Podcast
Questions and Answers
A patient with a history of heart failure reports experiencing shortness of breath while lying flat. Which respiratory condition is most likely indicated by this symptom?
A patient with a history of heart failure reports experiencing shortness of breath while lying flat. Which respiratory condition is most likely indicated by this symptom?
- Cheyne-Stokes respiration
- Hyperpnea
- Orthopnea (correct)
- Hypoxia
Which set of signs and symptoms would most strongly suggest the presence of hypoxia?
Which set of signs and symptoms would most strongly suggest the presence of hypoxia?
- Normal pulse rate, normal respiratory rate, and absence of cyanosis
- Slow pulse rate, shallow respirations, and lethargy
- Decreased pulse rate, deep respirations, and flushed skin
- Increased pulse rate, increased rate and depth of respirations, and cyanosis (correct)
A patient is exhibiting respirations that gradually increase in rate and depth, followed by a period of apnea. Which respiratory pattern is the patient demonstrating?
A patient is exhibiting respirations that gradually increase in rate and depth, followed by a period of apnea. Which respiratory pattern is the patient demonstrating?
- Cheyne-Stokes respiration (correct)
- Hyperpnea
- Dyspnea
- Orthopnea
A patient presents to the emergency room with rapid and deep breathing, and reports feeling anxious. Which respiratory condition is most likely occurring?
A patient presents to the emergency room with rapid and deep breathing, and reports feeling anxious. Which respiratory condition is most likely occurring?
A dark-skinned patient is suspected of having hypoxia. Where would cyanosis be most readily observed?
A dark-skinned patient is suspected of having hypoxia. Where would cyanosis be most readily observed?
Which of the following scenarios would MOST directly indicate an alteration in the alveolar gas exchange process?
Which of the following scenarios would MOST directly indicate an alteration in the alveolar gas exchange process?
A client with chronic obstructive pulmonary disease (COPD) is short of breath and using an oxygen tank. Why should a caregiver avoid increasing the oxygen flow rate without specific orders?
A client with chronic obstructive pulmonary disease (COPD) is short of breath and using an oxygen tank. Why should a caregiver avoid increasing the oxygen flow rate without specific orders?
A client is experiencing shortness of breath. Which action should the caregiver prioritize, assuming all are within their scope of practice?
A client is experiencing shortness of breath. Which action should the caregiver prioritize, assuming all are within their scope of practice?
A client with a respiratory condition exhibits orthopnea. What intervention would MOST likely provide immediate relief?
A client with a respiratory condition exhibits orthopnea. What intervention would MOST likely provide immediate relief?
Which of the following best describes the relationship between oxygen consumption and the effort of breathing when a client is struggling to breathe?
Which of the following best describes the relationship between oxygen consumption and the effort of breathing when a client is struggling to breathe?
Which of the following statements is MOST accurate regarding the role of a support worker in oxygen therapy?
Which of the following statements is MOST accurate regarding the role of a support worker in oxygen therapy?
A client receiving oxygen therapy exhibits a decreased respiratory rate. What is the MOST appropriate initial action for a support worker?
A client receiving oxygen therapy exhibits a decreased respiratory rate. What is the MOST appropriate initial action for a support worker?
Supplemental oxygen is typically administered to clients to:
Supplemental oxygen is typically administered to clients to:
Which healthcare professional is primarily responsible for evaluating, treating, and maintaining a client’s heart and lung function?
Which healthcare professional is primarily responsible for evaluating, treating, and maintaining a client’s heart and lung function?
Oxygen is considered a medication because:
Oxygen is considered a medication because:
A client with a history of heart disease is prescribed oxygen PRN for chest pain. What does 'PRN' indicate in this context?
A client with a history of heart disease is prescribed oxygen PRN for chest pain. What does 'PRN' indicate in this context?
Which route is NOT considered a typical airway for oxygen to enter the body?
Which route is NOT considered a typical airway for oxygen to enter the body?
What could happen if a client receives too much oxygen?
What could happen if a client receives too much oxygen?
A client reports experiencing chest pain that worsens with deep breathing and coughing. Which characteristic of the pain is MOST important to document?
A client reports experiencing chest pain that worsens with deep breathing and coughing. Which characteristic of the pain is MOST important to document?
