Podcast
Questions and Answers
What is the characteristic appearance of bones in Multiple Myeloma?
What is the characteristic appearance of bones in Multiple Myeloma?
- Swollen or inflamed
- Dense or compact
- Sparse or porous
- Punched-out or honeycombed (correct)
What is the primary goal of Nursing Management in Agranulocytosis?
What is the primary goal of Nursing Management in Agranulocytosis?
- Administering antibiotics
- Protective isolation and drug assessment (correct)
- Promoting ambulation and exercise
- Monitoring laboratory results
What is the primary cause of Coagulopathies in Thrombocytopenia?
What is the primary cause of Coagulopathies in Thrombocytopenia?
- Clotting factor deficiencies
- Increased platelet destruction by the spleen (correct)
- Immune system disorders
- Decreased platelet production by the bone marrow
What is the primary treatment for Disseminated Intravascular Coagulation (DIC)?
What is the primary treatment for Disseminated Intravascular Coagulation (DIC)?
What is the primary symptom of Hemophilia?
What is the primary symptom of Hemophilia?
What is the primary goal of Medical Management in Aplastic Anemia?
What is the primary goal of Medical Management in Aplastic Anemia?
What is the primary goal of administering oxygen in a patient with Hemolytic Anemia?
What is the primary goal of administering oxygen in a patient with Hemolytic Anemia?
A patient with Thalassemia is experiencing bronzing of the skin. What type of Thalassemia is likely?
A patient with Thalassemia is experiencing bronzing of the skin. What type of Thalassemia is likely?
What is the primary cause of Pernicious Anemia?
What is the primary cause of Pernicious Anemia?
A patient with Polycythemia Vera is experiencing reddish-purple face and lips. What is the underlying cause of this condition?
A patient with Polycythemia Vera is experiencing reddish-purple face and lips. What is the underlying cause of this condition?
What is the primary goal of phlebotomy in a patient with Polycythemia Vera?
What is the primary goal of phlebotomy in a patient with Polycythemia Vera?
What is the primary concern for a patient with Leukemia?
What is the primary concern for a patient with Leukemia?
What is the primary mechanism of action of radiation therapy in cancer treatment?
What is the primary mechanism of action of radiation therapy in cancer treatment?
What is the primary goal of nursing management for cancer patients undergoing chemotherapy?
What is the primary goal of nursing management for cancer patients undergoing chemotherapy?
What is the primary benefit of peripheral stem cell transplant in cancer treatment?
What is the primary benefit of peripheral stem cell transplant in cancer treatment?
What is the primary purpose of biologic response modifiers in targeted therapies?
What is the primary purpose of biologic response modifiers in targeted therapies?
What is the primary focus of care for the terminally ill cancer client?
What is the primary focus of care for the terminally ill cancer client?
What is the primary mechanism of action of mohs surgery in cancer treatment?
What is the primary mechanism of action of mohs surgery in cancer treatment?
Which symptom is uniquely associated with hypovolemic anemia as compared to general anemia?
Which symptom is uniquely associated with hypovolemic anemia as compared to general anemia?
Which intervention is specifically required for a patient with hypovolemic anemia?
Which intervention is specifically required for a patient with hypovolemic anemia?
What is the primary cause of sickle cell crisis?
What is the primary cause of sickle cell crisis?
For which type of anemia is prophylactic antibiotic therapy indicated?
For which type of anemia is prophylactic antibiotic therapy indicated?
Which assessment finding is common in both general anemia and sickle cell anemia?
Which assessment finding is common in both general anemia and sickle cell anemia?
Which of the following is NOT a typical treatment for iron deficiency anemia?
Which of the following is NOT a typical treatment for iron deficiency anemia?
Which classification of cancer originates from connective tissue?
Which classification of cancer originates from connective tissue?
What is the second leading cause of death in the United States?
What is the second leading cause of death in the United States?
Which factor is NOT a known contributing factor to cancer development?
Which factor is NOT a known contributing factor to cancer development?
Which diagnostic test detects tumor markers released by cancer cells?
Which diagnostic test detects tumor markers released by cancer cells?
What is indicated by an 'obvious change in size of a wart or mole'?
What is indicated by an 'obvious change in size of a wart or mole'?
Which treatment method is used primarily to relieve uncomfortable symptoms in cancer patients?
Which treatment method is used primarily to relieve uncomfortable symptoms in cancer patients?
Which of the following symptoms is most specifically associated with the onset of tumor lysis syndrome?
Which of the following symptoms is most specifically associated with the onset of tumor lysis syndrome?
Which intervention is critical in managing the potassium levels in patients with tumor lysis syndrome?
Which intervention is critical in managing the potassium levels in patients with tumor lysis syndrome?
What is a primary focus of hospice care for terminal patients?
What is a primary focus of hospice care for terminal patients?
What describes the circulatory changes seen in clinical signs of impending death?
What describes the circulatory changes seen in clinical signs of impending death?
What diagnostic tool is used for staging lymphomas?
What diagnostic tool is used for staging lymphomas?
