Podcast
Questions and Answers
What is the primary lymphatic drainage route after leaving the renal hilum?
What is the primary lymphatic drainage route after leaving the renal hilum?
- To the left lateral aortic lymph nodes (correct)
- Directly to the thoracic duct
- To the right suprarenal lymph nodes
- To the lumbar lymph nodes
Which structures are involved in the lymphatic drainage mentioned?
Which structures are involved in the lymphatic drainage mentioned?
- Celiac trunk and superior mesenteric artery
- Inferior mesenteric artery and diaphragm (correct)
- Ureter and bladder
- Renal artery and renal vein
Which lymph nodes are specifically noted for draining lymph from the left kidney?
Which lymph nodes are specifically noted for draining lymph from the left kidney?
- Celiac lymph nodes
- Right lateral aortic nodes
- Right renal nodes
- Left lateral aortic nodes (correct)
What anatomical location lies between the inferior mesenteric artery and the diaphragm?
What anatomical location lies between the inferior mesenteric artery and the diaphragm?
What role does the renal hilum play in the lymphatic drainage of the left kidney?
What role does the renal hilum play in the lymphatic drainage of the left kidney?
What is the primary functional unit of the kidneys responsible for filtration and urine formation?
What is the primary functional unit of the kidneys responsible for filtration and urine formation?
Which part of the nephron includes the Glomerular (Bowman's) capsule?
Which part of the nephron includes the Glomerular (Bowman's) capsule?
Which structure directly drains lymph from the right side of the body?
Which structure directly drains lymph from the right side of the body?
What is the primary function of the renal cortex?
What is the primary function of the renal cortex?
Why is the left renal vein longer than the right renal vein?
Why is the left renal vein longer than the right renal vein?
Which part of the nephron is responsible for carrying urine to the collecting system?
Which part of the nephron is responsible for carrying urine to the collecting system?
Which vein does the left gonadal vein typically drain into?
Which vein does the left gonadal vein typically drain into?
How does renal lymphatic drainage relate to the venous system?
How does renal lymphatic drainage relate to the venous system?
Where do the left suprarenal veins typically drain?
Where do the left suprarenal veins typically drain?
What is the significance of the renal hilum in relation to vascular supply?
What is the significance of the renal hilum in relation to vascular supply?
Flashcards
Left Renal Lymph Drainage
Left Renal Lymph Drainage
The left primary lymphatic vessels drain into the left lateral aortic lymph nodes located between the inferior mesenteric artery and the diaphragm.
Left Lateral Aortic Lymph Nodes
Left Lateral Aortic Lymph Nodes
Lymph nodes positioned along the left side of the aorta. These nodes receive lymphatic fluid from the left kidney and surrounding areas.
Inferior Mesenteric Artery (IMA)
Inferior Mesenteric Artery (IMA)
An artery that branches off the abdominal aorta and supplies blood to the lower part of the digestive tract.
Renal Hilum
Renal Hilum
Signup and view all the flashcards
Lymphatic Drainage
Lymphatic Drainage
Signup and view all the flashcards
Left Renal Vein
Left Renal Vein
Signup and view all the flashcards
Right Renal Vein
Right Renal Vein
Signup and view all the flashcards
Left Gonadal Vein Drainage
Left Gonadal Vein Drainage
Signup and view all the flashcards
Left Suprarenal Vein Drainage
Left Suprarenal Vein Drainage
Signup and view all the flashcards
Lymphatic Drainage Parallels Venous Drainage
Lymphatic Drainage Parallels Venous Drainage
Signup and view all the flashcards
What are nephrons?
What are nephrons?
Signup and view all the flashcards
Renal corpuscle structure
Renal corpuscle structure
Signup and view all the flashcards
Glomerulus
Glomerulus
Signup and view all the flashcards
Renal Tubule
Renal Tubule
Signup and view all the flashcards
Collecting System
Collecting System
Signup and view all the flashcards
Study Notes
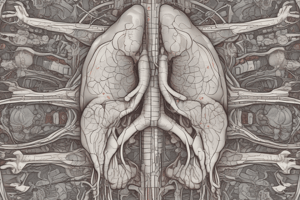
Renal Anatomy (Kidney)
- Kidneys are retroperitoneal structures, meaning their posterior surface is not covered by the peritoneum.
- Typical kidney weighs approximately 150 grams and is 12 cm long, 6 cm wide, and 3 cm thick.
- Located on the posterior abdominal wall, extending from the upper border of T12 to L3 vertebra.
