Podcast
Questions and Answers
What is the definition of pneumothorax?
What is the definition of pneumothorax?
- Presence of air in the pleural cavity (correct)
- Inflammation of lung tissue
- Fluid accumulation in the lungs
- Infection in the pleural cavity
Which of the following is NOT a type of pneumothorax?
Which of the following is NOT a type of pneumothorax?
- Traumatic Pneumothorax
- Obstructive Pneumothorax (correct)
- Spontaneous Pneumothorax
- Secondary Pneumothorax
Intrapleural pressure is typically positive compared to intrapulmonary pressure.
Intrapleural pressure is typically positive compared to intrapulmonary pressure.
False (B)
Name one risk factor for spontaneous pneumothorax.
Name one risk factor for spontaneous pneumothorax.
The presence of air in the pleural cavity can lead to lung __________.
The presence of air in the pleural cavity can lead to lung __________.
Which condition is associated with the development of subpleural blebs?
Which condition is associated with the development of subpleural blebs?
Breach in the chest wall can cause traumatic pneumothorax.
Breach in the chest wall can cause traumatic pneumothorax.
The __________ is attached to the chest wall.
The __________ is attached to the chest wall.
Match the following types of pneumothorax with their definitions:
Match the following types of pneumothorax with their definitions:
What effect does lung collapse have on intrapleural pressure?
What effect does lung collapse have on intrapleural pressure?
Which of the following is a cause of iatrogenic pneumothorax?
Which of the following is a cause of iatrogenic pneumothorax?
Tension pneumothorax can lead to significant hypotension and jugular venous distension.
Tension pneumothorax can lead to significant hypotension and jugular venous distension.
What is a common symptom of pneumothorax?
What is a common symptom of pneumothorax?
In tension pneumothorax, pressure accumulation can lead to ______________ of mediastinal structures.
In tension pneumothorax, pressure accumulation can lead to ______________ of mediastinal structures.
Match the following types of pneumothorax with their definitions:
Match the following types of pneumothorax with their definitions:
Which examination finding is associated with a pneumothorax?
Which examination finding is associated with a pneumothorax?
Percussion of the chest over a pneumothorax typically produces a dull sound.
Percussion of the chest over a pneumothorax typically produces a dull sound.
What imaging technique is typically used to diagnose pneumothorax?
What imaging technique is typically used to diagnose pneumothorax?
In a closed pneumothorax, air enters the pleural space through a break in the chest wall but does not ________________ during exhalation.
In a closed pneumothorax, air enters the pleural space through a break in the chest wall but does not ________________ during exhalation.
What compensatory mechanism occurs in response to hypoxemia due to pneumothorax?
What compensatory mechanism occurs in response to hypoxemia due to pneumothorax?
Which type of pneumothorax occurs in individuals without underlying lung disease?
Which type of pneumothorax occurs in individuals without underlying lung disease?
Accumulation of air in the pleural space decreases intrapleural pressure.
Accumulation of air in the pleural space decreases intrapleural pressure.
Name two physiological roles of the pleural cavity.
Name two physiological roles of the pleural cavity.
Tall, thin, young males who smoke are at risk for __________ pneumothorax.
Tall, thin, young males who smoke are at risk for __________ pneumothorax.
Match the following conditions with their descriptions:
Match the following conditions with their descriptions:
Which of the following is a common cause for air to enter the pleural space?
Which of the following is a common cause for air to enter the pleural space?
The visceral pleura is attached to the chest wall.
The visceral pleura is attached to the chest wall.
What is the typical intrapleural pressure value in a healthy individual?
What is the typical intrapleural pressure value in a healthy individual?
Patients with pre-existing lung conditions are at risk for __________ pneumothorax.
Patients with pre-existing lung conditions are at risk for __________ pneumothorax.
Which of the following factors can contribute to the rupture of subpleural blebs?
Which of the following factors can contribute to the rupture of subpleural blebs?
Which of the following is a severe consequence of tension pneumothorax?
Which of the following is a severe consequence of tension pneumothorax?
Closed pneumothorax allows air to exit the pleural space during exhalation.
Closed pneumothorax allows air to exit the pleural space during exhalation.
What is a common diagnostic approach for immediate identification of tension pneumothorax?
What is a common diagnostic approach for immediate identification of tension pneumothorax?
Air entering the pleural cavity increases pressure and can lead to lung ______________.
Air entering the pleural cavity increases pressure and can lead to lung ______________.
Match the following symptoms to their corresponding pneumothorax condition:
Match the following symptoms to their corresponding pneumothorax condition:
What can cause an iatrogenic pneumothorax?
What can cause an iatrogenic pneumothorax?
The percussion note over a lung affected by pneumothorax is typically dull.
The percussion note over a lung affected by pneumothorax is typically dull.
What is one potential complication of pneumothorax?
What is one potential complication of pneumothorax?
A severe form of pneumothorax where pressure accumulation leads to lung collapse is known as ______________.
A severe form of pneumothorax where pressure accumulation leads to lung collapse is known as ______________.
Which imaging technique can confirm the presence of air in the pleural space?
Which imaging technique can confirm the presence of air in the pleural space?
What is a distinguishing feature of open pneumothorax?
What is a distinguishing feature of open pneumothorax?
Which type of pneumothorax is common in tall, thin, young males who smoke?
Which type of pneumothorax is common in tall, thin, young males who smoke?
A tension pneumothorax compresses the inferior vena cava, leading to decreased venous return.
A tension pneumothorax compresses the inferior vena cava, leading to decreased venous return.
A pleural cavity normally has positive pressure compared to intrapulmonary pressure.
A pleural cavity normally has positive pressure compared to intrapulmonary pressure.
What condition is characterized by necrotic lung tissue and cavitary lesions?
