Podcast
Questions and Answers
What are the primary functions of the upper airway?
What are the primary functions of the upper airway?
- Facilitating laminar flow and conduit for air
- Tissue hydration and trapping of pathogens
- Warming and humidification of inspired gases
- All of the above (correct)
What determines whether airflow is laminar or turbulent?
What determines whether airflow is laminar or turbulent?
- Viscosity of gas
- Reynold's number (correct)
- Density of gas
- Cross-sectional area of airways
At which level of the airways do they lose all cartilage?
At which level of the airways do they lose all cartilage?
- Bronchi
- Bronchioles (correct)
- Trachea
- Alveoli
What is the effect of increasing division of airways on airflow resistance?
What is the effect of increasing division of airways on airflow resistance?
Which type of alveolar cell is responsible for gas exchange?
Which type of alveolar cell is responsible for gas exchange?
What should a functional assessment of the respiratory system include?
What should a functional assessment of the respiratory system include?
What is the typical duration for airway hyperreactivity to resolve after an upper respiratory infection?
What is the typical duration for airway hyperreactivity to resolve after an upper respiratory infection?
When providing anesthesia care for a patient with an upper airway infection, what strategies might reduce the risk of adverse airway events?
When providing anesthesia care for a patient with an upper airway infection, what strategies might reduce the risk of adverse airway events?
Which of the following medications is NOT typically used to treat asthma?
Which of the following medications is NOT typically used to treat asthma?
What is the primary method used to assess the severity of COPD?
What is the primary method used to assess the severity of COPD?
What is the sum of ERV and RV in a lung?
What is the sum of ERV and RV in a lung?
Which of the following lung volumes is not a part of vital capacity?
Which of the following lung volumes is not a part of vital capacity?
What is the minimum VO2 max required for a post-thoracotomy patient to have a lower risk of poor outcomes?
What is the minimum VO2 max required for a post-thoracotomy patient to have a lower risk of poor outcomes?
What is the most common cause of upper respiratory infections in children?
What is the most common cause of upper respiratory infections in children?
What is the percentage of upper respiratory infections caused by viral or bacterial nasopharyngitis?
What is the percentage of upper respiratory infections caused by viral or bacterial nasopharyngitis?
What is the primary mechanism underlying desaturation in obese patients during anesthesia?
What is the primary mechanism underlying desaturation in obese patients during anesthesia?
What is the primary indicator of pulmonary hypertension?
What is the primary indicator of pulmonary hypertension?
Which of the following is NOT a risk factor for obstructive sleep apnea?
Which of the following is NOT a risk factor for obstructive sleep apnea?
What is the primary benefit of applying PEEP during anesthesia in morbidly obese patients?
What is the primary benefit of applying PEEP during anesthesia in morbidly obese patients?
What percentage of patients with pulmonary hypertension experience dyspnea?
What percentage of patients with pulmonary hypertension experience dyspnea?
What is the primary indicator of severe pulmonary hypertension?
What is the primary indicator of severe pulmonary hypertension?
What is the primary diagnostic test for identifying valvular disorders, right ventricular function abnormalities, and left ventricular failure in pulmonary hypertensive patients?
What is the primary diagnostic test for identifying valvular disorders, right ventricular function abnormalities, and left ventricular failure in pulmonary hypertensive patients?
What is the primary benefit of smoking cessation in terms of wound healing?
What is the primary benefit of smoking cessation in terms of wound healing?
What is the primary implication of Schamroth's sign?
What is the primary implication of Schamroth's sign?
What is the recommended time frame for smoking cessation before surgery?
What is the recommended time frame for smoking cessation before surgery?
What is the primary mechanism by which smoking cessation improves mitochondrial function?
What is the primary mechanism by which smoking cessation improves mitochondrial function?
What organs tend to obstruct the upper airway when the patient is under the influence of anesthesia?
What organs tend to obstruct the upper airway when the patient is under the influence of anesthesia?
What is airflow directly proportional to, and inversely proportional to?
What is airflow directly proportional to, and inversely proportional to?
Laminar flow resistance primarily reflects what property of gas?
Laminar flow resistance primarily reflects what property of gas?
Turbulent flow reflects what property of gas?
Turbulent flow reflects what property of gas?
What type of airflow potentiates the trapping of inhaled particulate matter?
