view all the flashcards
High PO2
High PO2
Signup and view all the flashcards
Low PO2
Low PO2
Signup and view all the flashcards
CO2 Concentration
CO2 Concentration
Signup and view all the flashcards
Smooth Muscle Relaxation
Smooth Muscle Relaxation
Signup and view all the flashcards
Hypoxaemia
Hypoxaemia
Signup and view all the flashcards
What compromises ventilation- perfusion matching?
What compromises ventilation- perfusion matching?
Signup and view all the flashcards
How does bronchoconstriction affect ventilation-perfusion matching?
How does bronchoconstriction affect ventilation-perfusion matching?
Signup and view all the flashcards
Local controls on pulmonary blood vessels
Local controls on pulmonary blood vessels
Signup and view all the flashcards
How do local controls help maintain oxygen levels?
How do local controls help maintain oxygen levels?
Signup and view all the flashcards
What happens to the blood in poorly ventilated areas?
What happens to the blood in poorly ventilated areas?
Signup and view all the flashcards
Why PO2 is higher in alveoli than in blood?
Why PO2 is higher in alveoli than in blood?
Signup and view all the flashcards
What is the result of ventilation-perfusion mismatch?
What is the result of ventilation-perfusion mismatch?
Signup and view all the flashcards
How does the body compensate for ventilation-perfusion mismatch?
How does the body compensate for ventilation-perfusion mismatch?
Signup and view all the flashcards
Study Notes
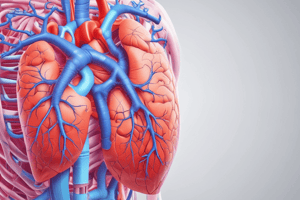
Respiratory Membrane
- The primary purpose of the respiratory membrane is to facilitate gas exchange between the air in the alveoli and the blood in the capillaries.
- The respiratory membrane is made up of two structures: the thin wall of the alveoli and the thin wall of the capillaries.
- Gas exchange occurs by diffusion across the respiratory membrane.
- The effectiveness of gas diffusion is NOT influenced by the thickness of the respiratory membrane.
Factors Affecting Gas Diffusion
- Pulmonary surfactant aids in gas exchange by reducing surface tension in the alveoli, which prevents them from collapsing.
- Partial pressure gradient is a key factor determining the effectiveness of gas diffusion.
- The total thickness of the alveolar and capillary walls combined is 0.5 micrometers.
- Oxygen (O2) needs to dissolve in the alveolar fluid before diffusion occurs.
- There are approximately 300 million alveoli in the human lungs.
- Carbon dioxide (CO2) is approximately 20 times more soluble than oxygen (O2).
Components of the Respiratory Membrane and Gas Exchange
- The total surface area available for gas exchange in the lungs is approximately 75 m².
- The primary function of the alveoli in the lungs is gas exchange.
- The respiratory membrane consists of the alveolar wall and the capillary wall.
- Nitrogen (N2) contributes 78% of atmospheric pressure.
- The total atmospheric pressure is NOT made up entirely of oxygen (O2).
- The typical partial pressure of oxygen (PO2) in the lungs is 100 mmHg.
- In atmospheric air, the partial pressure of nitrogen is 593 mmHg.
Gas Diffusion and Partial Pressure
- Nitrogen (N2) is the primary component of atmospheric pressure.
- Oxygen (O2) makes up 21% of atmospheric pressure.
- Carbon dioxide (CO2) contributes 0.04% to atmospheric pressure.
- Diffusion of oxygen (O2) stops when the partial pressures are equal.
- The partial pressure of a gas contributes to its diffusion force.
- The driving force for gas diffusion is the difference in partial pressure between the alveoli and the blood.
- The driving force for gas diffusion in the lungs is maintained through a pressure gradient.
- The calculated partial pressure of nitrogen (PN2) at sea level (760 mmHg) is 593 mmHg.
Intestinal Absorption
- Plicae circularis, villi, and microvilli are all features that increase the surface area of the small intestine for absorption.
- Cholera toxin chronically activates adenylate cyclase.
- The main function of villi in the small intestine is absorption of nutrients.
- Crohn's disease affects the surface area for absorption in the small intestine.
- Celiac disease triggers the immune response through gluten.
- Kwashiorkor is a form of malnutrition that occurs due to protein deficiency.
- Diverticula in the intestines can cause inflammation, pain, and bleeding.
- Microvilli are found on the apical surface of enterocytes.
- Plicae circularis are small finger-like projections in the small intestine.
- The two major forms of malnutrition associated with starvation are marasmus and kwashiorkor.
Factors Affecting Gas Diffusion
- The partial pressure gradient is the main factor facilitating diffusion of gases across the respiratory membrane.
- Pepsinogen in the stomach functions as a precursor to pepsin, which breaks down proteins.
- Lactose intolerance is a condition caused by a deficiency in lactase, leading to lactose malabsorption.
- Celiac disease is triggered by gluten, leading to damage in the small intestine and malabsorption.
- Crohn's disease can cause malabsorption due to inflammation and damage in the small intestine.
Ventilation and Gas Exchange
- When ventilation is compromised, hypoxia can occur due to decreased oxygen levels in the blood.
- Bronchoconstriction does NOT result in good ventilation.
- The normal partial pressure of oxygen (PO2) in the alveoli is 100 mmHg.
- Ventilation-perfusion matching helps maintain a high level of oxygen in the blood.
- Asthma can cause airway narrowing and increased airway resistance.
- Pneumonia causes inflammation in the lungs, leading to decreased gas exchange.
- Pulmonary embolism blocks blood flow to the lungs, decreasing gas exchange.
- Chronic obstructive pulmonary disease (COPD) is a condition characterized by airflow limitation and difficulty exhaling.
- Emphysema causes damage to the alveoli, reducing the surface area for gas exchange.
Maternal and Fetal Oxygen Levels
- Maternal and fetal oxygen levels are NEVER equal due to the barrier presented by the placenta.
- Alveolar PO2 levels can drop significantly without causing hypoxaemia.
- The hypoxic vasoconstriction mechanism helps redirect blood vessels in the pulmonary system.
- When blood passes through the alveoli with a PO2 of 40 mmHg, it indicates low oxygen levels.
- Poor ventilation results in decreased oxygen levels.
- In a lung region with a decrease in CO2 concentration, bronchoconstriction occurs.
- Increased CO2 concentration leads to the dilation of bronchioles.
Ventilation-Perfusion Matching
- A greater blood flow than airflow in the lungs results in shunting, where poorly oxygenated blood bypasses the alveoli.
- When airflow is greater than blood flow, there is constriction of local pulmonary artery smooth muscle.
- When CO2 concentration is high in a lung region, a balance is achieved by constricting blood flow and dilating airways.
- Airway resistance increases when blood flow is greater than airflow.
- The partial pressure of oxygen (PO2) in the region with constricted blood flow is lower than in regions with normal blood flow.
- Under conditions of increased blood flow, local airways experience dilation of smooth muscle.
- Small blood flow in a lung region results in vasoconstriction of pulmonary arterioles.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.