Which nursing intervention is vital for a client with Hodgkin Disease experiencing respiratory difficulty?
Which nursing intervention is vital for a client with Hodgkin Disease experiencing respiratory difficulty?
What is a common assessment finding in both Hodgkin and non-Hodgkin lymphomas?
What is a common assessment finding in both Hodgkin and non-Hodgkin lymphomas?
What is NOT a component of palliative care for terminal patients?
What is NOT a component of palliative care for terminal patients?
What role does promoting adequate hydration play in managing tumor lysis syndrome?
What role does promoting adequate hydration play in managing tumor lysis syndrome?
What is a common intervention in Hodgkin Disease to protect a patient's bony prominences?
What is a common intervention in Hodgkin Disease to protect a patient's bony prominences?
Which nursing diagnosis is most relevant for a patient with Hodgkin Disease who has impaired skin integrity?
Which nursing diagnosis is most relevant for a patient with Hodgkin Disease who has impaired skin integrity?
What is the purpose of administering Allopurinol in the management of Tumor Lysis Syndrome?
What is the purpose of administering Allopurinol in the management of Tumor Lysis Syndrome?
Which assessment finding is unique to Tumor Lysis Syndrome compared to other oncology emergencies?
Which assessment finding is unique to Tumor Lysis Syndrome compared to other oncology emergencies?
Which medical intervention is primarily utilized for patients with Non-Hodgkin Lymphomas showing aggressive progression?
Which medical intervention is primarily utilized for patients with Non-Hodgkin Lymphomas showing aggressive progression?
What is a primary complication of Tumor Lysis Syndrome due to the release of intracellular contents into the blood?
What is a primary complication of Tumor Lysis Syndrome due to the release of intracellular contents into the blood?
Which staging method is commonly used for diagnosing Hodgkin Disease?
Which staging method is commonly used for diagnosing Hodgkin Disease?
Why is promoting adequate hydration critical in the management of Tumor Lysis Syndrome?
Why is promoting adequate hydration critical in the management of Tumor Lysis Syndrome?
Which feature distinguishes localized radiation therapy in Hodgkin Disease management from other treatments like chemotherapy?
Which feature distinguishes localized radiation therapy in Hodgkin Disease management from other treatments like chemotherapy?
In palliative care, what is the primary goal when integrating the psychological and spiritual aspects of care?
In palliative care, what is the primary goal when integrating the psychological and spiritual aspects of care?
What is a key diagnostic tool for assessing Non-Hodgkin Lymphomas that involves the study of the lymphoid tissue?
What is a key diagnostic tool for assessing Non-Hodgkin Lymphomas that involves the study of the lymphoid tissue?
Which symptom is most indicative of Hodgkin Disease?
Which symptom is most indicative of Hodgkin Disease?
What is the primary role of administering diuretics in patients with Tumor Lysis Syndrome?
What is the primary role of administering diuretics in patients with Tumor Lysis Syndrome?
What is a common diagnostic tool used for both Hodgkin and Non-Hodgkin lymphomas?
What is a common diagnostic tool used for both Hodgkin and Non-Hodgkin lymphomas?
Which symptom is a sign of clinical impending death's effect on the circulatory system?
Which symptom is a sign of clinical impending death's effect on the circulatory system?
Which classification of Non-Hodgkin Lymphomas is known to progress slowly?
Which classification of Non-Hodgkin Lymphomas is known to progress slowly?
What is the primary diagnostic tool used to stage lymphoma?
What is the primary diagnostic tool used to stage lymphoma?
What is the main nursing intervention to manage respiratory difficulty in Hodgkin Disease?
What is the main nursing intervention to manage respiratory difficulty in Hodgkin Disease?
Which of the following treatments is common in the medical management of both Hodgkin Disease and Non-Hodgkin Lymphomas?
Which of the following treatments is common in the medical management of both Hodgkin Disease and Non-Hodgkin Lymphomas?
Which symptom is specifically associated with Tumor Lysis Syndrome (TLS) rather than general cancer symptoms?
Which symptom is specifically associated with Tumor Lysis Syndrome (TLS) rather than general cancer symptoms?
What is the goal when integrating the psychological and spiritual aspects of care in palliative care?
What is the goal when integrating the psychological and spiritual aspects of care in palliative care?
What is the primary goal of Medical Management in Hodgkin Disease?
What is the primary goal of Medical Management in Hodgkin Disease?
Which diagnostic test is used to assess the spread of Non-Hodgkin Lymphoma?
Which diagnostic test is used to assess the spread of Non-Hodgkin Lymphoma?
What is the primary complication of Tumor Lysis Syndrome due to the release of intracellular contents into the blood?
What is the primary complication of Tumor Lysis Syndrome due to the release of intracellular contents into the blood?
What is the primary purpose of administering Allopurinol in the management of Tumor Lysis Syndrome?
What is the primary purpose of administering Allopurinol in the management of Tumor Lysis Syndrome?
What is the primary focus of hospice care for terminal patients?
What is the primary focus of hospice care for terminal patients?
What is a key diagnostic tool for assessing Non-Hodgkin Lymphomas that involves the study of the lymphoid tissue?