What condition is characterized by necrotic lung tissue and cavitary lesions?
The presence of air in the pleural cavity increases __________, leading to lung collapse.
The presence of air in the pleural cavity increases __________, leading to lung collapse.
What physiological change occurs in intrapleural pressure during lung collapse?
What physiological change occurs in intrapleural pressure during lung collapse?
Match the following symptoms with their corresponding pneumothorax type:
Match the following symptoms with their corresponding pneumothorax type:
Air entering the pleural space through a defect in lung tissue is known as __________ pneumothorax.
Air entering the pleural space through a defect in lung tissue is known as __________ pneumothorax.
Match the following conditions to their associated characteristics:
Match the following conditions to their associated characteristics:
Which procedure could potentially lead to an iatrogenic pneumothorax?
Which procedure could potentially lead to an iatrogenic pneumothorax?
What is a potential risk factor for developing a secondary spontaneous pneumothorax?
What is a potential risk factor for developing a secondary spontaneous pneumothorax?
Patients with a small pneumothorax may be completely asymptomatic.
Patients with a small pneumothorax may be completely asymptomatic.
Subpleural blebs can rupture during activities like the Valsalva maneuver, leading to pneumothorax.
Subpleural blebs can rupture during activities like the Valsalva maneuver, leading to pneumothorax.
What is one potential complication of pneumothorax?
What is one potential complication of pneumothorax?
Identify one common cause of air entering the pleural space.
Identify one common cause of air entering the pleural space.
Decreased vascular return is often accompanied by __________ in response to cardiac output reduction due to tension pneumothorax.
Decreased vascular return is often accompanied by __________ in response to cardiac output reduction due to tension pneumothorax.
The pleura that is attached to the lung tissue is known as the __________ pleura.
The pleura that is attached to the lung tissue is known as the __________ pleura.
Which imaging technique is most commonly used to diagnose pneumothorax?
Which imaging technique is most commonly used to diagnose pneumothorax?
What condition is characterized by the presence of air in the pleural cavity?
What condition is characterized by the presence of air in the pleural cavity?
What is a common risk factor for spontaneous pneumothorax?
What is a common risk factor for spontaneous pneumothorax?
Elderly patients are the primary demographic affected by primary spontaneous pneumothorax.
Elderly patients are the primary demographic affected by primary spontaneous pneumothorax.
What happens to intrapleural pressure during lung collapse?
What happens to intrapleural pressure during lung collapse?
The pleural cavity normally contains __________ fluid for lubrication.
The pleural cavity normally contains __________ fluid for lubrication.
Match the following types of pneumothorax with their descriptions:
Match the following types of pneumothorax with their descriptions:
Which of the following lung conditions can lead to secondary spontaneous pneumothorax?
Which of the following lung conditions can lead to secondary spontaneous pneumothorax?
The visceral pleura is attached to the lung tissue.
The visceral pleura is attached to the lung tissue.
What physiological mechanism aids lung inflation?
What physiological mechanism aids lung inflation?
Tall, thin, young males who smoke are at risk for __________ pneumothorax.
Tall, thin, young males who smoke are at risk for __________ pneumothorax.
What physical activity can lead to the rupture of subpleural blebs?
What physical activity can lead to the rupture of subpleural blebs?
Which of the following is a common cause of tension pneumothorax?
Which of the following is a common cause of tension pneumothorax?
A closed pneumothorax allows air to exit the pleural space during exhalation.
A closed pneumothorax allows air to exit the pleural space during exhalation.
What is the primary risk associated with untreated tension pneumothorax?
What is the primary risk associated with untreated tension pneumothorax?
Pneumothorax can result in __________, which is characterized by a reduction in oxygen intake.
Pneumothorax can result in __________, which is characterized by a reduction in oxygen intake.
Match the following symptoms to their corresponding pneumothorax condition:
Match the following symptoms to their corresponding pneumothorax condition:
What imaging technique is best for confirming the presence of air in the pleural space?
What imaging technique is best for confirming the presence of air in the pleural space?
Hyper-resonance noted in percussion suggests the presence of pneumothorax.
Hyper-resonance noted in percussion suggests the presence of pneumothorax.
Name two potential complications of pneumothorax.
Name two potential complications of pneumothorax.
The clinical feature characterized by a drop in blood pressure during inspiration due to pneumothorax is known as __________.
The clinical feature characterized by a drop in blood pressure during inspiration due to pneumothorax is known as __________.
Which of the following is NOT a factor leading to pneumothorax?
Which of the following is NOT a factor leading to pneumothorax?
What type of pneumothorax is most likely to occur in tall, thin, young males?
What type of pneumothorax is most likely to occur in tall, thin, young males?
Accumulation of air in the pleural cavity can increase the pressure to a positive value.
Accumulation of air in the pleural cavity can increase the pressure to a positive value.
What is one physiological role of the pleural cavity?
What is one physiological role of the pleural cavity?
Tall and thin individuals often have a higher risk of developing __________ pneumothorax.
Tall and thin individuals often have a higher risk of developing __________ pneumothorax.
Which condition is a common risk factor for secondary spontaneous pneumothorax?
Which condition is a common risk factor for secondary spontaneous pneumothorax?
Match the type of pneumothorax with its correct description.
Match the type of pneumothorax with its correct description.
Spontaneous pneumothorax can occur in individuals with pre-existing lung conditions.
Spontaneous pneumothorax can occur in individuals with pre-existing lung conditions.
What is the typical intrapleural pressure in a healthy individual?
What is the typical intrapleural pressure in a healthy individual?
Which of the following factors may contribute to the rupture of subpleural blebs?
Which of the following factors may contribute to the rupture of subpleural blebs?
Air can enter the pleural space through a breach in the chest wall or a __________ in lung tissue.
