Podcast
Questions and Answers
What is the primary function of the alveolar process?
What is the primary function of the alveolar process?
- To provide osseous attachment to the forming periodontal ligament (correct)
- To produce dental enamel
- To support the roots of the tooth
- To form the sockets of the teeth
What type of bone makes up the alveolar bone proper?
What type of bone makes up the alveolar bone proper?
- Bundle bone and lamellated bone (correct)
- Compact bone
- Spongy bone
- Cancellous bone
What is the characteristic of bundle bone?
What is the characteristic of bundle bone?
- It contains more calcium salts per unit area than other bone (correct)
- It is a type of spongy bone
- It is a type of cortical plate
- It is a type of compact bone
What is the purpose of the supporting alveolar bone?
What is the purpose of the supporting alveolar bone?
What is the characteristic of the cortical plates in the maxilla?
What is the characteristic of the cortical plates in the maxilla?
What is the characteristic of the buccal plates in the mandible?
What is the characteristic of the buccal plates in the mandible?
What is the term for the perforated bone with many small foramina for blood vessels and nerves?
What is the term for the perforated bone with many small foramina for blood vessels and nerves?
What happens to the osteoblasts after moving away from the lamellae?
What happens to the osteoblasts after moving away from the lamellae?
What type of bone formation involves the formation of a cartilagenous model?
What type of bone formation involves the formation of a cartilagenous model?
What surrounds the cartilage in endochondral bone formation?
What surrounds the cartilage in endochondral bone formation?
What is the role of alkaline phosphatase in endochondral bone formation?
What is the role of alkaline phosphatase in endochondral bone formation?
What is the result of the cartilage cells being cut off from nutrition?
What is the result of the cartilage cells being cut off from nutrition?
What invades the calcified matrix in endochondral bone formation?
What invades the calcified matrix in endochondral bone formation?
What happens to the calcified matrix in the formation of secondary areolae?
What happens to the calcified matrix in the formation of secondary areolae?
What is the function of the Haversian system?
What is the function of the Haversian system?
What type of lamellae forms the outer surface of the bone?
What type of lamellae forms the outer surface of the bone?
What is the function of the periosteum?
What is the function of the periosteum?
What is the structural and metabolic unit of the lamellar bone?
What is the structural and metabolic unit of the lamellar bone?
What type of bone marrow is mainly found in the embryo and newborn?
What type of bone marrow is mainly found in the embryo and newborn?
What is the function of the osteoblasts?
What is the function of the osteoblasts?
What fills the space between adjacent concentric lamellae?
What fills the space between adjacent concentric lamellae?
What is the function of osteoclasts in bone?
What is the function of osteoclasts in bone?
What percentage of bone composition is made up of inorganic components?
What percentage of bone composition is made up of inorganic components?
What is the term for isolated areas in which the root is denuded of bone and the root surface is covered only by periosteum and overlying gingiva?
What is the term for isolated areas in which the root is denuded of bone and the root surface is covered only by periosteum and overlying gingiva?
What is the predisposing factor for fenestrations and dehiscences?
What is the predisposing factor for fenestrations and dehiscences?
What is the term for the replacement of old bone by new bone?
What is the term for the replacement of old bone by new bone?
What type of protein is found in bone composition?
What type of protein is found in bone composition?
What is the location of osteoclasts in bone?
What is the location of osteoclasts in bone?
What is the characteristic of bone remodeling during childhood?
What is the characteristic of bone remodeling during childhood?
What is the primary function of parathyroid hormone in bone remodeling?
What is the primary function of parathyroid hormone in bone remodeling?
What is the purpose of the proton pump in bone resorption?
What is the purpose of the proton pump in bone resorption?
What type of lines do remodeled alveolar bone show when stained?
What type of lines do remodeled alveolar bone show when stained?
What is the sequence of events in bone resorption?
What is the sequence of events in bone resorption?
What is the function of acid phosphatase and cathepsin B in bone resorption?
What is the function of acid phosphatase and cathepsin B in bone resorption?
What is the characteristic of resting lines in bone remodeling?
What is the characteristic of resting lines in bone remodeling?
What is the primary function of vitamin D3 in bone remodeling?
What is the primary function of vitamin D3 in bone remodeling?
What is the characteristic of reversal lines in bone remodeling?
What is the characteristic of reversal lines in bone remodeling?
What is the influence of age on bone cells in bone remodeling?
What is the influence of age on bone cells in bone remodeling?
Flashcards
Bone Growth
Bone Growth
Bone growth is rapid in childhood, slows in young adulthood, and continues through life, influenced by local functions, age-related changes in bone cells, and systemic factors like hormones and vitamin D.
Bone Turnover
Bone Turnover
The process of breaking down old bone and replacing it with new bone.
Osteoclasts
Osteoclasts
Bone cells that break down (resorb) bone.