What is a key diagnostic tool for assessing Non-Hodgkin Lymphomas that involves the study of the lymphoid tissue?
What is the primary goal of nursing management for cancer patients undergoing chemotherapy?
What is the primary goal of nursing management for cancer patients undergoing chemotherapy?
What is a common assessment finding in both Hodgkin and non-Hodgkin lymphomas?
What is a common assessment finding in both Hodgkin and non-Hodgkin lymphomas?
What is the primary mechanism of action of radiation therapy in cancer treatment?
What is the primary mechanism of action of radiation therapy in cancer treatment?
What is the primary benefit of peripheral stem cell transplant in cancer treatment?
What is the primary benefit of peripheral stem cell transplant in cancer treatment?
Flashcards are hidden until you start studying
Study Notes
Blood Disorders
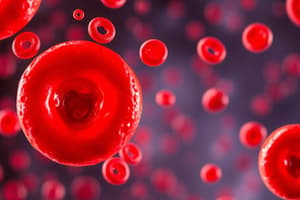
- Anemia: deficiency of erythrocytes or hemoglobin
- Causes: blood loss, inadequate erythrocyte production, destruction of formed RBCs
- Assessment findings: inadequate RBC volume, tachycardia, tachypnea, cool, clammy skin, amenorrhea
- Compensatory mechanisms: tachycardia, tachypnea, cool, clammy skin, amenorrhea
- Hypovolemic Anemia
- Causes: sudden loss of large volume, chronic loss of small amounts of blood
- Assessment findings: extreme pallor, tachycardia, hypotension, reduced urine output, altered consciousness, fatigue, chills, rapid respiratory rate
- Medical management: blood transfusions, administration of oral, IV, or IM iron
- Nursing process: monitor results of CBC, assess vital signs, monitor I&O
- Iron Deficiency Anemia
- Causes: insufficient iron to produce hemoglobin
- Assessment findings: reduced energy, feeling cold, fatigue, and dyspnea with minor physical exertion, rapid heart rate even at rest, decreased hemoglobin, hematocrit, and serum iron levels
- Medical management: foods high in iron, blood transfusions
- Nursing management: increase iron intake, collaborate with dietitian, administer iron supplement (IM Z-track)
- Sickle Cell Anemia
- Causes: Hemoglobin A replaced by Hemoglobin S; sickle- or crescent-shaped erythrocytes from inadequate oxygen supply to blood
- Assessment findings: jaundice, tachycardia, dyspnea, cardiomegaly, and dysrhythmias; stroke, acute chest syndrome
- Medical management: supportive treatment, regular blood transfusions, bone marrow transplantation, prophylactic antibiotic therapy
- Nursing process: assess health history, vital signs, physical assessment, evident dehydration, and pain; provide analgesics, oxygen, and fluids
- Hemolytic Anemia
- Causes: chronic premature erythrocyte destruction
- Assessment findings: jaundice, enlarged spleen, shock
- Medical management: removing the cause, corticosteroids, blood transfusions
- Nursing management: health history, supportive care, medication, teaching measures of self-care, arrange follow-up evaluations
- Thalassemia
- Causes: hereditary hemolytic anemia
- Assessment findings: Cooley's anemia: bronzing of the skin
- Medical management: symptomatic, frequent transfusions, iron chelation therapy
- Nursing management: bed rest, protect from infection, closely monitor blood transfusion
- Pernicious Anemia
- Causes: lack of intrinsic factor necessary for absorption of vitamin B12
- Assessment findings: stomatitis, glossitis, digestive disturbances, diarrhea, dyspnea with minimal exertion, jaundice, irritability, confusion, depression, numbness, and tingling in arms and legs, ataxia
- Medical management: IM vitamin B12, physical therapy for permanent neurologic deficits
- Nursing management: soft, bland diet, small, frequent meals, oral care, encourage and assist with ambulation, supervision
- Folic Acid Deficiency Anemia
- Causes: immature erythrocytes, insufficient dietary intake of foods rich in folic acid
- Assessment findings: severe fatigue, sore and beefy-red tongue, dyspnea, nausea, anorexia, headaches, weakness, light-headedness
- Medical management: folic acid supplements, balanced diet
- Nursing management: teaching, diet, oral hygiene, rest promotion
Leukocytosis and Leukemia
- Leukocytosis: proliferation of leukocytes, usually in immature form
- Causes: genetic correlation, precipitating factors
- Assessment findings: severe anemia, infections, fatigue, easy bruising, fever, enlarged spleen and lymph nodes, internal or external bleeding
- Medical management: antineoplastic drugs, transfusions, transplantation: bone marrow, stem cell
- Nursing process: assess history of symptoms, physical assessment, laboratory results, assess neutrophil, monitor platelet counts, assess for signs of bruising and petechiae, report hematuria or epistaxis
- Leukemia
- Types: acute and chronic forms of lymphocytic and myelogenous leukemia
- Assessment findings: severe anemia, infections, fatigue, easy bruising, fever, enlarged spleen and lymph nodes, internal or external bleeding
- Medical management: antineoplastic drugs, transfusions, transplantation: bone marrow, stem cell
- Nursing process: assess history of symptoms, physical assessment, laboratory results, assess neutrophil, monitor platelet counts, assess for signs of bruising and petechiae, report hematuria or epistaxis
