Podcast
Questions and Answers
Which type of alveolar cell is responsible for producing surfactant to lower surface tension and facilitate gas exchange?
Which type of alveolar cell is responsible for producing surfactant to lower surface tension and facilitate gas exchange?
What physiological process is directly initiated by cough receptors located in the carina?
What physiological process is directly initiated by cough receptors located in the carina?
What is the primary function of the mucociliary clearance mechanism in the respiratory system?
What is the primary function of the mucociliary clearance mechanism in the respiratory system?
Which of the following factors would directly lead to an increase in airway resistance?
Which of the following factors would directly lead to an increase in airway resistance?
Signup and view all the answers
What is the primary role of peripheral chemoreceptors in the control of ventilation?
What is the primary role of peripheral chemoreceptors in the control of ventilation?
Signup and view all the answers
What causes air to passively exit the lungs during normal expiration?
What causes air to passively exit the lungs during normal expiration?
Signup and view all the answers
Which event directly results from capillary hydrostatic pressure exceeding colloid osmotic pressure in pulmonary circulation?
Which event directly results from capillary hydrostatic pressure exceeding colloid osmotic pressure in pulmonary circulation?
Signup and view all the answers
Which of the following accurately describes the role of Type II alveolar cells?
Which of the following accurately describes the role of Type II alveolar cells?
Signup and view all the answers
The cough reflex is triggered by receptors located in the carina. What is the primary physiological purpose of this reflex?
The cough reflex is triggered by receptors located in the carina. What is the primary physiological purpose of this reflex?
Signup and view all the answers
Which of the following best describes the function of the mucociliary transport system?
Which of the following best describes the function of the mucociliary transport system?
Signup and view all the answers
What effect does stimulation of β2-adrenergic receptors have on the respiratory system?
What effect does stimulation of β2-adrenergic receptors have on the respiratory system?
Signup and view all the answers
How would a reduction in airway diameter affect airway resistance and the work of breathing?
How would a reduction in airway diameter affect airway resistance and the work of breathing?
Signup and view all the answers
How do baroreceptors influence ventilation when blood pressure increases?
How do baroreceptors influence ventilation when blood pressure increases?
Signup and view all the answers
What is the anticipated effect on alveolar gas exchange when capillary hydrostatic pressure exceeds colloid osmotic pressure in the pulmonary circulation?
What is the anticipated effect on alveolar gas exchange when capillary hydrostatic pressure exceeds colloid osmotic pressure in the pulmonary circulation?
Signup and view all the answers
What causes air to enter the lungs during normal inspiration?
What causes air to enter the lungs during normal inspiration?
Signup and view all the answers
Flashcards
Mucociliary Clearance
Mucociliary Clearance
A defense mechanism in the respiratory tract involving cilia and mucus to trap and sweep away foreign particles.
Cough Reflex
Cough Reflex
A protective mechanism initiated by cough receptors in the carina to clear airways of foreign matter.
Type I Alveolar Cells
Type I Alveolar Cells
Epithelial cells that form the structure of alveoli, facilitating gas exchange.
Type II Alveolar Cells
Type II Alveolar Cells
Signup and view all the flashcards
Pulmonary Edema
Pulmonary Edema
Signup and view all the flashcards
Airway Resistance
Airway Resistance
Signup and view all the flashcards
Autonomic Nervous System Control
Autonomic Nervous System Control
Signup and view all the flashcards
Baroreceptors
Baroreceptors
Signup and view all the flashcards
Mucus Production
Mucus Production
Signup and view all the flashcards
Alveolar Macrophages
Alveolar Macrophages
Signup and view all the flashcards
Ventilation
Ventilation
Signup and view all the flashcards
Perfusion
Perfusion
Signup and view all the flashcards
Expiration Mechanism
Expiration Mechanism
Signup and view all the flashcards
Inspiration Mechanism
Inspiration Mechanism
Signup and view all the flashcards
Cough Receptors
Cough Receptors
Signup and view all the flashcards
Pulmonary Circulation Mechanism
Pulmonary Circulation Mechanism
Signup and view all the flashcards
Study Notes
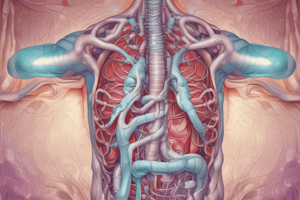
Pulmonary System Function
- The pulmonary system is responsible for gas exchange.