Howship's Lacunae
Howship's Lacunae
Signup and view all the flashcards
Endochondral Bone Formation
Endochondral Bone Formation
Signup and view all the flashcards
Bone Composition
Bone Composition
Signup and view all the flashcards
Bone Remodeling Steps
Bone Remodeling Steps
Signup and view all the flashcards
Alveolar Process
Alveolar Process
Signup and view all the flashcards
Alveolar Bone Proper
Alveolar Bone Proper
Signup and view all the flashcards
Supporting Alveolar Bone
Supporting Alveolar Bone
Signup and view all the flashcards
Bundle Bone
Bundle Bone
Signup and view all the flashcards
Lamellar Bone
Lamellar Bone
Signup and view all the flashcards
Osteon
Osteon
Signup and view all the flashcards
Periosteum
Periosteum
Signup and view all the flashcards
Fenestration
Fenestration
Signup and view all the flashcards
Dehiscence
Dehiscence
Signup and view all the flashcards
Haversian System
Haversian System
Signup and view all the flashcards
Lamellae
Lamellae
Signup and view all the flashcards
Study Notes
Bone Development and Remodeling
- Bone growth is rapid during childhood, slow in young adulthood, and continuous throughout life
- Influencing factors: local functional requirements, age-related changes in bone cells, systemic factors (parathyroid hormone, calcitonin, vitamin D3)
Bone Turnover (Remodeling)
- Process of replacing old bone with new bone
- Involves sequences of resorptive events:
- Attachment of osteoclasts to mineralized surface of bone
- Creation of acidic microenvironment, demineralization, and degradation of organic matrix
- Secretion of new osteoid layer and calcification
- Results in formation of resting lines (hypocalcified lines representing phasic formation of bone) and reversal lines (hypocalcified lines marking change from bone resorption to deposition)
Endochondral Bone Formation
- Type of bone formation involving cartilaginous model replacement
- Mesenchymal cells condense, differentiate into chondroblasts, and lay down hyaline cartilage
- Cartilage is surrounded by perichondrium (highly vascular and containing osteogenic cells)
- Cartilage calcification, death of cartilage cells, and invasion by blood vessels and osteogenic cells
- Formation of primary and secondary areolae
Osteoclasts
- Found against the surface of calcified matrix in shallow depressions called Howship's lacunae
- Function: degradation of bone causing resorption
- Secrete enzymes (e.g., tartrate-resistant acid phosphatase) against mineral substrate
Bone Composition
- 67% inorganic hydroxyapatite crystals, calcium phosphate, and other minerals
- 33% organic components (non-collagenous proteins, osteocalcin, osteonectin, phosphoproteins, and collagen type I)
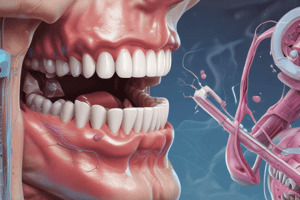
Fenestrations and Dehiscences
- Isolated areas where root is denuded of bone and covered only by periosteum and overlying gingiva (fenestrations)
- Defect extending through marginal bone (dehiscence)
- Etiology unknown; predisposing factors: prominent root contour, malposition, labial portion of root, and thin bony plate
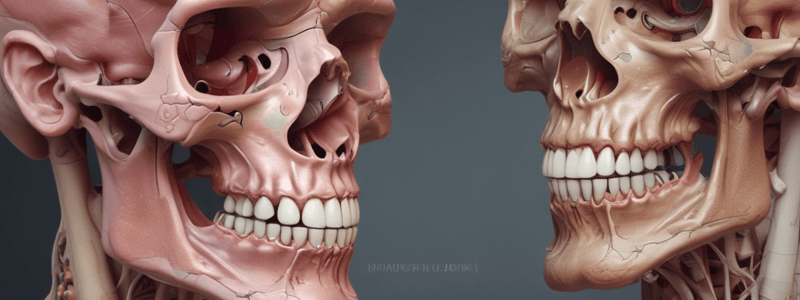
Alveolar Process
- Defined as parts of maxilla and mandible that form and support tooth sockets
- Forms when tooth erupts, providing osseous attachment to periodontal ligament; disappears after tooth loss
Alveolar Bone Proper
- Surrounded by roots of tooth, giving attachment to principal fibers of periodontal ligament
- Histologically composed of bundle bone and lamellar bone
- Bundle bone: bone lining socket with Sharpey's fibers embedded; also called cribriform plate
- Lamellated bone: compact, with haversian system
Supporting Alveolar Bone
- Surrounds alveolar bone proper, providing support to socket
- Consists of cortical plates and spongy bone (cancellous bone)
Microscopic Structure of Bone
- Periosteum: thin connective tissue membrane covering compact bone, rich in blood vessels and nerves
- Osteon: structural and metabolic unit of lamellar bone, consisting of haversian canal and concentric, mineralized lamellae
- Haversian system: haversian canal and Volkmann's canal, providing nutrition to bone
- Lamellae: made up of osteocytes within lacunae; types include circumferential, concentric, and interstitial lamellae
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.