Cancer
- Definition: abnormal, unregulated cell growth; neoplasms
- Classifications: carcinomas, lymphomas, leukemias, sarcomas
- TNM classification: tumor, node, metastasis
- Stages: I to IV
- Etiology: genetic mutation, environmental factors, chemicals, radiation, viruses
- Factors: chemical agents, environmental factors, diet, viruses, bacteria, medications, immune system
- Signs and symptoms: headaches, weight loss, chronic pain, persistent fatigue, low-grade fever, infections
- Diagnostic tests: client's history, physical examination, laboratory tests, imaging studies, biopsies
- Cancer treatment
- Surgery: primary method of diagnosing, staging, and treating
- Radiation: destroys cell by breaking a strand of DNA molecule, preventing growth
- Chemotherapy: antineoplastic agents, cell cycle patterns
- Targeted therapies: biologic response modifiers, monoclonal antibody immunotherapy, cancer vaccines
- Stem cell transplant: replaces bone marrow destroyed by cancer or cancer treatments
- Nursing care plan
- Nursing diagnosis: fatigue, imbalanced nutrition, disturbed body image
- Interventions: encourage protein and calorie intake, plan care around energy level, administer antiemetics, explore strengths and resources
Coagulopathies
- Thrombocytopenia: platelet manufacture by bone marrow is decreased or platelet destruction by the spleen is increased
- Causes: leukemia, malignant blood diseases, severe infections
- Assessment findings: purpura, bleeding, internal hemorrhage
- Medical management: eliminate cause, corticosteroids, transfusions
- Surgical management: splenectomy
- Nursing management: manage/minimize bleeding, apply pressure/tourniquet, ADR, taper corticosteroid dosage/frequency
- Hemophilia: clotting factor, inherited: mother to son
- Assessment findings: oozing, severe bleeding, bleeding in joints
- Diagnostic findings: coagulant factor assay
- Medical management: transfusions, thrombin/fibrin application, fresh frozen plasma, direct pressure
- Nursing management: health history, physical assessment, VS, prevent trauma, minimize bleeding, reduce pain or discomfort
- Disseminated Intravascular Coagulation (DIC)
- Causes: shock, infections, trauma, burns, transfusion reaction, cancer, and obstetric complications
- Assessment findings: petechiae, purpura, ecchymoses, tachycardia, hypotension, cold/mottled fingers and toes
- Medical management: correction of the cause, replacement of platelets, coagulation factors, and fibrinogen
- Nursing management: assess pain, signs of infection, fatigue, bleeding, thrombus formation, urine output, safety, prevent infection
Palliative Care
- Definition: neither hastens nor postpones death, provides pain relief and reduces distressing symptoms
- Integrates the psychological and spiritual aspects of care
- Provides support system to help clients live as actively as possible until death
- Referral to support system to help clients' families cope during the client's illness and in their own bereavement
- Hospice care
- Initiated for patients as they near the end of life
- Emphasizes quality of life
- Patient and family are included in plan of care
- Provides support for a dignified and peaceful death
- Palliative rather than curative
Blood Disorders
- Anemia: deficiency of erythrocytes or hemoglobin
- Causes: blood loss, inadequate erythrocyte production, destruction of formed RBCs
- Assessment findings: inadequate RBC volume, tachycardia, tachypnea, cool, clammy skin, amenorrhea
- Compensatory mechanisms: tachycardia, tachypnea, cool, clammy skin, amenorrhea
- Hypovolemic Anemia
- Causes: sudden loss of large volume, chronic loss of small amounts of blood
- Assessment findings: extreme pallor, tachycardia, hypotension, reduced urine output, altered consciousness, fatigue, chills, rapid respiratory rate
- Medical management: blood transfusions, administration of oral, IV, or IM iron
- Nursing process: monitor results of CBC, assess vital signs, monitor I&O
- Iron Deficiency Anemia
- Causes: insufficient iron to produce hemoglobin
- Assessment findings: reduced energy, feeling cold, fatigue, and dyspnea with minor physical exertion, rapid heart rate even at rest, decreased hemoglobin, hematocrit, and serum iron levels
- Medical management: foods high in iron, blood transfusions
- Nursing management: increase iron intake, collaborate with dietitian, administer iron supplement (IM Z-track)
- Sickle Cell Anemia
- Causes: Hemoglobin A replaced by Hemoglobin S; sickle- or crescent-shaped erythrocytes from inadequate oxygen supply to blood
- Assessment findings: jaundice, tachycardia, dyspnea, cardiomegaly, and dysrhythmias; stroke, acute chest syndrome
- Medical management: supportive treatment, regular blood transfusions, bone marrow transplantation, prophylactic antibiotic therapy
- Nursing process: assess health history, vital signs, physical assessment, evident dehydration, and pain; provide analgesics, oxygen, and fluids
- Hemolytic Anemia
- Causes: chronic premature erythrocyte destruction
- Assessment findings: jaundice, enlarged spleen, shock
- Medical management: removing the cause, corticosteroids, blood transfusions