Air can enter the pleural space through a breach in the chest wall or a __________ in lung tissue.
What is a common symptom of pneumothorax?
What is a common symptom of pneumothorax?
Closed pneumothorax allows air to exit the pleural space during exhalation.
Closed pneumothorax allows air to exit the pleural space during exhalation.
Name one common cause of tension pneumothorax.
Name one common cause of tension pneumothorax.
The presence of air in the pleural cavity can lead to lung __________.
The presence of air in the pleural cavity can lead to lung __________.
Match the following conditions with their characteristic features:
Match the following conditions with their characteristic features:
Which diagnostic approach is essential for immediate identification of tension pneumothorax?
Which diagnostic approach is essential for immediate identification of tension pneumothorax?
Percussion over a pneumothorax typically produces a dull sound.
Percussion over a pneumothorax typically produces a dull sound.
What happens to venous return during tension pneumothorax?
What happens to venous return during tension pneumothorax?
A significant condition associated with necrotic lung tissue is __________.
A significant condition associated with necrotic lung tissue is __________.
Increased heart rate during tension pneumothorax is a compensatory mechanism to maintain what?
Increased heart rate during tension pneumothorax is a compensatory mechanism to maintain what?
Flashcards are hidden until you start studying
Study Notes
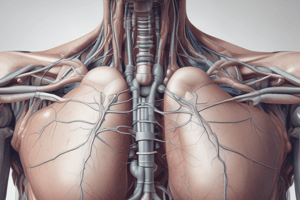
Pneumothorax Overview
- Pneumothorax is defined as the presence of air in the pleural cavity, leading to increased pressure and potential lung collapse.
- The pleural cavity normally contains serous fluid, providing lubrication between two pleural layers: the parietal pleura (attached to the chest wall) and the visceral pleura (attached to lung tissue).
- Under normal conditions, the intrapleural pressure is negative compared to intrapulmonary pressure, facilitating lung expansion during respiration.
Physiological Mechanism
- Intrapleural pressure typically maintains a negative value (approximately -4 mmHg), aiding lung inflation.
- Accumulation of air in the pleural space can convert this pressure to positive, making it greater than the intrapulmonary pressure, resulting in lung collapse.
Causes of Pneumothorax
- Air can enter the pleural space through:
- A breach in the chest wall (traumatic).
- A defect in lung tissue (spontaneous).
Types of Pneumothorax
-
Spontaneous Pneumothorax:
- Primary: Occurs in individuals without underlying lung disease, often seen in tall, thin, young males who smoke, or individuals with Marfan syndrome.
- Secondary: Occurs in patients with pre-existing lung conditions causing air accumulation.
-
Traumatic Pneumothorax: Results from physical injury to the chest wall leading to air entry.
Risk Factors for Spontaneous Pneumothorax
- Tall, thin, young males, typically smokers.
- Associated with Marfan syndrome due to the structural weakness of lung tissue.
- Development of subpleural blebs (air-filled sacs) which can rupture from pressure changes during activities like Valsalva maneuver.
Secondary Spontaneous Pneumothorax Conditions
-
Obstructive lung diseases, leading to hyperinflation, including:
- Emphysema: Loss of connective tissue causing air trapping.
- Chronic Bronchitis: Excess mucus obstructing airways.
- Asthma: Edema and inflammation narrowing airways.
- Cystic Fibrosis: Mucus plugging leading to bronchiectasis.
-
Destructive lesions in lung tissue can also lead to pneumothorax:
- Tuberculosis: Causes necrotic lung tissue and cavitary lesions.
- Pneumocystis pneumonia (PCP) in immunocompromised patients.
- Lung abscesses or malignancies (such as squamous cell carcinoma) can rupture and allow air leakage.
Traumatic Pneumothorax Etiologies
- Caused by trauma leading to a break in the chest wall.
- Can result from accidents, falls, or penetrating injuries, allowing air to enter the pleural space.
Key Takeaways
- Pneumothorax represents a serious alteration in pleural pressure dynamics that can lead to respiratory distress.
- Understanding the differences between types and causes is crucial for diagnosis and management.
- Risk identification, particularly in spontaneous cases, is essential for prevention strategies.### Types of Pneumothorax
- Open Pneumothorax: Caused by a defect in the chest wall allowing air to enter and exit during breathing; can lead to a "sucking" chest wound.
- Closed Pneumothorax: Occurs when air enters the pleural space through a break in the chest wall but does not exit during exhalation, similar to a one-way valve.
Causes of Pneumothorax
- Iatrogenic Causes: Resulting from medical procedures like:
- Subclavian central line placement
- Thoracentesis (draining a pleural effusion)
- Pleural biopsies
- High-pressure mechanical ventilation (can cause barotrauma)
- Inadvertent rib fractures during CPR
- Non-Iatrogenic Causes: Includes trauma from:
- Motor vehicle accidents
- Bullet or stab wounds
- Falls causing rib fractures
Pathophysiology of Pneumothorax
- Presence of air in the pleural cavity increases pressure, disrupting normal negative pressure and leading to lung collapse.
- Collapsed lung reduces oxygen intake, resulting in hypoxemia.
- Decreased ventilation with normal perfusion (V/Q mismatch) characterizes pneumothorax, leading to compromised gas exchange.
Symptoms and Clinical Manifestations
- Patients may be asymptomatic if the pneumothorax is small.
- Common symptoms:
- Dyspnea (shortness of breath)
- Pleuritic chest pain (sharp pain upon breathing)
- Physical exam findings:
- Decreased or absent breath sounds on the affected side
- Hyper-resonant percussion note over the pneumothorax
- Decreased tactile fremitus
- Possible signs of subcutaneous emphysema (air trapped in subcutaneous tissue)
Diagnosis Indicators
- Percussion Note: Hyper-resonance can indicate pneumothorax.