- Right kidney is slightly lower than the left due to the liver.
- The hilum is the indented area on the medial surface where renal vessels and the ureter enter and exit the kidney.
- The hilum is directed medially.
- The renal vessels (artery and vein) are anterior to the ureter.
- The ureter is directed downwards.
- The kidney is divided into superficial cortex and inner medulla.
Kidney Structure
- The medulla contains the renal pyramids, triangular structures whose bases face the cortex and whose tips (renal papillae) project into the renal sinus.
- Renal columns are bands of cortical tissue that separate adjacent renal pyramids.
- The cortex surrounds the medulla.
Kidney Parts
- Upper pole: The superior end of the kidney.
- Lower pole: The inferior end of the kidney.
- Lateral border: The outer edge of the kidney.
- Medial border: The inner edge of the kidney, containing the hilum.
- Anterior surface: The front-facing side of the kidney.
- Posterior surface: The back-facing side of the kidney.
Kidney Functions
- Filtration and excretion of metabolic waste products (e.g., urea, ammonium).
- Regulation of essential electrolytes, fluid, and acid-base balance.
- Stimulation of red blood cell production.
- Regulation of blood pressure via the renin-angiotensin-aldosterone system.
- Reabsorption of water and maintenance of intravascular volume.
- Reabsorption of glucose and amino acids.
- Hormonal functions involving erythropoietin, calcitriol, and vitamin D activation.
Renal Segments
- The kidney is subdivided into segments based on its vascular pattern.
- Apical, inferior, superior, and middle segments are present on both anterior and posterior surfaces of the kidneys.
Renal Vessels
- Renal arteries supply blood to the kidneys arising from the abdominal aorta at the level of L2.
- The renal artery branches into segmental arteries which supplies most of the posterior kidney with some exception of the lower pole.
- Anterior branches of the renal artery are superior, anterior superior, and anterior inferior segmental arteries.
- Renal veins drain the kidneys, similar to the arteries, and are generally located anterior to the renal arteries.
- The left renal vein is longer than the right as it crosses the midline to reach the inferior vena cava(IVC).
Kidney Covering and Support
- Renal fascia: A dense fibrous outer capsule that anchors the kidney to surrounding structures.
- Perinephric fat: A layer of adipose tissue that cushions and protects the kidney.
- Four layers: fibrous capsule, perinephric fat, renal fascia, subdiaphragmatic fascia.
- True capsule: innermost
Renal Lymphatic Drainage
- The lymphatic drainage of the kidneys follows the venous drainage pattern.
- The left kidney drains into the left lateral aortic lymph nodes.
- The right kidney drains into the right lateral caval lymph nodes.
Nephron
- Nephrons are the microscopic functional units of the kidneys.
- Each nephron consists of a renal corpuscle and a renal tubule.
- Renal corpuscle: Spherical structure consisting of the Bowman's capsule and the glomerulus.
- Glomerulus: A cluster of capillaries where filtration takes place.
Renal Tubule
- Proximal convoluted tubule (PCT): First segment of the renal tubule, characterized by simple cuboidal epithelium and microvilli. Absorbs ions, water, and nutrients.
- Loop of Henle: U-shaped structure extending into the medulla. Has descending and ascending limbs, each with differing epithelial characteristics.
- Distal convoluted tubule (DCT): Smaller than the PCT, lacking microvilli. Involved in reabsorption and secretion.
- Collecting ducts: Receive fluid from multiple nephrons and carry it to the minor calyxes.
Juxtaglomerular Complex
- Consists of the macula densa, juxtaglomerular cells, and extraglomerular mesangial cells.
- Functions in regulating blood pressure and electrolyte balance.
Collecting System
- A series of tubes (collecting ducts) that carry tubular fluid away from nephrons to the kidney pelvis.
- Receives fluid from multiple nephrons and carries it toward the renal pelvis.
Renal Cortex
- The superficial region of the kidney in contact with the fibrous capsule.
- Reddish-brown, granular appearance.
- Contains renal pyramids (6-18).
Renal Columns
- Bands of cortical tissue that separate adjacent renal pyramids.
- Extends into the medulla, containing ducts that discharge urine into the minor calyces.
Major Calyx
- Formed by four or five minor calyxes, funnel-like structure.
- Connected to the ureter, which carries urine from the kidney to the bladder.
Clinical Importance of Renal Fascia
- Sudden weight loss may cause kidney descent (ptosis).
- Pus around the kidney spreads downwards due to loose areolar connective tissue.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.