Podcast
Questions and Answers
What is the average diameter of pulmonary capillaries?
What is the average diameter of pulmonary capillaries?
- 8 μm
- 5 μm
- 10 μm
- 6 μm (correct)
Which cells are found within the pulmonary capillary as seen in transmission electron micrographs?
Which cells are found within the pulmonary capillary as seen in transmission electron micrographs?
- Erythrocytes (correct)
- Platelets
- Fibroblasts
- Lymphocytes
What occurs as red blood cells pass through pulmonary capillaries?
What occurs as red blood cells pass through pulmonary capillaries?
- They do not change at all.
- They change shape slightly. (correct)
- They release oxygen.
- They increase in size.
Which of the following factors influences pulmonary vascular smooth muscle response?
Which of the following factors influences pulmonary vascular smooth muscle response?
What initiates gas exchange in the lungs according to the provided content?
What initiates gas exchange in the lungs according to the provided content?
What is a key characteristic of the pulmonary arteries compared to systemic arteries?
What is a key characteristic of the pulmonary arteries compared to systemic arteries?
Where does the venous circuit of the pulmonary circulation begin?
Where does the venous circuit of the pulmonary circulation begin?
What is the capacity of blood located in the pulmonary capillaries per square meter of body surface area?
What is the capacity of blood located in the pulmonary capillaries per square meter of body surface area?
How long does it take for a red blood cell to travel through the pulmonary circulation at resting cardiac output?
How long does it take for a red blood cell to travel through the pulmonary circulation at resting cardiac output?
What is the role of lymphatics in the pulmonary circulation?
What is the role of lymphatics in the pulmonary circulation?
Which of the following statements about pulmonary veins is correct?
Which of the following statements about pulmonary veins is correct?
What is found in the foreground of the scanning electron micrograph of an alveolar septum?
What is found in the foreground of the scanning electron micrograph of an alveolar septum?
What happens to the pulmonary arteries shortly after arising from the main pulmonary artery?
What happens to the pulmonary arteries shortly after arising from the main pulmonary artery?
What can result from impaired movement of O2 from alveoli to pulmonary vasculature?
What can result from impaired movement of O2 from alveoli to pulmonary vasculature?
Which condition is most likely to lead to diffusion limitations in the lungs?
Which condition is most likely to lead to diffusion limitations in the lungs?
What is the primary function of bronchial circulation?
What is the primary function of bronchial circulation?
How does blood flow in the pulmonary circulation compare to that in the bronchial circulation?
How does blood flow in the pulmonary circulation compare to that in the bronchial circulation?
What is the impact of exercise on oxygenation in the lungs?
What is the impact of exercise on oxygenation in the lungs?
What role do anastomoses between bronchial and pulmonary capillaries play in healthy individuals?
What role do anastomoses between bronchial and pulmonary capillaries play in healthy individuals?
What is the typical pulmonary blood flow output at rest?
What is the typical pulmonary blood flow output at rest?
What happens to the diffusion of oxygen during intense exercise?
What happens to the diffusion of oxygen during intense exercise?
What is the percentage of left ventricle output supplied by bronchial circulation?
What is the percentage of left ventricle output supplied by bronchial circulation?
During what conditions is ventilation/perfusion mismatching most prevalent?
During what conditions is ventilation/perfusion mismatching most prevalent?
What primarily regulates pulmonary blood flow?
What primarily regulates pulmonary blood flow?
What is the function of hypoxic pulmonary vasoconstriction?
What is the function of hypoxic pulmonary vasoconstriction?
How is pulmonary vascular resistance calculated?
How is pulmonary vascular resistance calculated?
What happens to the arterioles when the partial pressure of oxygen (PAO2) is low?
What happens to the arterioles when the partial pressure of oxygen (PAO2) is low?
What role does hypoxic vasoconstriction play in lung diseases?
What role does hypoxic vasoconstriction play in lung diseases?
What is a major factor influencing pulmonary blood flow according to the regulation mechanisms?
What is a major factor influencing pulmonary blood flow according to the regulation mechanisms?
Which local vasoactive substance primarily mediates changes in pulmonary vasculature tone?
Which local vasoactive substance primarily mediates changes in pulmonary vasculature tone?
What characterizes hypoxic pulmonary vasoconstriction in terms of location?
What characterizes hypoxic pulmonary vasoconstriction in terms of location?
What is the primary function of the pulmonary circulation?
What is the primary function of the pulmonary circulation?
Which of the following factors does NOT influence pulmonary vascular resistance?
Which of the following factors does NOT influence pulmonary vascular resistance?
What occurs when alveolar surface area decreases relative to arteriolar perfusion?
