Podcast
Questions and Answers
What is the main reason for the pressure wave becoming larger as it moves down the arterial tree?
What is the main reason for the pressure wave becoming larger as it moves down the arterial tree?
- Due to the increase in arterial stiffness (correct)
- Due to the decrease in blood flow rate
- Due to the increase in blood cell velocity
- Due to the decrease in arterial stiffness
What is the approximate velocity of the blood cell in the aorta?
What is the approximate velocity of the blood cell in the aorta?
- 32 cm/s (correct)
- 25 cm/s
- 33 cm/s
- 5 m/s
What happens to the blood flow during systole?
What happens to the blood flow during systole?
- 25% of the stroke volume is pushed forward into the smaller arteries (correct)
- 75% of the stroke volume is pushed forward into the smaller arteries
- It is completely pushed forward into the smaller arteries
- It is completely stored in the aorta and large arteries
What is the main component of total peripheral resistance (TPR)?
What is the main component of total peripheral resistance (TPR)?
What happens to the pressure wave as it moves into the arterioles and microcirculation?
What happens to the pressure wave as it moves into the arterioles and microcirculation?
What is the approximate length of the aorta?
What is the approximate length of the aorta?
What happens to the flow during systole?
What happens to the flow during systole?
What is the characteristic of blood flow in the aorta and arteries?
What is the characteristic of blood flow in the aorta and arteries?
What is the primary reason for the development of the thrifty genotype in humans?
What is the primary reason for the development of the thrifty genotype in humans?
What is the primary consequence of eating too much salt?
What is the primary consequence of eating too much salt?
What would happen to plasma [Na+] if an individual started eating very little salt?
What would happen to plasma [Na+] if an individual started eating very little salt?
What is the primary function of ADH in response to changes in salt intake?
What is the primary function of ADH in response to changes in salt intake?
What is the primary driver of the human desire to consume salt?
What is the primary driver of the human desire to consume salt?
What is the ultimate consequence of the thrifty genotype in modern humans?
What is the ultimate consequence of the thrifty genotype in modern humans?
What is the main function of the Arterial Baroreflex?
What is the main function of the Arterial Baroreflex?
What is the primary mechanism by which the baroreflex responds to changes in blood pressure?
What is the primary mechanism by which the baroreflex responds to changes in blood pressure?
What is the main determinant of mean arterial blood pressure?
What is the main determinant of mean arterial blood pressure?
What is the role of the Renin-Angiotensin-Aldosterone System (RAAS) in regulating blood pressure?
What is the role of the Renin-Angiotensin-Aldosterone System (RAAS) in regulating blood pressure?
What is the primary mechanism by which the baroreflex regulates blood pressure?
What is the primary mechanism by which the baroreflex regulates blood pressure?
What is the normal range of systolic blood pressure measured using a sphygmomanometer?
What is the normal range of systolic blood pressure measured using a sphygmomanometer?
What is the effect of an increase in arterial blood pressure on the baroreflex?
What is the effect of an increase in arterial blood pressure on the baroreflex?
What is the formula for calculating mean blood pressure?
What is the formula for calculating mean blood pressure?
What is the role of the kidneys in long-term regulation of blood pressure?
What is the role of the kidneys in long-term regulation of blood pressure?
Where would you measure blood pressure to get the highest reading?
Where would you measure blood pressure to get the highest reading?
What is the effect of angiotensin II on blood pressure?
What is the effect of angiotensin II on blood pressure?
What is the term for the oscillation of blood pressure with the cardiac cycle?
What is the term for the oscillation of blood pressure with the cardiac cycle?
What is the mechanism that helps regulate mean blood pressure in the short-term?
What is the mechanism that helps regulate mean blood pressure in the short-term?
What is the role of pressure natriuresis in regulating blood pressure?
What is the role of pressure natriuresis in regulating blood pressure?
What is the primary way the kidneys regulate mean blood pressure in the long-term?
What is the primary way the kidneys regulate mean blood pressure in the long-term?
What is the primary determinant of extracellular fluid volume?
What is the primary determinant of extracellular fluid volume?
What is the term for the increased excretion of Na+ and water by the kidneys in response to high blood pressure?
What is the term for the increased excretion of Na+ and water by the kidneys in response to high blood pressure?
What is the typical measurement location for blood pressure using a sphygmomanometer?
What is the typical measurement location for blood pressure using a sphygmomanometer?
What is the effect of increased blood volume on atrial stretch receptors?
What is the effect of increased blood volume on atrial stretch receptors?
What is the effect of increased blood pressure on renal sodium excretion?
What is the effect of increased blood pressure on renal sodium excretion?
Which of the following is NOT a mechanism that contributes to long-term blood pressure control?
Which of the following is NOT a mechanism that contributes to long-term blood pressure control?
What is the effect of increased sympathetic nervous system (SNS) outflow to the kidney?