- Tactile Fremitus: Decreased vibrations felt on palpation due to air in the pleural space.
Tension Pneumothorax
- A severe form of pneumothorax where pressure accumulation leads to lung collapse and shifts mediastinal structures.
- Affects venous return:
- Compression of the superior vena cava reduces venous return to the heart, risking cardiac output and blood pressure.
- Body compensates with:
- Increased respiratory rate (tachypnea) due to hypoxemia.
- Increased heart rate (tachycardia) in an attempt to maintain blood pressure and perfusion.
Complications of Pneumothorax
- Significant hypoxemia can develop due to lung collapse.
- Potential for cardiac complications from decreased venous return.
- Watch for jugular venous distention as a sign of impaired venous return.
Summary
- Pneumothorax can be classified into open and closed types based on airflow dynamics in the pleural cavity.
- Iatrogenic and non-iatrogenic causes highlight the importance of awareness in clinical practice.
- Symptoms correlate with mechanical impairment of lung function, and timely diagnosis is critical for management to prevent complications like tension pneumothorax.### Hemodynamic Effects of Tension Pneumothorax
- Compression of the inferior vena cava (IVC) reduces venous return, leading to decreased stroke volume, cardiac output, and blood pressure.
- Compression of the superior vena cava (SVC) can result in jugular venous distension (JVD) and further decrease venous return.
- Right ventricular compression decreases preload, affecting stroke volume and cardiac output, contributing to hypotension.
- Significant tension pneumothorax compresses the right ventricle, leading to leftward bowing of the interventricular septum during inspiration, worsening cardiac output.
Pulsus Paradoxus
- Occurs when there is a drop of 10-20 mmHg in blood pressure during inspiration, caused by septal bowing and increased left ventricular afterload.
Compensatory Mechanisms
- Decreased systolic blood pressure from right ventricular output reduction leads to reflex tachycardia.
- Hypoxemia can develop due to the collapse of alveoli, initiating a series of compensatory cardiovascular responses.
Clinical Features of Tension Pneumothorax
- Symptoms include tachycardia, hypotension, decreased breath sounds, tracheal deviation, and JVD.
Diagnostic Approaches
- Immediate clinical diagnosis is essential for tension pneumothorax, based on symptomatology rather than waiting for imaging.
- Chest X-ray, lung ultrasound, and chest CT can help diagnose pneumothorax but should not delay treatment for tension pneumothorax.
Imaging Characteristics
- Chest X-ray: Look for hyperlucency and absence of lung markings in the affected hemithorax indicating pneumothorax.
- Ultrasound: Absence of lung sliding suggests pneumothorax, indicated by the pleural line separating visceral from parietal pleura.
- CT Scan: Provides detailed visualization, confirming the presence of air in the pleural space and assessing size.
Management Strategies
- Supportive Therapy: All patients with pneumothorax should receive supplemental high-flow oxygen to facilitate nitrogen absorption from the pleural space, promoting resorption of pneumothorax.
- Unstable Patients: Those with tension pneumothorax, bilateral pneumothorax, or under mechanical ventilation require immediate intervention.
Emergency Interventions
- For unstable patients, perform needle decompression in the second intercostal space to relieve pressure.
- Needle decompression allows trapped air to escape, equalizing pleural pressure and improving hemodynamics.
Summary of Key Takeaways
- Tension pneumothorax critically impacts hemodynamics.
- Immediate clinical diagnosis and treatment are paramount.
- Supplemental oxygen aids in nitrogen resorption facilitating recovery.
- Recognize imaging features as important adjuncts to diagnosis while prioritizing direct interventions.
Pneumothorax Overview
- Pneumothorax refers to air accumulation in the pleural cavity, leading to increased pressure and potential lung collapse.
- The pleural cavity usually contains serous fluid, providing lubrication between the parietal pleura (chest wall) and visceral pleura (lung tissue).
- Normal intrapleural pressure is negative, aiding lung expansion during breathing.
Physiological Mechanism
- Typical intrapleural pressure is around -4 mmHg, essential for lung inflation.
- Air accumulation can result in positive intrapleural pressure, surpassing intrapulmonary pressure and causing lung collapse.
Causes of Pneumothorax
- Air may enter the pleural space due to:
- Traumatic breaches in the chest wall.
- Spontaneous defects in lung tissue.
Types of Pneumothorax
- Spontaneous Pneumothorax:
- Primary: Occurs in healthy individuals, often in tall, thin young males, smokers, or those with Marfan syndrome.
- Secondary: Associated with existing lung conditions that lead to air accumulation.
- Traumatic Pneumothorax: Results from physical injury to the chest wall.
Risk Factors for Spontaneous Pneumothorax
- Predominantly affects tall, thin young males, especially smokers.
- Linked to Marfan syndrome due to lung tissue structural weaknesses.
- Consideration of subpleural blebs which can rupture during physical stress (e.g. Valsalva maneuver).
Secondary Spontaneous Pneumothorax Conditions
- Associated with obstructive lung diseases causing hyperinflation such as:
- Emphysema: Air trapping due to connective tissue loss.
- Chronic Bronchitis: Obstruction caused by excessive mucus.
- Asthma: Narrowing due to edema and inflammation.
- Cystic Fibrosis: Mucus plugging leading to bronchiectasis.
- Destructive lesions from conditions like tuberculosis or lung abscesses can also lead to pneumothorax.
Traumatic Pneumothorax Etiologies
- Occurs from trauma resulting in damage to the chest wall.
- Can result from various incidents, including falls or penetrating injuries.
Key Takeaways
- Pneumothorax alters pleural pressure dynamics, potentially leading to respiratory distress.
- Understanding the nuances between types and causes is crucial for effective diagnosis and management.
