Podcast
Questions and Answers
What is the primary role of chemoreceptors in cardiovascular regulation?
What is the primary role of chemoreceptors in cardiovascular regulation?
- Regulate the release of hormones
- Detect changes in heart rate
- Monitor chemical changes in blood (correct)
- Monitor blood pressure changes
Which of the following substances decreases cardiac activity?
Which of the following substances decreases cardiac activity?
- Thyroid hormones
- Hypoxia (correct)
- Calcium
- Adrenaline
How do adrenaline and noradrenaline affect heart function?
How do adrenaline and noradrenaline affect heart function?
- They exclusively influence blood chemistry
- They enhance efficiency and increase heart rate (correct)
- They stabilize blood pressure without affecting heart rate
- They lower heart rate and reduce contractility
What type of receptor is primarily responsible for detecting changes in blood pressure?
What type of receptor is primarily responsible for detecting changes in blood pressure?
What effect do moderate increases in calcium ions have on heart rate?
What effect do moderate increases in calcium ions have on heart rate?
What role do positive inotropic agents play in heart function?
What role do positive inotropic agents play in heart function?
Which neurotransmitter is primarily associated with sympathetic stimulation of the heart?
Which neurotransmitter is primarily associated with sympathetic stimulation of the heart?
How does the autonomic nervous system regulate heart rate?
How does the autonomic nervous system regulate heart rate?
What is the effect of glucagon on the heart?
What is the effect of glucagon on the heart?
What is the impact of increased extracellular K+ concentration on cardiac muscle?
What is the impact of increased extracellular K+ concentration on cardiac muscle?
What is the function of receptors activated by adrenergic hormones like adrenaline?
What is the function of receptors activated by adrenergic hormones like adrenaline?
What effect does anoxia have on cardiac function?
What effect does anoxia have on cardiac function?
Which drug is known for its positive inotropic effects by blocking calcium flux out of sarcoplasm?
Which drug is known for its positive inotropic effects by blocking calcium flux out of sarcoplasm?
What effect does noradrenaline have on cardiac output?
What effect does noradrenaline have on cardiac output?
Which hormone is primarily responsible for causes vasodilation?
Which hormone is primarily responsible for causes vasodilation?
Which factor does NOT influence resistance to blood flow?
Which factor does NOT influence resistance to blood flow?
What is the primary effect of aldosterone on blood pressure?
What is the primary effect of aldosterone on blood pressure?
Which of the following hormones does NOT lead to vasoconstriction?
Which of the following hormones does NOT lead to vasoconstriction?
How does increased blood viscosity affect blood flow?
How does increased blood viscosity affect blood flow?
What role does angiotensin II play in blood pressure regulation?
What role does angiotensin II play in blood pressure regulation?
What is hydrostatic pressure in the context of blood flow?
What is hydrostatic pressure in the context of blood flow?
Which of these hormones primarily causes an increase in heart rate?
Which of these hormones primarily causes an increase in heart rate?
What effect does atrial natriuretic peptide have on blood pressure?
What effect does atrial natriuretic peptide have on blood pressure?
Flashcards are hidden until you start studying
Study Notes
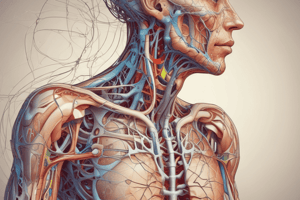
Regulation of Heart Rate
- Increased input to cardiovascular center: Happens upon movement, this is a significant stimulus for rapid heart rate increase at the start of physical activity.
- Chemoreceptors: Monitor chemical changes in the blood.
- Baroreceptors: Monitor blood pressure in major arteries and veins.
- Located in the aortic arch and carotid arteries.
- Detect blood pressure changes, influencing blood pressure and heart rate.
- Chemical Regulation:
- Depression of cardiac activity:
- Hypoxia (low oxygen levels).
- Acidosis (low pH).
- Alkalosis (high pH).
- Major effects on the heart:
- Hormones:
- Adrenaline (E) and noradrenaline (NE): (both from adrenal medulla) enhance heart efficiency.
- E and NE increase heart rate (HR) and contractility.
- Thyroid hormones also enhance HR and contractility.
- Ions:
- Relative concentrations of K+, Na+, and Ca2+ have a major impact on cardiac function.