- Airway structures include the trachea, bronchi, bronchioles, and alveoli. The trachea bifurcates into two primary bronchi at the carina.
- The lungs are enclosed by the pleura, with parietal pleura lining the chest cavity and visceral pleura surrounding the lungs.
- Alveoli are tiny air sacs where gas exchange takes place. Alveolar sacs are clusters of alveoli.
- Pulmonary capillaries surround alveoli for efficient gas exchange.
Mucociliary Clearance
- The respiratory tract's lining contains ciliated columnar epithelium and goblet cells.
- Cilia move mucus upwards, enabling the elimination of foreign particles and microorganisms.
- Goblet cells produce mucus, which entraps foreign substances.
- Mucus-producing glands contribute to this process.
Cough Reflex
- The cough reflex is a force/pressure mechanism to clear foreign matter from the airways.
- Cough receptors are located in the carina, the point where the trachea branches into the two primary bronchi.
Alveolar Cells
- Alveolar cells (Type I and II) are involved in gas exchange and surfactant production.
- Type I cells are epithelial structure cells.
- Type II cells produce surfactant.
- Surfactant lowers surface tension in alveoli, facilitating gas exchange. Surfactant is damaged by smoking and silica.
- Alveolar macrophages phagocytize foreign particles.
Mechanisms Affecting Pulmonary Circulation
- Capillary hydrostatic pressure exceeding colloid osmotic pressure can cause fluid leakage into the interstitial space.
- This can lead to alveolar edema, impacting gas exchange. Fluid accumulating into the alveoli is a primary result of poor gas exchange.
Ventilation and Perfusion
- Ventilation and perfusion are two processes significantly influencing alveolar respiration.
Airway Resistance
- Airway resistance is impacted by airway diameter.
- Factors affecting airway resistance include mucus, bronchospasm, stress, pulmonary conditioning, and age. A decrease in airway diameter will result in a greater airway resistance.
Expiration Mechanism
- The lungs deflate passively during exhalation.
- Functional residual capacity refers to the amount of air remaining in the lungs after passive exhalation.
Inspiration Mechanism
- The inspiratory process involves chest wall muscle contraction, diaphragm movement, and intrapleural pressure changes. Inspiration creates a negative intrapleural pressure to inflate the lungs.
Ventilation Control
- The autonomic nervous system regulates respiratory rate (RR).
- Parasympathetic stimulation via the vagus nerve, releasing acetylcholine, causes bronchoconstriction and reduced RR.
- Sympathetic stimulation, activating β₂-adrenergic receptors, relaxes muscles, leading to bronchodilation and increased RR.
Neurologic Control of Ventilation
- The respiratory center in the brainstem, pneumotaxic center, central chemoreceptors, peripheral chemoreceptors, baroreceptors, and proprioceptors are elements of ventilation control.
Baroreceptors and Peripheral Chemoreceptors
- Baroreceptors, located in aortic arch and carotid bodies, respond to blood pressure (BP) fluctuations.
- High BP inhibits inspiration, while low systolic BP (<80 mm Hg) stimulates inspiration.
- Peripheral chemoreceptors in the aortic arch and carotid bodies, monitor arterial oxygen (O₂), hydrogen ion (H⁺) concentration (pH), and carbon dioxide (CO₂) levels.
Perfusion
- Pulmonary vasculature is a low-pressure system.
- Capillary beds surround alveoli, enabling efficient gas exchange.
Hypoxic Vasoconstriction
- Alveolar hypoxia triggers vasoconstriction, diverting blood flow from poorly ventilated areas to better-ventilated areas of the lungs.
Gas Exchange in Alveoli
- Efficient gas exchange between the air in the alveoli and the blood in pulmonary capillaries is essential for respiration in alveoli.
- Oxygen (O₂) diffuses into the blood, and carbon dioxide (CO₂) diffuses out of the blood.
Six Barriers
- Six structures participate in the passage of gases across the respiratory membrane. These include red blood cells, plasma, capillary membrane, interstitial fluid, alveolar membrane, and surfactant.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.