- Identifying risk factors, particularly in spontaneous pneumothorax, is critical for prevention.
Types of Pneumothorax
- Open Pneumothorax: Air enters and exits during breathing, resembling a "sucking" chest wound.
- Closed Pneumothorax: Air enters through the chest wall but does not exit during exhalation, acting like a one-way valve.
Causes of Pneumothorax
- Iatrogenic: Occurs from medical procedures such as central line placement or thoracentesis.
- Non-Iatrogenic: Originates from accidents, e.g., motor vehicle crashes or stab wounds.
Pathophysiology of Pneumothorax
- Air presence disrupts negative pleural pressure, leading to lung collapse and reduced oxygen intake (hypoxemia).
- Affects ventilation, causing V/Q mismatch that compromises gas exchange.
Symptoms and Clinical Manifestations
- Small pneumothoraces may be asymptomatic, while larger cases often exhibit:
- Dyspnea (shortness of breath).
- Pleuritic chest pain.
- Examination may reveal:
- Decreased breath sounds and hyper-resonance over affected areas.
Diagnosis Indicators
- Percussion Note: Hyper-resonance can suggest pneumothorax.
- Tactile Fremitus: Reduced vibrations felt during palpation indicate air in the pleural space.
Tension Pneumothorax
- Life-threatening condition where pressure buildup leads to lung collapse and mediastinal displacement.
- It compresses the superior vena cava, reducing venous return, potentially risking cardiac output.
- Compensatory responses include increased respiratory and heart rates.
Complications of Pneumothorax
- Significant hypoxemia may ensue.
- Cardiac complications can arise from impaired venous return; jugular venous distention may signal issues.
Clinical Features of Tension Pneumothorax
- Symptoms include tachycardia, hypotension, decreased breath sounds, tracheal deviation, and JVD.
Diagnostic Approaches
- Immediate clinical assessment is crucial for tension pneumothorax; imaging should not delay treatment.
- Imaging techniques include chest X-ray, ultrasound, and CT scan for confirmation and evaluation.
Imaging Characteristics
- Chest X-ray: Hyperlucency and absence of lung markings on the affected side indicate pneumothorax.
- Ultrasound: Lack of lung sliding denotes pneumothorax.
- CT Scan: Provides detailed visualization of air in the pleural space.
Management Strategies
- Supportive Therapy: Oxygen therapy facilitates nitrogen absorption, assisting pneumothorax resolution.
- Unstable Patients: Require immediate intervention such as needle decompression to relieve pressure.
Emergency Interventions
- Perform needle decompression in the second intercostal space for unstable patients to normalize pleural pressure and improve hemodynamics.
Summary of Key Takeaways
- Tension pneumothorax poses significant hemodynamic risk, necessitating prompt diagnosis and intervention.
- Supplemental oxygen can aid in recovery through nitrogen resorption.
- Awareness of imaging features complements clinical assessment but should not defer urgent treatment.
Pneumothorax Overview
- Pneumothorax refers to air accumulation in the pleural cavity, leading to increased pressure and potential lung collapse.
- The pleural cavity usually contains serous fluid, providing lubrication between the parietal pleura (chest wall) and visceral pleura (lung tissue).
- Normal intrapleural pressure is negative, aiding lung expansion during breathing.
Physiological Mechanism
- Typical intrapleural pressure is around -4 mmHg, essential for lung inflation.
- Air accumulation can result in positive intrapleural pressure, surpassing intrapulmonary pressure and causing lung collapse.
Causes of Pneumothorax
- Air may enter the pleural space due to:
- Traumatic breaches in the chest wall.
- Spontaneous defects in lung tissue.
Types of Pneumothorax
- Spontaneous Pneumothorax:
- Primary: Occurs in healthy individuals, often in tall, thin young males, smokers, or those with Marfan syndrome.
- Secondary: Associated with existing lung conditions that lead to air accumulation.
- Traumatic Pneumothorax: Results from physical injury to the chest wall.
Risk Factors for Spontaneous Pneumothorax
- Predominantly affects tall, thin young males, especially smokers.
- Linked to Marfan syndrome due to lung tissue structural weaknesses.
- Consideration of subpleural blebs which can rupture during physical stress (e.g. Valsalva maneuver).
Secondary Spontaneous Pneumothorax Conditions
- Associated with obstructive lung diseases causing hyperinflation such as:
- Emphysema: Air trapping due to connective tissue loss.
- Chronic Bronchitis: Obstruction caused by excessive mucus.
- Asthma: Narrowing due to edema and inflammation.
- Cystic Fibrosis: Mucus plugging leading to bronchiectasis.
- Destructive lesions from conditions like tuberculosis or lung abscesses can also lead to pneumothorax.
Traumatic Pneumothorax Etiologies
- Occurs from trauma resulting in damage to the chest wall.
- Can result from various incidents, including falls or penetrating injuries.
Key Takeaways
- Pneumothorax alters pleural pressure dynamics, potentially leading to respiratory distress.
- Understanding the nuances between types and causes is crucial for effective diagnosis and management.
- Identifying risk factors, particularly in spontaneous pneumothorax, is critical for prevention.
Types of Pneumothorax
- Open Pneumothorax: Air enters and exits during breathing, resembling a "sucking" chest wound.
- Closed Pneumothorax: Air enters through the chest wall but does not exit during exhalation, acting like a one-way valve.
Causes of Pneumothorax
- Iatrogenic: Occurs from medical procedures such as central line placement or thoracentesis.
- Non-Iatrogenic: Originates from accidents, e.g., motor vehicle crashes or stab wounds.
Pathophysiology of Pneumothorax
- Air presence disrupts negative pleural pressure, leading to lung collapse and reduced oxygen intake (hypoxemia).