What type of airflow potentiates the trapping of inhaled particulate matter?
Where does the trachea terminate?
Where does the trachea terminate?
What is unique about the right mainstem bronchus?
What is unique about the right mainstem bronchus?
Which generations of airways are used for conducting air?
Which generations of airways are used for conducting air?
What is the definition of an acinus in the context of the respiratory system?
What is the definition of an acinus in the context of the respiratory system?
What is the function of Type II alveolar cells?
What is the function of Type II alveolar cells?
What are the key features of a lung exam?
What are the key features of a lung exam?
What is the definition of total lung capacity?
What is the definition of total lung capacity?
What is the Inspiratory Reserve Volume (IRV)?
What is the Inspiratory Reserve Volume (IRV)?
Which three lung volumes are included in vital capacity?
Which three lung volumes are included in vital capacity?
What lung volumes cannot be determined by spirometry?
What lung volumes cannot be determined by spirometry?
What is the most useful test of gas exchange capacity?
What is the most useful test of gas exchange capacity?
What does DLCO (diffusion capacity of the lungs for carbon monoxide) correlate with?
What does DLCO (diffusion capacity of the lungs for carbon monoxide) correlate with?
Why is the DLCO test useful in respiratory assessment?
Why is the DLCO test useful in respiratory assessment?
6 minute walk test correlates with VO2 max
6 minute walk test correlates with VO2 max
The ability to climb 5 flights of stairs is approximately VO2 max > 20
The ability to climb 5 flights of stairs is approximately VO2 max > 20
What are the common symptoms of an Upper Respiratory Infection (URI)?
What are the common symptoms of an Upper Respiratory Infection (URI)?
Bacterial URIs produce more serious symptoms
Bacterial URIs produce more serious symptoms
Diagnosis of URIs are usually based on cultures and labs tests
Diagnosis of URIs are usually based on cultures and labs tests
Children with URIs are at an increased risk of which respiratory complications?
Children with URIs are at an increased risk of which respiratory complications?
What effects do surgery and anesthesia have on the immune system?
What effects do surgery and anesthesia have on the immune system?
What is the preferred airway management technique when a patient has an upper respiratory tract infection (URI)?
What is the preferred airway management technique when a patient has an upper respiratory tract infection (URI)?
What is COPD?
What is COPD?
What are some common causes of Chronic Obstructive Pulmonary Disease (COPD)?
What are some common causes of Chronic Obstructive Pulmonary Disease (COPD)?
What differentiates asthma from COPD?
What differentiates asthma from COPD?
Are patients with mild well-controlled asthma at an increased perioperative risk?
Are patients with mild well-controlled asthma at an increased perioperative risk?
During assessment, asthma patients should be queried about:
During assessment, asthma patients should be queried about:
In asthma patients, what can ET intubation cause?
In asthma patients, what can ET intubation cause?
How is the severity of COPD typically measured?
How is the severity of COPD typically measured?
What FEV1/FVC ratio is needed to be diagnosed with COPD?
What FEV1/FVC ratio is needed to be diagnosed with COPD?
At which FEV1/FVC ratio is moderate COPD graded?
At which FEV1/FVC ratio is moderate COPD graded?
What is the FEV1/FVC ratio?
What is the FEV1/FVC ratio?
How does COPD affect FEV1?
How does COPD affect FEV1?
How does COPD affect FRC (Functional Residual Capacity)?
How does COPD affect FRC (Functional Residual Capacity)?
What is the DLC0 in COPD?
What is the DLC0 in COPD?
Is a chest x-ray useful for the routine assessment of asthma and COPD patients?
Is a chest x-ray useful for the routine assessment of asthma and COPD patients?
Is it true that pulmonary hypertension medications should be continued on the day of surgery?
Is it true that pulmonary hypertension medications should be continued on the day of surgery?
What pulmonary changes are present in restrictive lung disease?
What pulmonary changes are present in restrictive lung disease?
What pulmonary symptoms are typically present in obstructive lung disease?
What pulmonary symptoms are typically present in obstructive lung disease?
What are the FEV1 and FVC in restrictive lung disease?
What are the FEV1 and FVC in restrictive lung disease?
The FEV1/FVC ratio in restrictive lung disease is increased
The FEV1/FVC ratio in restrictive lung disease is increased
How many bronchi does the right upper lobe bronchus typically give off?