What occurs when alveolar surface area decreases relative to arteriolar perfusion?
How does hypoxic pulmonary vasoconstriction affect blood flow?
How does hypoxic pulmonary vasoconstriction affect blood flow?
What plays a crucial role in the diffusion of oxygen during pulmonary gas exchange?
What plays a crucial role in the diffusion of oxygen during pulmonary gas exchange?
Why is carbon dioxide less of a concern than oxygen in the context of diffusion in the lungs?
Why is carbon dioxide less of a concern than oxygen in the context of diffusion in the lungs?
Which statement correctly distinguishes pulmonary circulation from systemic circulation?
Which statement correctly distinguishes pulmonary circulation from systemic circulation?
What is the role of ventilation concerning gas concentrations in the lungs?
What is the role of ventilation concerning gas concentrations in the lungs?
Flashcards are hidden until you start studying
Study Notes
Pulmonary Circulation Physiology
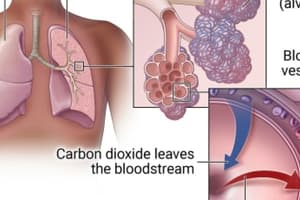
- The pulmonary system's function is to facilitate gas exchange from environmental air into the circulatory system.
- This process involves taking in oxygen (O2), which diffuses into the blood for systemic circulation and is used to produce ATP for energy at a cellular level.
- We exhale carbon dioxide (CO2) along with other metabolic byproducts from the body.
- The lungs consist of tiny air sacs called alveoli, approximately 300 million in number.
- Gas exchange between the air and blood occurs at the surface of these alveoli.
Diffusion
- Diffusion is the passive movement of molecules from an area of higher concentration to an area of lower concentration.
- Ventilation, the movement of air in and out of the lungs, creates an environment where O2 is in high concentration in the lungs and CO2 is in low concentration, relative to the pulmonary capillaries.
- The rate of diffusion is influenced by the solubility of the gas in liquid, gas density, and the available surface area for diffusion within the lungs.
- CO2 is highly soluble in the body's conditions, making O2 the limiting factor concerning diffusion.
- The total available surface area is crucial for efficient gas exchange.
- A decrease in alveolar surface area reduces the potential space for O2 diffusion into the blood, and can lead to hypoxia (low blood oxygen).
Diffusion Limitation
- Diffusion limitation occurs when O2 movement from the alveoli to the pulmonary vasculature is impaired.
- This occurs due to conditions like lung fibrosis and parenchymal destruction of alveoli leading to a reduced alveolar surface area.
- Perfusion refers to the flow of blood through the lungs.
- The ventilation/perfusion ratio (V/Q) measures the efficiency of gas exchange in the lungs.
- Diffusion abnormalities often coexist with V/Q mismatching and are particularly prevalent during exercise.
Pulmonary Circulation
- The lungs receive blood flow through two distinct circulations: the bronchial circulation and the pulmonary circulation.
- Bronchial blood flow: part of the systemic circulation supplying oxygenated blood to the lungs.
- Pulmonary blood flow: carries deoxygenated blood to the lungs for oxygenation, returning oxygenated blood to the heart.
Bronchial Circulation
- The bronchial circulation plays a role in the “air-conditioning” of inhaled air.
- Bronchial arteries originate either directly from the aorta or the intercostal arteries.
- They supply blood to the tracheobronchial tree and lung structures down to the terminal bronchioles.
- The bronchial circulation also provides blood flow to the hilar lymph nodes, visceral pleura, pulmonary arteries and veins, vagus, and esophagus.
- Lung structures beyond the terminal bronchioles receive oxygen directly through diffusion from the alveolar air and nutrients from the mixed venous blood in the pulmonary circulation.
- Bronchial blood flow accounts for about 2% of the left ventricle's output.
- Blood pressure in the bronchial arteries is higher than in the pulmonary arteries, reflecting its connection with the systemic circulation.
Blood Flow to the Lung
- Anastomoses (connections) exist between bronchial and pulmonary capillaries, and between bronchial arteries and branches of the pulmonary artery.
- These connections are less significant in healthy individuals but may open in pathological states, such as when either bronchial or pulmonary blood flow to a portion of the lung is blocked (e.g., by a pulmonary embolus).
Pulmonary Circulation
- Pulmonary blood flow undergoes gas exchange with alveolar air in the pulmonary capillaries.
- Pulmonary blood flow represents approximately 100% of the left ventricle's output.
- Pulmonary blood flow is equal to cardiac output, which is roughly 3.5 L/min/m2 of body surface area at rest.
- 280 billion pulmonary capillaries supply approximately 300 million alveoli.
- One arteriole and its accompanying venule supply and drain one pulmonary lobule.