- Affects ventilation, causing V/Q mismatch that compromises gas exchange.
Symptoms and Clinical Manifestations
- Small pneumothoraces may be asymptomatic, while larger cases often exhibit:
- Dyspnea (shortness of breath).
- Pleuritic chest pain.
- Examination may reveal:
- Decreased breath sounds and hyper-resonance over affected areas.
Diagnosis Indicators
- Percussion Note: Hyper-resonance can suggest pneumothorax.
- Tactile Fremitus: Reduced vibrations felt during palpation indicate air in the pleural space.
Tension Pneumothorax
- Life-threatening condition where pressure buildup leads to lung collapse and mediastinal displacement.
- It compresses the superior vena cava, reducing venous return, potentially risking cardiac output.
- Compensatory responses include increased respiratory and heart rates.
Complications of Pneumothorax
- Significant hypoxemia may ensue.
- Cardiac complications can arise from impaired venous return; jugular venous distention may signal issues.
Clinical Features of Tension Pneumothorax
- Symptoms include tachycardia, hypotension, decreased breath sounds, tracheal deviation, and JVD.
Diagnostic Approaches
- Immediate clinical assessment is crucial for tension pneumothorax; imaging should not delay treatment.
- Imaging techniques include chest X-ray, ultrasound, and CT scan for confirmation and evaluation.
Imaging Characteristics
- Chest X-ray: Hyperlucency and absence of lung markings on the affected side indicate pneumothorax.
- Ultrasound: Lack of lung sliding denotes pneumothorax.
- CT Scan: Provides detailed visualization of air in the pleural space.
Management Strategies
- Supportive Therapy: Oxygen therapy facilitates nitrogen absorption, assisting pneumothorax resolution.
- Unstable Patients: Require immediate intervention such as needle decompression to relieve pressure.
Emergency Interventions
- Perform needle decompression in the second intercostal space for unstable patients to normalize pleural pressure and improve hemodynamics.
Summary of Key Takeaways
- Tension pneumothorax poses significant hemodynamic risk, necessitating prompt diagnosis and intervention.
- Supplemental oxygen can aid in recovery through nitrogen resorption.
- Awareness of imaging features complements clinical assessment but should not defer urgent treatment.
Pneumothorax Overview
- Pneumothorax refers to air accumulation in the pleural cavity, leading to increased pressure and potential lung collapse.
- The pleural cavity usually contains serous fluid, providing lubrication between the parietal pleura (chest wall) and visceral pleura (lung tissue).
- Normal intrapleural pressure is negative, aiding lung expansion during breathing.
Physiological Mechanism
- Typical intrapleural pressure is around -4 mmHg, essential for lung inflation.
- Air accumulation can result in positive intrapleural pressure, surpassing intrapulmonary pressure and causing lung collapse.
Causes of Pneumothorax
- Air may enter the pleural space due to:
- Traumatic breaches in the chest wall.
- Spontaneous defects in lung tissue.
Types of Pneumothorax
- Spontaneous Pneumothorax:
- Primary: Occurs in healthy individuals, often in tall, thin young males, smokers, or those with Marfan syndrome.
- Secondary: Associated with existing lung conditions that lead to air accumulation.
- Traumatic Pneumothorax: Results from physical injury to the chest wall.
Risk Factors for Spontaneous Pneumothorax
- Predominantly affects tall, thin young males, especially smokers.
- Linked to Marfan syndrome due to lung tissue structural weaknesses.
- Consideration of subpleural blebs which can rupture during physical stress (e.g. Valsalva maneuver).
Secondary Spontaneous Pneumothorax Conditions
- Associated with obstructive lung diseases causing hyperinflation such as:
- Emphysema: Air trapping due to connective tissue loss.
- Chronic Bronchitis: Obstruction caused by excessive mucus.
- Asthma: Narrowing due to edema and inflammation.
- Cystic Fibrosis: Mucus plugging leading to bronchiectasis.
- Destructive lesions from conditions like tuberculosis or lung abscesses can also lead to pneumothorax.
Traumatic Pneumothorax Etiologies
- Occurs from trauma resulting in damage to the chest wall.
- Can result from various incidents, including falls or penetrating injuries.
Key Takeaways
- Pneumothorax alters pleural pressure dynamics, potentially leading to respiratory distress.
- Understanding the nuances between types and causes is crucial for effective diagnosis and management.
- Identifying risk factors, particularly in spontaneous pneumothorax, is critical for prevention.
Types of Pneumothorax
- Open Pneumothorax: Air enters and exits during breathing, resembling a "sucking" chest wound.
- Closed Pneumothorax: Air enters through the chest wall but does not exit during exhalation, acting like a one-way valve.
Causes of Pneumothorax
- Iatrogenic: Occurs from medical procedures such as central line placement or thoracentesis.
- Non-Iatrogenic: Originates from accidents, e.g., motor vehicle crashes or stab wounds.
Pathophysiology of Pneumothorax
- Air presence disrupts negative pleural pressure, leading to lung collapse and reduced oxygen intake (hypoxemia).
- Affects ventilation, causing V/Q mismatch that compromises gas exchange.
Symptoms and Clinical Manifestations
- Small pneumothoraces may be asymptomatic, while larger cases often exhibit:
- Dyspnea (shortness of breath).
- Pleuritic chest pain.
- Examination may reveal:
- Decreased breath sounds and hyper-resonance over affected areas.
Diagnosis Indicators
- Percussion Note: Hyper-resonance can suggest pneumothorax.
- Tactile Fremitus: Reduced vibrations felt during palpation indicate air in the pleural space.
Tension Pneumothorax
- Life-threatening condition where pressure buildup leads to lung collapse and mediastinal displacement.
- It compresses the superior vena cava, reducing venous return, potentially risking cardiac output.