- Excess K+ and Na+ have negative effects.
- Moderate increases in Ca2+ speed HR.
- Hormones:
- Depression of cardiac activity:
- Nervous System Control of the Heart
- Higher Brain Centers:
- Sensory receptors
- Cerebral Cortex
- Limbic System
- Hypothalamus
- Proprioceptors: Monitor limb and muscle position.
- Chemoreceptors: Monitor blood chemistry.
- Baroreceptors: Monitor blood pressure.
- Higher Brain Centers:
Contractility
- The forcefulness of contraction of individual ventricular muscle fibers.
- The strength of contraction for any given preload.
- Regulated by:
- Positive inotropic agents: Increase contractility.
- Negative inotropic agents: Decrease contractility.
Afterload
- The pressure that must be exceeded before blood ejection from ventricles can begin.
- It’s the pressure needed to force open semilunar valves.
- When increased (e.g., elevated blood pressure, atherosclerosis), stroke volume decreases, and more blood remains in the ventricles at the end of systole.
Positive Inotropic Agents (Regulation of Stroke Volume)
- Often promote Ca2+ influx during cardiac action potentials, strengthening muscle fiber contraction force.
- Types:
- Sympathetic stimulation:
- Noradrenaline (NE) released from postganglionic fibers binds receptors on cardiac muscle cell membrane.
- Adrenaline (E) and NE released from adrenal medulla bind receptors on cardiac muscle cell membrane.
- Stimulation of cardiac muscle metabolism.
- Hormones:
- Adrenaline (E) and noradrenaline (NE).
- Glucagon.
- Thyroid hormones.
- Increased extracellular Ca2+ concentration.
- Drugs:
- Isoproterenol, dopamine, and dobutamine: (via α- and β-receptor-mediated effects).
- Digitalis: (via blocking Ca2+ flux out of sarcoplasm).
- Sympathetic stimulation:
Negative Inotropic Agents (Regulation of Stroke Volume)
- Types:
- Sympathetic inhibition:
- Acetylcholine (ACh) released from the vagus nerve binds receptors and hyperpolarizes the cardiac muscle cell membrane.
- Decreased heart rate (via effects on SA and AV nodes).
- Reduced force of contraction.
- Anoxia (oxygen deficiency).
- Acidosis (low pH).
- Increased extracellular K+ concentration.
- Drugs:
- Propanolol, artenolol, and barbiturates: (via α- and β-receptor-mediated effects).
- Anaesthetics (e.g., halothane): via reduced intracellular Ca2+.
- Sympathetic inhibition:
Regulation of Heart Rate: Autonomic Innervation
- Cardiovascular center:
- Processes nerve impulses (input) to deliver specific responses (output) via sympathetic and parasympathetic nerves.
- Proprioceptors: Monitor limb and muscle position.
Hormonal Regulation of Blood Pressure
- Factor influencing blood pressure | Hormone | Effect on blood pressure
- Increased heart rate and force of contraction | Noradrenaline | Increase
- Vasoconstriction | Angiotensin II | Increase
- Vasoconstriction | Antidiuretic hormone | Increase
- Vasoconstriction | Noradrenaline | Increase
- Vasoconstriction | Adrenaline | Increase
- Vasoconstriction | Calcitriol (active form of vitamin D) | Increase
- Vasodilation | Atrial natriuretic peptide | Decrease
- Vasodilation | Adrenaline | Decrease
- Vasodilation | Parathyroid hormone | Decrease
- Blood volume increase | Aldosterone | Increase
- Blood volume increase | Antidiuretic hormone | Increase
- Blood Volume decrease | Atrial natriuretic peptide | Decrease
Other Key Points
- Blood flow depends on the heart to maintain a pressure head.
- Hydrostatic pressure: Force exerted in all directions when a fluid is not moving.
- Resistance to blood flow depends on:
- Total blood vessel length
- Blood viscosity
- Turbulence
- Average blood vessel radius
- Increased | Increased | Increased | Increased total blood vessel radius (vasoconstriction)
- Heart rate | Stroke volume (preload) | Blood viscosity | Increased vessel length
- Increased cardiac output | Increased systemic vascular resistance | Increased mean arterial pressure (MABP)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.