- Nursing management: health history, supportive care, medication, teaching measures of self-care, arrange follow-up evaluations
- Thalassemia
- Causes: hereditary hemolytic anemia
- Assessment findings: Cooley's anemia: bronzing of the skin
- Medical management: symptomatic, frequent transfusions, iron chelation therapy
- Nursing management: bed rest, protect from infection, closely monitor blood transfusion
- Pernicious Anemia
- Causes: lack of intrinsic factor necessary for absorption of vitamin B12
- Assessment findings: stomatitis, glossitis, digestive disturbances, diarrhea, dyspnea with minimal exertion, jaundice, irritability, confusion, depression, numbness, and tingling in arms and legs, ataxia
- Medical management: IM vitamin B12, physical therapy for permanent neurologic deficits
- Nursing management: soft, bland diet, small, frequent meals, oral care, encourage and assist with ambulation, supervision
- Folic Acid Deficiency Anemia
- Causes: immature erythrocytes, insufficient dietary intake of foods rich in folic acid
- Assessment findings: severe fatigue, sore and beefy-red tongue, dyspnea, nausea, anorexia, headaches, weakness, light-headedness
- Medical management: folic acid supplements, balanced diet
- Nursing management: teaching, diet, oral hygiene, rest promotion
Leukocytosis and Leukemia
- Leukocytosis: proliferation of leukocytes, usually in immature form
- Causes: genetic correlation, precipitating factors
- Assessment findings: severe anemia, infections, fatigue, easy bruising, fever, enlarged spleen and lymph nodes, internal or external bleeding
- Medical management: antineoplastic drugs, transfusions, transplantation: bone marrow, stem cell
- Nursing process: assess history of symptoms, physical assessment, laboratory results, assess neutrophil, monitor platelet counts, assess for signs of bruising and petechiae, report hematuria or epistaxis
- Leukemia
- Types: acute and chronic forms of lymphocytic and myelogenous leukemia
- Assessment findings: severe anemia, infections, fatigue, easy bruising, fever, enlarged spleen and lymph nodes, internal or external bleeding
- Medical management: antineoplastic drugs, transfusions, transplantation: bone marrow, stem cell
- Nursing process: assess history of symptoms, physical assessment, laboratory results, assess neutrophil, monitor platelet counts, assess for signs of bruising and petechiae, report hematuria or epistaxis
Cancer
- Definition: abnormal, unregulated cell growth; neoplasms
- Classifications: carcinomas, lymphomas, leukemias, sarcomas
- TNM classification: tumor, node, metastasis
- Stages: I to IV
- Etiology: genetic mutation, environmental factors, chemicals, radiation, viruses
- Factors: chemical agents, environmental factors, diet, viruses, bacteria, medications, immune system
- Signs and symptoms: headaches, weight loss, chronic pain, persistent fatigue, low-grade fever, infections
- Diagnostic tests: client's history, physical examination, laboratory tests, imaging studies, biopsies
- Cancer treatment
- Surgery: primary method of diagnosing, staging, and treating
- Radiation: destroys cell by breaking a strand of DNA molecule, preventing growth
- Chemotherapy: antineoplastic agents, cell cycle patterns
- Targeted therapies: biologic response modifiers, monoclonal antibody immunotherapy, cancer vaccines
- Stem cell transplant: replaces bone marrow destroyed by cancer or cancer treatments
- Nursing care plan
- Nursing diagnosis: fatigue, imbalanced nutrition, disturbed body image
- Interventions: encourage protein and calorie intake, plan care around energy level, administer antiemetics, explore strengths and resources
Coagulopathies
- Thrombocytopenia: platelet manufacture by bone marrow is decreased or platelet destruction by the spleen is increased
- Causes: leukemia, malignant blood diseases, severe infections
- Assessment findings: purpura, bleeding, internal hemorrhage
- Medical management: eliminate cause, corticosteroids, transfusions
- Surgical management: splenectomy
- Nursing management: manage/minimize bleeding, apply pressure/tourniquet, ADR, taper corticosteroid dosage/frequency
- Hemophilia: clotting factor, inherited: mother to son
- Assessment findings: oozing, severe bleeding, bleeding in joints
- Diagnostic findings: coagulant factor assay
- Medical management: transfusions, thrombin/fibrin application, fresh frozen plasma, direct pressure
- Nursing management: health history, physical assessment, VS, prevent trauma, minimize bleeding, reduce pain or discomfort
- Disseminated Intravascular Coagulation (DIC)
- Causes: shock, infections, trauma, burns, transfusion reaction, cancer, and obstetric complications
- Assessment findings: petechiae, purpura, ecchymoses, tachycardia, hypotension, cold/mottled fingers and toes
- Medical management: correction of the cause, replacement of platelets, coagulation factors, and fibrinogen
- Nursing management: assess pain, signs of infection, fatigue, bleeding, thrombus formation, urine output, safety, prevent infection
Palliative Care
- Definition: neither hastens nor postpones death, provides pain relief and reduces distressing symptoms
- Integrates the psychological and spiritual aspects of care