A patient presents with respirations of 30 per minute following a strenuous workout. The patient denies pain and has no fever. What is the MOST likely cause of their tachypnea?
A patient presents with respirations of 30 per minute following a strenuous workout. The patient denies pain and has no fever. What is the MOST likely cause of their tachypnea?
What is the PRIMARY characteristic that differentiates Kussmaul respirations from tachypnea?
What is the PRIMARY characteristic that differentiates Kussmaul respirations from tachypnea?
A nurse observes a client sitting upright and leaning forward. What respiratory condition is the client MOST likely trying to alleviate?
A nurse observes a client sitting upright and leaning forward. What respiratory condition is the client MOST likely trying to alleviate?
A patient with pneumonia is exhibiting slow, shallow, and irregular respirations. Which of the following terms BEST describes this patient's respiratory pattern?
A patient with pneumonia is exhibiting slow, shallow, and irregular respirations. Which of the following terms BEST describes this patient's respiratory pattern?
A client is admitted with a suspected drug overdose and is exhibiting a respiratory rate of 8 breaths per minute. Which of the following BEST describes this respiratory pattern?
A client is admitted with a suspected drug overdose and is exhibiting a respiratory rate of 8 breaths per minute. Which of the following BEST describes this respiratory pattern?
When assessing a client's sputum, what characteristics should be noted?
When assessing a client's sputum, what characteristics should be noted?
A patient is experiencing diabetic acidosis. Which respiratory pattern would the nurse expect to observe?
A patient is experiencing diabetic acidosis. Which respiratory pattern would the nurse expect to observe?
Flashcards
Ventilation
Ventilation
Movement of air into and out of the lungs.
Alveolar Exchange
Alveolar Exchange
O2 and CO2 exchange at the alveoli.
Gas Transport
Gas Transport
Blood carries O2 to cells, removes CO2.
SOB/SOBOE
SOB/SOBOE
Signup and view all the flashcards
Orthopnea
Orthopnea
Signup and view all the flashcards
Oxygen (O2)
Oxygen (O2)
Signup and view all the flashcards
Airway
Airway
Signup and view all the flashcards
Supplemental Oxygen
Supplemental Oxygen
Signup and view all the flashcards
Oxygen Therapy
Oxygen Therapy
Signup and view all the flashcards
Oxygen Prescription
Oxygen Prescription
Signup and view all the flashcards
Respiratory Therapist
Respiratory Therapist
Signup and view all the flashcards
Too Much Oxygen
Too Much Oxygen
Signup and view all the flashcards
Safe Oxygen Administration
Safe Oxygen Administration
Signup and view all the flashcards
Hyperventilation
Hyperventilation
Signup and view all the flashcards
Dyspnea
Dyspnea
Signup and view all the flashcards
Cheyne-Stokes Respirations
Cheyne-Stokes Respirations
Signup and view all the flashcards
Hypoxia
Hypoxia
Signup and view all the flashcards
Cyanosis
Cyanosis
Signup and view all the flashcards
Productive Cough
Productive Cough
Signup and view all the flashcards
Hemoptysis
Hemoptysis
Signup and view all the flashcards
Eupnea
Eupnea
Signup and view all the flashcards
Tachypnea
Tachypnea
Signup and view all the flashcards
Bradypnea
Bradypnea
Signup and view all the flashcards
Apnea
Apnea
Signup and view all the flashcards
Study Notes
- Oxygen (O2) is a colorless, odorless, and tasteless gas that is essential for life
- Without oxygen, death can occur within minutes
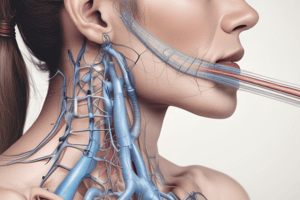
- Oxygen enters the body through the airway, which includes the nose, mouth, breathing tube or tracheostomy
Supplemental Oxygen
- Support workers often assist clients who have difficulty breathing or absorbing oxygen
- These clients require supplemental oxygen supplied via nasal tube or face mask
- It is the support worker's responsibility to provide safe and effective care
Oxygen Therapy
- Oxygen therapy involves administering oxygen at concentrations greater than those in room air
- Only qualified healthcare providers, such as physicians or nurse practitioners, can prescribe oxygen therapy
- The prescription includes the amount of oxygen, the type of device, and the duration of therapy
- Respiratory therapists or nurses usually set up the oxygen device and provide respiratory therapies
