Podcast
Questions and Answers
Why does the mucosa appear white in color?
Why does the mucosa appear white in color?
Increased production of keratin, abnormal but benign thickening of stratum spinosum, intra and extracellular accumulation of fluid in the epithelium, or fungi producing white pseudomembranes.
Why does the mucosa appear red in color?
Why does the mucosa appear red in color?
Atrophy of the epithelium, reduction in the number of epithelial cells.
What is the common lesion associated with frictional irritation, pressure, or sucking trauma from facial surfaces of the teeth?
What is the common lesion associated with frictional irritation, pressure, or sucking trauma from facial surfaces of the teeth?
- Linea alba (correct)
- Morsicatio mucosae oris
- Thermal burn
- Chemical burn
What is the common site of Thermal burn?
What is the common site of Thermal burn?
What is Morsicatio mucosae oris?
What is Morsicatio mucosae oris?
What is the treatment for Thermal burn?
What is the treatment for Thermal burn?
What is the risk associated with the use of electronic cigarettes?
What is the risk associated with the use of electronic cigarettes?
What is the treatment for Electronic cigarette burns?
What is the treatment for Electronic cigarette burns?
What is the recommended treatment regimen for oral candidiasis using Nystatin oral suspension?
What is the recommended treatment regimen for oral candidiasis using Nystatin oral suspension?
Which medication for angular cheilitis requires to be applied to the corners of the mouth three times a day?
Which medication for angular cheilitis requires to be applied to the corners of the mouth three times a day?
Submucosal hemorrhage is commonly characterized by blanching lesions.
Submucosal hemorrhage is commonly characterized by blanching lesions.
What is the best treatment for chemical burns according to the text?
What is the best treatment for chemical burns according to the text?
What are some common factors associated with hairy tongue? Select all that apply.
What are some common factors associated with hairy tongue? Select all that apply.
Angular cheilitis is commonly seen in younger patients.
Angular cheilitis is commonly seen in younger patients.
What can coated tongue be mistaken for? It may be mistaken for __________.
What can coated tongue be mistaken for? It may be mistaken for __________.
Match the drug with its application method according to the text:
Match the drug with its application method according to the text:
Flashcards are hidden until you start studying
Study Notes
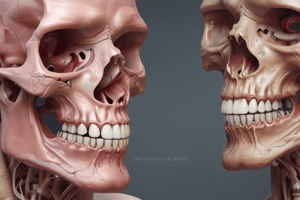
Red and White Lesions
- Causes of white mucosa:
- Hyperkeratosis (increased keratin production)
- Acanthosis (abnormal thickening of stratum spinosum)
- Intra- and extracellular fluid accumulation in epithelium
- Fungal pseudomembranes
- Causes of red mucosa:
- Atrophy of epithelium (decrease in cell size)
- Reduction in number of epithelial cells
Developmental, Hereditary, and Congenital Lesions
- White lesions:
- White sponge nevus
- Leukoedema
- Hereditary benign intraepithelial dyskeratosis
- Red lesions:
- Hemangioma
- Red and white lesions:
- Oral lichen planus
- Erythema migrans/geographic tongue
Linea Alba
- Common lesion
- Caused by frictional irritation, pressure or sucking trauma
- Presents as a linear white lesion, usually bilateral on buccal mucosa along occlusal plane
- No need for biopsy or treatment, may show spontaneous regression
Morsicatio Mucosae Oris
- Caused by chronic chewing
- Presents as thick, shredded, white areas with irregular surface
- May have zones of erythema, erosion, or focal traumatic ulceration
- Common in females, affecting anterior buccal mucosa, lips, and tongue
- No treatment needed, resolves upon habit cessation
Thermal Burn
- Caused by ingestion of hot foods or beverages
- Presents as sloughing white lesion, red-white lesion, or red lesion
- May show zones of erythema and ulceration
- Commonly affects palate or posterior buccal mucosa
- Most cases resolve without treatment, corticosteroids and antibiotics used in severe cases
Chemical Burn
- Caused by:
- Aspirin-tablets, powder
- Bisphosphonates
- Psychoactive drugs
- Hydrogen peroxide
- Recreational drugs
- Presents as white, wrinkled plaque or necrotic red, bleeding connective tissue
- May affect any oral mucosal site
- Treatment involves prevention of exposure, sodium hypochlorite irrigation, and debridement