- Provides support system to help clients live as actively as possible until death
- Referral to support system to help clients' families cope during the client's illness and in their own bereavement
- Hospice care
- Initiated for patients as they near the end of life
- Emphasizes quality of life
- Patient and family are included in plan of care
- Provides support for a dignified and peaceful death
- Palliative rather than curative
Blood Disorders
- Anemia: deficiency of erythrocytes or hemoglobin
- Causes: blood loss, inadequate erythrocyte production, destruction of formed RBCs
- Assessment findings: inadequate RBC volume, tachycardia, tachypnea, cool, clammy skin, amenorrhea
- Compensatory mechanisms: tachycardia, tachypnea, cool, clammy skin, amenorrhea
- Hypovolemic Anemia
- Causes: sudden loss of large volume, chronic loss of small amounts of blood
- Assessment findings: extreme pallor, tachycardia, hypotension, reduced urine output, altered consciousness, fatigue, chills, rapid respiratory rate
- Medical management: blood transfusions, administration of oral, IV, or IM iron
- Nursing process: monitor results of CBC, assess vital signs, monitor I&O
- Iron Deficiency Anemia
- Causes: insufficient iron to produce hemoglobin
- Assessment findings: reduced energy, feeling cold, fatigue, and dyspnea with minor physical exertion, rapid heart rate even at rest, decreased hemoglobin, hematocrit, and serum iron levels
- Medical management: foods high in iron, blood transfusions
- Nursing management: increase iron intake, collaborate with dietitian, administer iron supplement (IM Z-track)
- Sickle Cell Anemia
- Causes: Hemoglobin A replaced by Hemoglobin S; sickle- or crescent-shaped erythrocytes from inadequate oxygen supply to blood
- Assessment findings: jaundice, tachycardia, dyspnea, cardiomegaly, and dysrhythmias; stroke, acute chest syndrome
- Medical management: supportive treatment, regular blood transfusions, bone marrow transplantation, prophylactic antibiotic therapy
- Nursing process: assess health history, vital signs, physical assessment, evident dehydration, and pain; provide analgesics, oxygen, and fluids
- Hemolytic Anemia
- Causes: chronic premature erythrocyte destruction
- Assessment findings: jaundice, enlarged spleen, shock
- Medical management: removing the cause, corticosteroids, blood transfusions
- Nursing management: health history, supportive care, medication, teaching measures of self-care, arrange follow-up evaluations
- Thalassemia
- Causes: hereditary hemolytic anemia
- Assessment findings: Cooley's anemia: bronzing of the skin
- Medical management: symptomatic, frequent transfusions, iron chelation therapy
- Nursing management: bed rest, protect from infection, closely monitor blood transfusion
- Pernicious Anemia
- Causes: lack of intrinsic factor necessary for absorption of vitamin B12
- Assessment findings: stomatitis, glossitis, digestive disturbances, diarrhea, dyspnea with minimal exertion, jaundice, irritability, confusion, depression, numbness, and tingling in arms and legs, ataxia
- Medical management: IM vitamin B12, physical therapy for permanent neurologic deficits
- Nursing management: soft, bland diet, small, frequent meals, oral care, encourage and assist with ambulation, supervision
- Folic Acid Deficiency Anemia
- Causes: immature erythrocytes, insufficient dietary intake of foods rich in folic acid
- Assessment findings: severe fatigue, sore and beefy-red tongue, dyspnea, nausea, anorexia, headaches, weakness, light-headedness
- Medical management: folic acid supplements, balanced diet
- Nursing management: teaching, diet, oral hygiene, rest promotion
Leukocytosis and Leukemia
- Leukocytosis: proliferation of leukocytes, usually in immature form
- Causes: genetic correlation, precipitating factors
- Assessment findings: severe anemia, infections, fatigue, easy bruising, fever, enlarged spleen and lymph nodes, internal or external bleeding
- Medical management: antineoplastic drugs, transfusions, transplantation: bone marrow, stem cell
- Nursing process: assess history of symptoms, physical assessment, laboratory results, assess neutrophil, monitor platelet counts, assess for signs of bruising and petechiae, report hematuria or epistaxis
- Leukemia
- Types: acute and chronic forms of lymphocytic and myelogenous leukemia
- Assessment findings: severe anemia, infections, fatigue, easy bruising, fever, enlarged spleen and lymph nodes, internal or external bleeding
- Medical management: antineoplastic drugs, transfusions, transplantation: bone marrow, stem cell
- Nursing process: assess history of symptoms, physical assessment, laboratory results, assess neutrophil, monitor platelet counts, assess for signs of bruising and petechiae, report hematuria or epistaxis
Cancer
- Definition: abnormal, unregulated cell growth; neoplasms
- Classifications: carcinomas, lymphomas, leukemias, sarcomas
- TNM classification: tumor, node, metastasis
- Stages: I to IV
- Etiology: genetic mutation, environmental factors, chemicals, radiation, viruses
- Factors: chemical agents, environmental factors, diet, viruses, bacteria, medications, immune system
- Signs and symptoms: headaches, weight loss, chronic pain, persistent fatigue, low-grade fever, infections