Pulmonary Circulation: A Low-Pressure System
- The lower pressure of the pulmonary circulation is essential for optimal gas exchange in the delicate lung structures.
Pulmonary Circulation Division
- The pulmonary circulation is divided into three parts:
- Arterial circuit
- Venous circuit
- Lymphatics
Arterial Circuit
- Arises from the main pulmonary artery, originating from the right ventricle.
- Branches into right and left main branches, creating a network of small arteries, arterioles, and capillaries.
- Vessels are thinner and wider than their systemic counterparts, making them more distensible and compliant.
Venous Circuit
- Begins with venules that drain capillaries, joining to form smaller veins ultimately draining into the main pulmonary veins, leading to the left atrium.
- Pulmonary veins are thinner and more distensible than systemic veins.
- Their larger compliance allows them to accommodate more blood.
Lymphatics
- Lymphatics play a vital role in maintaining a dry alveolar membrane and preventing fluid accumulation around the pulmonary circulation.
- These vessels are situated near the terminal bronchioles.
- They drain into the mediastinal lymphatics before emptying into the right lymphatic duct.
Pulmonary Circulation Physiology: Blood Volume
- The pulmonary circulation contains approximately 250-300 mL of blood/m2 of body surface area.
- About 60-70 mL/m2 of this blood resides in the pulmonary capillaries.
- Red blood cells (RBCs) take approximately 4-5 seconds to traverse the pulmonary circulation at resting cardiac outputs; 0.75 seconds of this time is spent in pulmonary capillaries.
Pulmonary Circulation: Microstructure
- Pulmonary capillaries have an average diameter of about 6 μm.
- This is slightly smaller than the average RBC, which is 8 μm in diameter.
- RBCs must slightly deform to navigate through these narrow capillaries.
- An RBC passes through multiple pulmonary capillaries as it travels through the lung.
- Gas exchange begins in smaller pulmonary arterial vessels, which are not technically capillaries by histological standards.
- These arterial segments and successive capillaries function as functional pulmonary capillaries.
Control of Pulmonary Vascular Smooth Muscle
- Pulmonary vascular smooth muscle responds to both neural and humoral influences, leading to "active" changes in pulmonary vascular resistance (PVR).
- "Passive" factors, such as gravity, also contribute to PVR.
Regulation of Pulmonary Circulation
- Pulmonary blood flow is primarily regulated by altering the resistance of the arterioles (PVR).
- These resistance changes are achieved through alterations in the tone of arteriolar smooth muscle.
- In the pulmonary circulation, these changes are mediated by local vasoactive substances, particularly oxygen (O2).
Pulmonary Vascular Resistance
- Pulmonary Vascular Resistance (PVR) is calculated as: R=P1 –P2 / ˙Q
- P1: pressure at the beginning of the tube (in mmHg).
- P2: pressure at the end of the tube (in mmHg).
- ˙Q: flow (in mL/min).
- R: resistance (in mmHg/mL/min).
Regulation of Pulmonary Circulation: Hypoxic Vasoconstriction
- The primary factor regulating pulmonary blood flow is the partial pressure of oxygen in alveolar gas (PAO2).
- The mechanism of hypoxic pulmonary vasoconstriction is not fully understood but has a local effect only in areas with alveolar hypoxia.
- Decreases in PAO2 cause pulmonary vasoconstriction.
Hypoxic Vasoconstriction: Adaptive Role
- In the lungs, hypoxic vasoconstriction acts as an adaptive mechanism, diverting pulmonary blood flow away from poorly ventilated areas where gas exchange would be inefficient.
- This redirects blood flow towards well-ventilated areas of the lung, where gas exchange is more effective.
Hypoxic Vasoconstriction: Protective Role
- In certain lung diseases, hypoxic vasoconstriction serves a protective role, enabling blood redirection to well-oxygenated alveoli without altering overall pulmonary vascular resistance.
- However, if lung disease is widespread (e.g., severe pneumonia) and insufficient well-ventilated alveoli exist, this compensatory mechanism fails, resulting in hypoxemia (low blood oxygen levels).
Mechanism of Hypoxic Vasoconstriction
- The mechanism involves the direct action of alveolar PO2 on the vascular smooth muscle of pulmonary arterioles.
- Oxygen is highly permeable across cell membranes due to its high lipid solubility.
- At normal PAO2 (100 mmHg), oxygen diffuses from the alveoli into nearby arteriolar smooth muscle cells, causing relaxation and dilation of the arterioles.
- When PAO2 is low, O2 diffusion is reduced, triggering vasoconstriction of the arterioles, redirecting blood flow away from poorly ventilated areas.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.