How many bronchi does the right upper lobe bronchus typically give off?
You can measure RV using a spirometer
You can measure RV using a spirometer
Is obesity the most common restrictive lung disease?
Is obesity the most common restrictive lung disease?
The decreased in FRC in obese patients also decreases the tendency to desaturate during anesthesia procedures
The decreased in FRC in obese patients also decreases the tendency to desaturate during anesthesia procedures
What should be the goal of all interventions used during anesthesia procedures with obese patients?
What should be the goal of all interventions used during anesthesia procedures with obese patients?
What is the functional residual capacity (FRC)?
What is the functional residual capacity (FRC)?
How is the severity of Obstructive Sleep Apnea (OSA) typically measured?
How is the severity of Obstructive Sleep Apnea (OSA) typically measured?
What is the defining feature of the upper airway in obstructive sleep apnea (OSA)?
What is the defining feature of the upper airway in obstructive sleep apnea (OSA)?
What is used preoperatively to assess OSA (obstructive sleep apnea)?
What is used preoperatively to assess OSA (obstructive sleep apnea)?
OSA patients tolerate the respiratory depressant effects of opioids due to their tolerance of hypoxia
OSA patients tolerate the respiratory depressant effects of opioids due to their tolerance of hypoxia
Patients with pulmonary hypertension have a high rate of perioperative morbidity and mortality
Patients with pulmonary hypertension have a high rate of perioperative morbidity and mortality
Moderate to severe pulmonary hypertension increases the risk of which disease?
Moderate to severe pulmonary hypertension increases the risk of which disease?
Pulmonary hypertension causes a decreased sympathetic tone
Pulmonary hypertension causes a decreased sympathetic tone
Is opioid administration well tolerated in patients with cor pulmonale?
Is opioid administration well tolerated in patients with cor pulmonale?
What is a common cause of pulmonary hypertension?
What is a common cause of pulmonary hypertension?
In pulmonary hypertension, syncopal episodes indicate what about the disease progression?
In pulmonary hypertension, syncopal episodes indicate what about the disease progression?
What are the common signs and symptoms of pulmonary hypertension?
What are the common signs and symptoms of pulmonary hypertension?
What is unique about heart sounds in pulmonary hypertension?
What is unique about heart sounds in pulmonary hypertension?
What type of murmur may be heard in pulmonary hypertension?
What type of murmur may be heard in pulmonary hypertension?
What EKG changes are present in pulmonary hypertension?
What EKG changes are present in pulmonary hypertension?
Mild pulmonary hypertension does not influence anesthetic management
Mild pulmonary hypertension does not influence anesthetic management
Consulting with a patient's pulmonologist preoperatively is not necessary unless the patient has severe pulmonary hypertension
Consulting with a patient's pulmonologist preoperatively is not necessary unless the patient has severe pulmonary hypertension
What is the effect of smoking on coronary blood flow?
What is the effect of smoking on coronary blood flow?
What is the effect of smoking on macrophage function?
What is the effect of smoking on macrophage function?
What is the mechanism by which vascular relaxation occurs after the cessation of smoking?
What is the mechanism by which vascular relaxation occurs after the cessation of smoking?
What are some risks of pulmonary complications during surgery?
What are some risks of pulmonary complications during surgery?
How do you calculate BMI?
How do you calculate BMI?
Can chronic dyspnea of unclear etiology usually be attributed to asthma, COPD, interstitial lung disease, or cardiac dysfunction?
Can chronic dyspnea of unclear etiology usually be attributed to asthma, COPD, interstitial lung disease, or cardiac dysfunction?
What can increase the risk of right heart failure in a pulmonary hypertension patient?
What can increase the risk of right heart failure in a pulmonary hypertension patient?
What does FEV1 represent in respiratory assessment?
What does FEV1 represent in respiratory assessment?
What is FVC?
What is FVC?
Wheezing is specific to asthma
Wheezing is specific to asthma
What cartilage does the trachea originate from?
What cartilage does the trachea originate from?