- Diagnostic tests: client's history, physical examination, laboratory tests, imaging studies, biopsies
- Cancer treatment
- Surgery: primary method of diagnosing, staging, and treating
- Radiation: destroys cell by breaking a strand of DNA molecule, preventing growth
- Chemotherapy: antineoplastic agents, cell cycle patterns
- Targeted therapies: biologic response modifiers, monoclonal antibody immunotherapy, cancer vaccines
- Stem cell transplant: replaces bone marrow destroyed by cancer or cancer treatments
- Nursing care plan
- Nursing diagnosis: fatigue, imbalanced nutrition, disturbed body image
- Interventions: encourage protein and calorie intake, plan care around energy level, administer antiemetics, explore strengths and resources
Coagulopathies
- Thrombocytopenia: platelet manufacture by bone marrow is decreased or platelet destruction by the spleen is increased
- Causes: leukemia, malignant blood diseases, severe infections
- Assessment findings: purpura, bleeding, internal hemorrhage
- Medical management: eliminate cause, corticosteroids, transfusions
- Surgical management: splenectomy
- Nursing management: manage/minimize bleeding, apply pressure/tourniquet, ADR, taper corticosteroid dosage/frequency
- Hemophilia: clotting factor, inherited: mother to son
- Assessment findings: oozing, severe bleeding, bleeding in joints
- Diagnostic findings: coagulant factor assay
- Medical management: transfusions, thrombin/fibrin application, fresh frozen plasma, direct pressure
- Nursing management: health history, physical assessment, VS, prevent trauma, minimize bleeding, reduce pain or discomfort
- Disseminated Intravascular Coagulation (DIC)
- Causes: shock, infections, trauma, burns, transfusion reaction, cancer, and obstetric complications
- Assessment findings: petechiae, purpura, ecchymoses, tachycardia, hypotension, cold/mottled fingers and toes
- Medical management: correction of the cause, replacement of platelets, coagulation factors, and fibrinogen
- Nursing management: assess pain, signs of infection, fatigue, bleeding, thrombus formation, urine output, safety, prevent infection
Palliative Care
- Definition: neither hastens nor postpones death, provides pain relief and reduces distressing symptoms
- Integrates the psychological and spiritual aspects of care
- Provides support system to help clients live as actively as possible until death
- Referral to support system to help clients' families cope during the client's illness and in their own bereavement
- Hospice care
- Initiated for patients as they near the end of life
- Emphasizes quality of life
- Patient and family are included in plan of care
- Provides support for a dignified and peaceful death
- Palliative rather than curative
Blood Disorders
- Anemia: deficiency of erythrocytes or hemoglobin
- Causes: blood loss, inadequate erythrocyte production, destruction of formed RBCs
- Assessment findings: inadequate RBC volume, tachycardia, tachypnea, cool, clammy skin, amenorrhea
- Compensatory mechanisms: tachycardia, tachypnea, cool, clammy skin, amenorrhea
- Hypovolemic Anemia
- Causes: sudden loss of large volume, chronic loss of small amounts of blood
- Assessment findings: extreme pallor, tachycardia, hypotension, reduced urine output, altered consciousness, fatigue, chills, rapid respiratory rate
- Medical management: blood transfusions, administration of oral, IV, or IM iron
- Nursing process: monitor results of CBC, assess vital signs, monitor I&O
- Iron Deficiency Anemia
- Causes: insufficient iron to produce hemoglobin
- Assessment findings: reduced energy, feeling cold, fatigue, and dyspnea with minor physical exertion, rapid heart rate even at rest, decreased hemoglobin, hematocrit, and serum iron levels
- Medical management: foods high in iron, blood transfusions
- Nursing management: increase iron intake, collaborate with dietitian, administer iron supplement (IM Z-track)
- Sickle Cell Anemia
- Causes: Hemoglobin A replaced by Hemoglobin S; sickle- or crescent-shaped erythrocytes from inadequate oxygen supply to blood
- Assessment findings: jaundice, tachycardia, dyspnea, cardiomegaly, and dysrhythmias; stroke, acute chest syndrome
- Medical management: supportive treatment, regular blood transfusions, bone marrow transplantation, prophylactic antibiotic therapy
- Nursing process: assess health history, vital signs, physical assessment, evident dehydration, and pain; provide analgesics, oxygen, and fluids
- Hemolytic Anemia
- Causes: chronic premature erythrocyte destruction
- Assessment findings: jaundice, enlarged spleen, shock
- Medical management: removing the cause, corticosteroids, blood transfusions
- Nursing management: health history, supportive care, medication, teaching measures of self-care, arrange follow-up evaluations
- Thalassemia
- Causes: hereditary hemolytic anemia
- Assessment findings: Cooley's anemia: bronzing of the skin
- Medical management: symptomatic, frequent transfusions, iron chelation therapy
- Nursing management: bed rest, protect from infection, closely monitor blood transfusion
- Pernicious Anemia
- Causes: lack of intrinsic factor necessary for absorption of vitamin B12