- Compensatory responses include increased respiratory and heart rates.
Complications of Pneumothorax
- Significant hypoxemia may ensue.
- Cardiac complications can arise from impaired venous return; jugular venous distention may signal issues.
Clinical Features of Tension Pneumothorax
- Symptoms include tachycardia, hypotension, decreased breath sounds, tracheal deviation, and JVD.
Diagnostic Approaches
- Immediate clinical assessment is crucial for tension pneumothorax; imaging should not delay treatment.
- Imaging techniques include chest X-ray, ultrasound, and CT scan for confirmation and evaluation.
Imaging Characteristics
- Chest X-ray: Hyperlucency and absence of lung markings on the affected side indicate pneumothorax.
- Ultrasound: Lack of lung sliding denotes pneumothorax.
- CT Scan: Provides detailed visualization of air in the pleural space.
Management Strategies
- Supportive Therapy: Oxygen therapy facilitates nitrogen absorption, assisting pneumothorax resolution.
- Unstable Patients: Require immediate intervention such as needle decompression to relieve pressure.
Emergency Interventions
- Perform needle decompression in the second intercostal space for unstable patients to normalize pleural pressure and improve hemodynamics.
Summary of Key Takeaways
- Tension pneumothorax poses significant hemodynamic risk, necessitating prompt diagnosis and intervention.
- Supplemental oxygen can aid in recovery through nitrogen resorption.
- Awareness of imaging features complements clinical assessment but should not defer urgent treatment.
Pneumothorax Overview
- Pneumothorax refers to air accumulation in the pleural cavity, leading to increased pressure and potential lung collapse.
- The pleural cavity usually contains serous fluid, providing lubrication between the parietal pleura (chest wall) and visceral pleura (lung tissue).
- Normal intrapleural pressure is negative, aiding lung expansion during breathing.
Physiological Mechanism
- Typical intrapleural pressure is around -4 mmHg, essential for lung inflation.
- Air accumulation can result in positive intrapleural pressure, surpassing intrapulmonary pressure and causing lung collapse.
Causes of Pneumothorax
- Air may enter the pleural space due to:
- Traumatic breaches in the chest wall.
- Spontaneous defects in lung tissue.
Types of Pneumothorax
- Spontaneous Pneumothorax:
- Primary: Occurs in healthy individuals, often in tall, thin young males, smokers, or those with Marfan syndrome.
- Secondary: Associated with existing lung conditions that lead to air accumulation.
- Traumatic Pneumothorax: Results from physical injury to the chest wall.
Risk Factors for Spontaneous Pneumothorax
- Predominantly affects tall, thin young males, especially smokers.
- Linked to Marfan syndrome due to lung tissue structural weaknesses.
- Consideration of subpleural blebs which can rupture during physical stress (e.g. Valsalva maneuver).
Secondary Spontaneous Pneumothorax Conditions
- Associated with obstructive lung diseases causing hyperinflation such as:
- Emphysema: Air trapping due to connective tissue loss.
- Chronic Bronchitis: Obstruction caused by excessive mucus.
- Asthma: Narrowing due to edema and inflammation.
- Cystic Fibrosis: Mucus plugging leading to bronchiectasis.
- Destructive lesions from conditions like tuberculosis or lung abscesses can also lead to pneumothorax.
Traumatic Pneumothorax Etiologies
- Occurs from trauma resulting in damage to the chest wall.
- Can result from various incidents, including falls or penetrating injuries.
Key Takeaways
- Pneumothorax alters pleural pressure dynamics, potentially leading to respiratory distress.
- Understanding the nuances between types and causes is crucial for effective diagnosis and management.
- Identifying risk factors, particularly in spontaneous pneumothorax, is critical for prevention.
Types of Pneumothorax
- Open Pneumothorax: Air enters and exits during breathing, resembling a "sucking" chest wound.
- Closed Pneumothorax: Air enters through the chest wall but does not exit during exhalation, acting like a one-way valve.
Causes of Pneumothorax
- Iatrogenic: Occurs from medical procedures such as central line placement or thoracentesis.
- Non-Iatrogenic: Originates from accidents, e.g., motor vehicle crashes or stab wounds.
Pathophysiology of Pneumothorax
- Air presence disrupts negative pleural pressure, leading to lung collapse and reduced oxygen intake (hypoxemia).
- Affects ventilation, causing V/Q mismatch that compromises gas exchange.
Symptoms and Clinical Manifestations
- Small pneumothoraces may be asymptomatic, while larger cases often exhibit:
- Dyspnea (shortness of breath).
- Pleuritic chest pain.
- Examination may reveal:
- Decreased breath sounds and hyper-resonance over affected areas.
Diagnosis Indicators
- Percussion Note: Hyper-resonance can suggest pneumothorax.
- Tactile Fremitus: Reduced vibrations felt during palpation indicate air in the pleural space.
Tension Pneumothorax
- Life-threatening condition where pressure buildup leads to lung collapse and mediastinal displacement.
- It compresses the superior vena cava, reducing venous return, potentially risking cardiac output.
- Compensatory responses include increased respiratory and heart rates.
Complications of Pneumothorax
- Significant hypoxemia may ensue.
- Cardiac complications can arise from impaired venous return; jugular venous distention may signal issues.
Clinical Features of Tension Pneumothorax
- Symptoms include tachycardia, hypotension, decreased breath sounds, tracheal deviation, and JVD.
Diagnostic Approaches
- Immediate clinical assessment is crucial for tension pneumothorax; imaging should not delay treatment.
- Imaging techniques include chest X-ray, ultrasound, and CT scan for confirmation and evaluation.
Imaging Characteristics
- Chest X-ray: Hyperlucency and absence of lung markings on the affected side indicate pneumothorax.
- Ultrasound: Lack of lung sliding denotes pneumothorax.