LMA is preferred in instances of high risk of broncho or laryngospasm
LMA is preferred in instances of high risk of broncho or laryngospasm
Resistance = 8 * length * viscosity / (pi*r^4)
Resistance = 8 * length * viscosity / (pi*r^4)
Study Notes
Respiratory Assessment
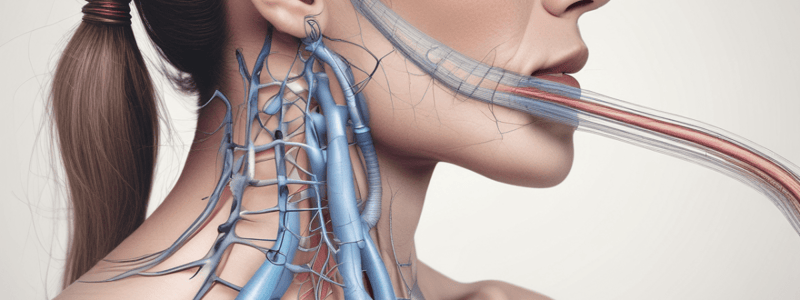
- The upper airway has three main functions: conduit for inhalation and exhalation of air, warming and humidification of inspired gases, and tissue hydration and trapping of pathogens via mucous membranes.
Airway Resistance
- Airway resistance is affected by laminar flow (smooth, efficient gas exchange) and turbulent flow (chaotic, trapping inhaled particulate matter).
- Reynold's number determines whether flow is laminar or turbulent.
Trachea and Bronchi
- The trachea terminates at the carina (bifurcation).
- The right upper bronchus gives off three segmental bronchi.
Airways and Cartilage
- Airways lose all cartilage at the level of bronchioles.
Alveolar Cells and Functions
- There are three types of alveolar cells: Type 1 (squamous epithelial, for gas exchange), Type 2 (produce surfactant), and Alveolar macrophages (phagocytize foreign objects).
Functional Assessment of Respiratory System
- Functional assessment should include evaluation of three functions: respiratory mechanics, gas exchange, and cardiopulmonary interaction.
Lung Capacities and Volumes
- FRC (functional residual capacity) is the volume after normal exhalation.
- TLC (total lung capacity) is the sum of IRV, TV, and FRC.
- RV (residual volume) is the volume of air to keep lungs inflated.
- VC (vital capacity) includes inspiratory reserve volume, TV, and expiratory reserve volume.
Diffusion Capacity and CO
- Diffusion capacity for carbon monoxide (CO) is the most useful test of alveolar gas exchange.
- CO has high affinity for Hgb, following the same path as oxygen to bind with hemoglobin.
Post-Thoracotomy Patients
- Patients are at risk for poorer post-thoracotomy outcomes if their VO2 max is < 15 mL/kg/min.
- The 6-minute walk test correlates well with VO2 max.
Upper Respiratory Infection
- 95% of URIs are due to viral or bacterial nasopharyngitis.
- Symptoms include non-productive cough, sneezing, and rhinorrhea.
- Four risk factors associated with URI that increase the frequency of adverse events under anesthesia: fever, purulent rhinitis, productive cough, and rhonchi.
Asthma
- Asthma is characterized by chronic airway inflammation, variable expiratory airflow limitation, SOB, chest tightness, and cough.
- Three classes of medications an asthma patient may be taking: inhaled/oral steroids, beta2 agonists, and antibiotics.
COPD
- Five exposures likely to be associated with provoking COPD: smoking, environmental pollutants, chronic infections, longstanding asthma, and alpha1 antitrypsin deficiency.
- Measures to assess severity of COPD include spirometry and lung volumes.
Obstructive Sleep Apnea
- Risk factors for OSA: snoring, daytime sleepiness, hypertension, obesity, and family history.
- The Apnea-Hypopnea Index measures the number of apneic-hypopneic episodes per hour of sleep.
- Three airway management tasks that may be more difficult in OSA patients: mask ventilation, direct laryngoscopy, and ET placement.
Pulmonary Hypertension
- Pulmonary hypertension is defined by mean PAP >25 mmHg or PAOP >15 mmHg.
- Five events that can increase the risk of right heart failure in PH patients: hypoxia, hypercarbia, administration of vasoconstrictors, increased sympathetic tone, and increased PVR.
Tobacco Smoking
- Five complications of tobacco smoking: decreased macrophage function, impairment of coronary blood flow, vascular endothelial dysfunction, hypertension, and respiratory complications.
- Ideally, cessation of smoking should occur 3-4 weeks prior to surgery.
- Four benefits of smoking cessation: lowered CO levels, levels of toxic substances, cyanide levels, and vascular relaxation.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.