- Respiratory therapists evaluate, treat, and maintain lung function to help clients keep breathing
Oxygen Needs
- Some clients need oxygen constantly, while others need it for symptom relief, such as chest pain or shortness of breath
- It is crucial to administer only the prescribed amount of oxygen
- Excessive oxygen can dangerously slow the client's respiratory rate
Task Considerations
Before assisting with any care, ensure that:
- The task is within your scope of practice according to your province or territory
- The task is part of your job description at your facility or agency
- You have received the necessary training
- You know how to use the equipment properly
- A nurse or respiratory technician provides supervision
Altered Respiratory Function
- Respiratory function involves three processes: air movement into and out of the lungs, O2 and CO2 exchange in the alveoli, and O2 transport to cells with CO2 removal
- Altered respiratory function occurs when any of these processes are affected
- Shortness of breath (SOB) or shortness of breath on exertion (SOBOE) indicates altered respiratory function
- Clients with breathing difficulties may panic, feel anxious, and struggle to breathe, often preferring to sit upright (orthopnea)
- Struggling to breathe is exhausting and dangerous, requiring prompt and accurate reporting to supervisors
- Never increase the oxygen level on an oxygen tank unless directed by the client's care plan, as it can be harmful
Signs and Symptoms of Altered Respiratory Function
- Hypoxia
- Abnormal breathing pattern
- Shortness of breath
- Cough (note frequency and time of day)
- Dry or hacking cough
- Harsh or barking cough
- Productive (sputum-producing) or nonproductive cough
- Sputum color (clear, white, yellow, green, brown, or red)
- Sputum odor (none or foul)
- Sputum consistency (thick, watery, or frothy)
- Hemoptysis (bloody sputum)
- Noisy respirations
- Wheezing
- Wet-sounding respirations
- Crowing sounds
- Chest pain location
- Constant or intermittent chest pain
- Description of chest pain (stabbing, knifelike, aching)
- Factors that worsen chest pain (movement, coughing, yawning, sneezing, sighing, deep breathing)
- Cyanosis (skin, mucous membranes, lips, nail beds)
- Changes in vital signs
- Body position (sitting upright, leaning forward or hunched over a table)
Abnormal Respiratory Patterns
- Normal respiration rate for adults is 12 to 20 per minute; infants and children have faster rates
- Normal respirations are quiet, effortless, and regular, with uniform chest rise and fall
- Eupnea is the medical term for normal respirations
- Tachypnea is rapid breathing (over 20 respirations per minute) caused by fever, exercise, pain, airway obstruction, or hypoxemia
- Bradypnea is slow breathing (fewer than 12 respirations per minute) caused by drug overdoses or nervous system disorders
- Apnea is the absence of breathing, occurring in cardiac or respiratory arrest
- Kussmaul respirations are deep and rapid, characteristic of diabetic acidosis
- Hypoventilation involves slow, shallow, and irregular respirations caused by lung disorders, obesity, airway obstruction, or drug effects
- Hyperventilation involves rapid and deeper-than-normal respirations caused by asthma, emphysema, infection, fever, nervous system disorders, hypoxia, anxiety, pain, or drugs
- Dyspnea is difficult, labored, or painful breathing caused by heart disease, exercise, or anxiety
- Cheyne-Stokes respirations gradually increase in rate and depth, then become shallow and slow, with possible apnea for 10 to 20 seconds; common near death
- Orthopnea is shortness of breath when lying flat, relieved by sitting or standing, caused by emphysema, asthma, pneumonia, angina pectoris, or heart disorders
Hypoxia
- Hypoxia is a deficiency of oxygen in the cells due to abnormal respiratory function, caused by illness, disease, injury, or surgery
- Hypoxia is life-threatening, leading to cell damage or death
- Restlessness
- Dizziness
- Disorientation
- Confusion
- Behavior and personality changes
- Difficulty concentrating and following directions
- Apprehension
- Anxiety
- Fatigue
- Agitation
- Increased pulse rate
- Increased rate and depth of respirations
- Sitting position, often leaning forward
- Cyanosis (bluish skin, mucous membranes, lips, nail beds)
- Dyspnea
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.