- Assessment findings: stomatitis, glossitis, digestive disturbances, diarrhea, dyspnea with minimal exertion, jaundice, irritability, confusion, depression, numbness, and tingling in arms and legs, ataxia
- Medical management: IM vitamin B12, physical therapy for permanent neurologic deficits
- Nursing management: soft, bland diet, small, frequent meals, oral care, encourage and assist with ambulation, supervision
- Folic Acid Deficiency Anemia
- Causes: immature erythrocytes, insufficient dietary intake of foods rich in folic acid
- Assessment findings: severe fatigue, sore and beefy-red tongue, dyspnea, nausea, anorexia, headaches, weakness, light-headedness
- Medical management: folic acid supplements, balanced diet
- Nursing management: teaching, diet, oral hygiene, rest promotion
Leukocytosis and Leukemia
- Leukocytosis: proliferation of leukocytes, usually in immature form
- Causes: genetic correlation, precipitating factors
- Assessment findings: severe anemia, infections, fatigue, easy bruising, fever, enlarged spleen and lymph nodes, internal or external bleeding
- Medical management: antineoplastic drugs, transfusions, transplantation: bone marrow, stem cell
- Nursing process: assess history of symptoms, physical assessment, laboratory results, assess neutrophil, monitor platelet counts, assess for signs of bruising and petechiae, report hematuria or epistaxis
- Leukemia
- Types: acute and chronic forms of lymphocytic and myelogenous leukemia
- Assessment findings: severe anemia, infections, fatigue, easy bruising, fever, enlarged spleen and lymph nodes, internal or external bleeding
- Medical management: antineoplastic drugs, transfusions, transplantation: bone marrow, stem cell
- Nursing process: assess history of symptoms, physical assessment, laboratory results, assess neutrophil, monitor platelet counts, assess for signs of bruising and petechiae, report hematuria or epistaxis
Cancer
- Definition: abnormal, unregulated cell growth; neoplasms
- Classifications: carcinomas, lymphomas, leukemias, sarcomas
- TNM classification: tumor, node, metastasis
- Stages: I to IV
- Etiology: genetic mutation, environmental factors, chemicals, radiation, viruses
- Factors: chemical agents, environmental factors, diet, viruses, bacteria, medications, immune system
- Signs and symptoms: headaches, weight loss, chronic pain, persistent fatigue, low-grade fever, infections
- Diagnostic tests: client's history, physical examination, laboratory tests, imaging studies, biopsies
- Cancer treatment
- Surgery: primary method of diagnosing, staging, and treating
- Radiation: destroys cell by breaking a strand of DNA molecule, preventing growth
- Chemotherapy: antineoplastic agents, cell cycle patterns
- Targeted therapies: biologic response modifiers, monoclonal antibody immunotherapy, cancer vaccines
- Stem cell transplant: replaces bone marrow destroyed by cancer or cancer treatments
- Nursing care plan
- Nursing diagnosis: fatigue, imbalanced nutrition, disturbed body image
- Interventions: encourage protein and calorie intake, plan care around energy level, administer antiemetics, explore strengths and resources
Coagulopathies
- Thrombocytopenia: platelet manufacture by bone marrow is decreased or platelet destruction by the spleen is increased
- Causes: leukemia, malignant blood diseases, severe infections
- Assessment findings: purpura, bleeding, internal hemorrhage
- Medical management: eliminate cause, corticosteroids, transfusions
- Surgical management: splenectomy
- Nursing management: manage/minimize bleeding, apply pressure/tourniquet, ADR, taper corticosteroid dosage/frequency
- Hemophilia: clotting factor, inherited: mother to son
- Assessment findings: oozing, severe bleeding, bleeding in joints
- Diagnostic findings: coagulant factor assay
- Medical management: transfusions, thrombin/fibrin application, fresh frozen plasma, direct pressure
- Nursing management: health history, physical assessment, VS, prevent trauma, minimize bleeding, reduce pain or discomfort
- Disseminated Intravascular Coagulation (DIC)
- Causes: shock, infections, trauma, burns, transfusion reaction, cancer, and obstetric complications
- Assessment findings: petechiae, purpura, ecchymoses, tachycardia, hypotension, cold/mottled fingers and toes
- Medical management: correction of the cause, replacement of platelets, coagulation factors, and fibrinogen
- Nursing management: assess pain, signs of infection, fatigue, bleeding, thrombus formation, urine output, safety, prevent infection
Palliative Care
- Definition: neither hastens nor postpones death, provides pain relief and reduces distressing symptoms
- Integrates the psychological and spiritual aspects of care
- Provides support system to help clients live as actively as possible until death
- Referral to support system to help clients' families cope during the client's illness and in their own bereavement
- Hospice care
- Initiated for patients as they near the end of life
- Emphasizes quality of life
- Patient and family are included in plan of care
- Provides support for a dignified and peaceful death
- Palliative rather than curative
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.