What is the effect of increased sympathetic nervous system (SNS) outflow to the kidney?
What is the role of the baroreceptor reflex in blood pressure control?
What is the role of the baroreceptor reflex in blood pressure control?
Why are vasodilators effective anti-hypertensive drugs?
Why are vasodilators effective anti-hypertensive drugs?
What is the effect of increased central venous pressure (CVP) on atrial stretch receptors?
What is the effect of increased central venous pressure (CVP) on atrial stretch receptors?
Which of the following is an alternative model of blood pressure control?
Which of the following is an alternative model of blood pressure control?
Flashcards are hidden until you start studying
Study Notes
Physiology and Anatomy of Systems
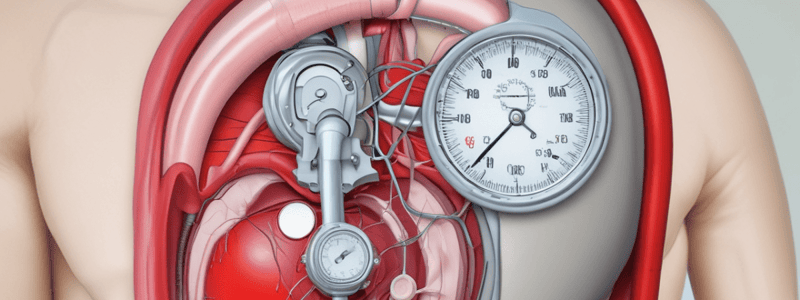
Blood Pressure - A Brief Review
- Blood pressure (BP) refers to the pressure in the large arteries, oscillating with the cardiac cycle
- BP is typically measured at the level of the heart in one arm using a sphygmomanometer
- Normal systolic and diastolic pressures are approximately 120/80 mmHg
- Mean BP is calculated as the time-weighted average of the systolic and diastolic blood pressures or 2/3 x DBP + 1/3 x SBP
Mechanisms Governing Pressure and Flow Waves in the Arteries
- Blood from the heart hits the aorta, causing pressure and flow waves propagated down the vascular system
- The pressure wave becomes larger as it moves down the arterial tree due to greater arterial stiffness
- Flow is progressively smoothed out as blood moves into the arterioles and the microcirculation
- Blood flow is pulsatile in the aorta and arteries, with pulse and pressure waves moving at approximately 5 m/s
- Blood cells move at approximately 32 cm/s, with an average aortic length of approximately 33 cm
Acute Regulation of Blood Pressure: Baroreceptor Reflex
- Baroreceptors contain fine nerve endings sensitive to stretch (mechanoreceptors)
- Decreased pressure causes decreased firing, most sensitive when mean BP is between 80-150 mmHg
- Sensitivity also increased by a large pulse pressure, with receptors showing adaptation
- Baroreceptors respond rapidly to changes in MAP and pulse pressure in the short-term
- The baroreflex responds rapidly to changes in MAP and pulse pressure, communicating via sympathetic/parasympathetic NS
Determinants of Mean Arterial Blood Pressure
- Baroreceptor reflex
- Arterial tone
- Total peripheral resistance
- Cardiac output (CO x TPR = BP)
- Heart rate and contractility (i.e., heart)
- Venous return (i.e., veins)
- Blood volume (i.e., kidneys)
Renin-Angiotensin-Aldosterone System (RAAS)
- RAAS activates vasoconstriction, increasing total peripheral resistance
- RAAS increases blood volume through sodium retention and potassium excretion
- RAAS also stimulates the release of aldosterone, promoting sodium reabsorption and potassium excretion in the kidneys
Regulation of Mean Arterial Blood Pressure by RAAS
- Various stimuli activate the RAAS, leading to increased renin release from juxtaglomerular cells
- Renin converts angiotensinogen to angiotensin I, which is then converted to angiotensin II by angiotensin-converting enzyme (ACE)
- Angiotensin II stimulates vasoconstriction, aldosterone release, and sodium reabsorption in the kidneys
Long-term Determinants of Mean Arterial Blood Pressure
- Stable body sodium content
- Stable extracellular fluid volume
- Stable plasma/blood volume
- Pressure natriuresis
Pressure Natriuresis
- Increased renal perfusion and medullary blood flow decrease angiotensin II production
- Increased nitric oxide, prostaglandins, and renal kinins stimulate natriuresis and diuresis
- Pressure natriuresis increases renal interstitial hydrostatic pressure, decreasing tubular sodium reabsorption and increasing sodium excretion
Long-term Regulation of Arterial Blood Pressure
- Stabilization of BP in the long term is mainly due to maintenance of a constant ECF volume
- ECF volume is controlled by the sodium concentration of the ECF
- Diseases of civilization, such as hypertension and type 2 diabetes, may be explained by the thrifty genotype hypothesis
- Human evolution has programmed us to crave and conserve nutritional resources, contributing to the development of hypertension and type 2 diabetes.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.