Leukoedema
- Common oral mucosal condition
- Seen in 70-90% of black adults and 50% of black children
- Presents as diffuse gray-white, milky, or opalescent lesion
- Unknown cause, may be developmental in nature
- No treatment required
Candidiasis
- Most common oral fungal infection
- Caused by:
- Local factors (denture wearing, smoking, inhalation steroids)
- General factors (immunosuppressive diseases, impaired health status)
- Presents as:
- Pseudomembranous candidiasis (adherent white plaques)
- Coated tongue (accumulation of bacteria and desquamated epithelial cells)
- Hairy tongue (marked accumulation of keratin on filiform papillae)
Hairy Tongue
- Seen in 0.5-11.3% of adults
- Caused by increase in keratin production or decrease in normal keratin desquamation
- Presents as elongated, yellowish-white or brown filiform papillae on dorsal tongue
- Asymptomatic, eliminate predisposing factors, encourage excellent oral hygiene
Median Rhomboid Glossitis
- Presents as well-demarcated erythematous zone on midline of posterior dorsal tongue
- Erythema due to loss of filiform papillae, often asymmetric and smooth or lobulated
- Often asymptomatic### Denture Stomatitis/Chronic Atrophic Candidiasis
- Most common form of candidiasis in denture patients, usually asymptomatic
- Localized to denture-bearing areas of maxillary removable denture
- Seen when patient wears denture continuously, but must rule out other causes such as improper denture design, allergy to denture base, or inadequate curing of denture acrylic
- Presents with varying degrees of erythema, sometimes accompanied by petechial hemorrhage
- Can be associated with concomitant inflammatory papillary hyperplasia, often secondary to poorly fitting dentures
Angular Cheilitis
- Presents with erythema, fissuring, and scaling of the angles of the mouth
- Commonly seen in older patients with decreased vertical dimension of occlusion and accentuated folds at the corners of the mouth, with pooling of saliva in the corners of the mouth
- The severity of the lesions waxes and wanes
- Caused by 20% Candida albicans, 60% Candida albicans & Staphylococcus aureus, and 20% Staphylococcus aureus
Oral Candidiasis
- Diagnosis involves clinical signs in conjunction with exfoliative cytology
- Cytological findings should demonstrate hyphal phase of the organism
- Cytology is simple, non-invasive, and cost-effective
- Treatment options include:
- Imidazole agents (clotrimazole 1% cream, clotrimazole troches 10 mg)
- Polyene agents (nystatin oral suspension 100,000 units/ml, nystatin pastilles 200,000 units/pastille, nystatin ointment)
- Triazoles (fluconazole)
- Other agents (iodoquinol)
Geographic Tongue (Erythema Migrans, Benign Migratory Glossitis)
- Seen in 1-3% of the population, with unknown etiopathogenesis and female predilection
- Presents as multiple, well-demarcated zones of erythema (atrophy of filiform papillae) surrounded by slightly raised yellow-white serpentine or scalloped border on the dorsal tongue (anterior 2/3rd) and ventrolateral tongue
- Lesions develop quickly, heal in days to weeks, and then develop in a different area; continually changing pattern
- Often associated with fissured tongue (1/3rd of patients)
- May demonstrate burning sensation or sensitivity to hot or spicy foods
- Treatment is not usually indicated, but topical steroids may be used for symptomatic patients
Submucosal Hemorrhage
- Seen when a traumatic event results in hemorrhage and entrapment of blood within tissues
- Terminology depends on the size of hemorrhage:
- Petechiae: minute hemorrhages into skin, mucosa, or serosa
- Purpura: slightly larger area affected (5 mm – 2 cm)
- Ecchymosis: any accumulation greater than 2 cm
- Hematoma: accumulation of blood within tissue producing a mass
- Causes include:
- Trauma (blunt trauma, oral trauma from sexual practices)
- Increased intrathoracic pressure (repeated or prolonged coughing, vomiting, convulsion, or giving birth)
- Non-traumatic causes (anticoagulation therapy, thrombocytopenia, disseminated intravascular coagulation, viral infections)
- Presents as non-blanching lesion, usually flat, except for hematoma (elevated lesion)
- Commonly seen on labial mucosa or buccal mucosa
- No treatment if not associated with morbidity or related to systemic disease, as areas resolve spontaneously
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.