- CT Scan: Provides detailed visualization of air in the pleural space.
Management Strategies
- Supportive Therapy: Oxygen therapy facilitates nitrogen absorption, assisting pneumothorax resolution.
- Unstable Patients: Require immediate intervention such as needle decompression to relieve pressure.
Emergency Interventions
- Perform needle decompression in the second intercostal space for unstable patients to normalize pleural pressure and improve hemodynamics.
Summary of Key Takeaways
- Tension pneumothorax poses significant hemodynamic risk, necessitating prompt diagnosis and intervention.
- Supplemental oxygen can aid in recovery through nitrogen resorption.
- Awareness of imaging features complements clinical assessment but should not defer urgent treatment.
Pneumothorax Overview
- Pneumothorax refers to air accumulation in the pleural cavity, leading to increased pressure and potential lung collapse.
- The pleural cavity usually contains serous fluid, providing lubrication between the parietal pleura (chest wall) and visceral pleura (lung tissue).
- Normal intrapleural pressure is negative, aiding lung expansion during breathing.
Physiological Mechanism
- Typical intrapleural pressure is around -4 mmHg, essential for lung inflation.
- Air accumulation can result in positive intrapleural pressure, surpassing intrapulmonary pressure and causing lung collapse.
Causes of Pneumothorax
- Air may enter the pleural space due to:
- Traumatic breaches in the chest wall.
- Spontaneous defects in lung tissue.
Types of Pneumothorax
- Spontaneous Pneumothorax:
- Primary: Occurs in healthy individuals, often in tall, thin young males, smokers, or those with Marfan syndrome.
- Secondary: Associated with existing lung conditions that lead to air accumulation.
- Traumatic Pneumothorax: Results from physical injury to the chest wall.
Risk Factors for Spontaneous Pneumothorax
- Predominantly affects tall, thin young males, especially smokers.
- Linked to Marfan syndrome due to lung tissue structural weaknesses.
- Consideration of subpleural blebs which can rupture during physical stress (e.g. Valsalva maneuver).
Secondary Spontaneous Pneumothorax Conditions
- Associated with obstructive lung diseases causing hyperinflation such as:
- Emphysema: Air trapping due to connective tissue loss.
- Chronic Bronchitis: Obstruction caused by excessive mucus.
- Asthma: Narrowing due to edema and inflammation.
- Cystic Fibrosis: Mucus plugging leading to bronchiectasis.
- Destructive lesions from conditions like tuberculosis or lung abscesses can also lead to pneumothorax.
Traumatic Pneumothorax Etiologies
- Occurs from trauma resulting in damage to the chest wall.
- Can result from various incidents, including falls or penetrating injuries.
Key Takeaways
- Pneumothorax alters pleural pressure dynamics, potentially leading to respiratory distress.
- Understanding the nuances between types and causes is crucial for effective diagnosis and management.
- Identifying risk factors, particularly in spontaneous pneumothorax, is critical for prevention.
Types of Pneumothorax
- Open Pneumothorax: Air enters and exits during breathing, resembling a "sucking" chest wound.
- Closed Pneumothorax: Air enters through the chest wall but does not exit during exhalation, acting like a one-way valve.
Causes of Pneumothorax
- Iatrogenic: Occurs from medical procedures such as central line placement or thoracentesis.
- Non-Iatrogenic: Originates from accidents, e.g., motor vehicle crashes or stab wounds.
Pathophysiology of Pneumothorax
- Air presence disrupts negative pleural pressure, leading to lung collapse and reduced oxygen intake (hypoxemia).
- Affects ventilation, causing V/Q mismatch that compromises gas exchange.
Symptoms and Clinical Manifestations
- Small pneumothoraces may be asymptomatic, while larger cases often exhibit:
- Dyspnea (shortness of breath).
- Pleuritic chest pain.
- Examination may reveal:
- Decreased breath sounds and hyper-resonance over affected areas.
Diagnosis Indicators
- Percussion Note: Hyper-resonance can suggest pneumothorax.
- Tactile Fremitus: Reduced vibrations felt during palpation indicate air in the pleural space.
Tension Pneumothorax
- Life-threatening condition where pressure buildup leads to lung collapse and mediastinal displacement.
- It compresses the superior vena cava, reducing venous return, potentially risking cardiac output.
- Compensatory responses include increased respiratory and heart rates.
Complications of Pneumothorax
- Significant hypoxemia may ensue.
- Cardiac complications can arise from impaired venous return; jugular venous distention may signal issues.
Clinical Features of Tension Pneumothorax
- Symptoms include tachycardia, hypotension, decreased breath sounds, tracheal deviation, and JVD.
Diagnostic Approaches
- Immediate clinical assessment is crucial for tension pneumothorax; imaging should not delay treatment.
- Imaging techniques include chest X-ray, ultrasound, and CT scan for confirmation and evaluation.
Imaging Characteristics
- Chest X-ray: Hyperlucency and absence of lung markings on the affected side indicate pneumothorax.
- Ultrasound: Lack of lung sliding denotes pneumothorax.
- CT Scan: Provides detailed visualization of air in the pleural space.
Management Strategies
- Supportive Therapy: Oxygen therapy facilitates nitrogen absorption, assisting pneumothorax resolution.
- Unstable Patients: Require immediate intervention such as needle decompression to relieve pressure.
Emergency Interventions
- Perform needle decompression in the second intercostal space for unstable patients to normalize pleural pressure and improve hemodynamics.
Summary of Key Takeaways
- Tension pneumothorax poses significant hemodynamic risk, necessitating prompt diagnosis and intervention.
- Supplemental oxygen can aid in recovery through nitrogen resorption.
- Awareness of imaging features complements clinical assessment but should not defer urgent treatment.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.