Podcast
Questions and Answers
What is the primary function of skeletal muscles related to posture?
What is the primary function of skeletal muscles related to posture?
- Static force production for maintaining posture (correct)
- Heat production
- Kinetic force production for locomotion
- Venous drainage
How does myosin interact with ATP during muscle contraction?
How does myosin interact with ATP during muscle contraction?
- It hydrolyzes ATP and uses the energy for contraction (correct)
- It solely binds to ATP without hydrolyzing it
- It stores ATP for later use
- It employs ATP for binding to actin only
Which component is involved in the flexing mechanism of myosin cross-bridges?
Which component is involved in the flexing mechanism of myosin cross-bridges?
- The ATP binding site on actin
- The amine terminal of actin
- The head structure of tropomyosin
- The hinges of the myosin protein (correct)
What role do tropomyosin molecules play in muscle contraction?
What role do tropomyosin molecules play in muscle contraction?
Which statement describes skeletal muscle tissue?
Which statement describes skeletal muscle tissue?
What is the primary function of Troponin-I in muscle contraction?
What is the primary function of Troponin-I in muscle contraction?
What percentage of the human body is comprised of skeletal muscles?
What percentage of the human body is comprised of skeletal muscles?
Where are T tubules located in mammalian skeletal muscle fibers?
Where are T tubules located in mammalian skeletal muscle fibers?
What is the characteristic feature of thin filament proteins?
What is the characteristic feature of thin filament proteins?
What role does calcium play in muscle contraction?
What role does calcium play in muscle contraction?
Which function does skeletal muscle NOT perform?
Which function does skeletal muscle NOT perform?
What is the function of the ryanodine receptor in the sarcoplasmic reticulum?
What is the function of the ryanodine receptor in the sarcoplasmic reticulum?
What structures make up the triad in skeletal muscle fibers?
What structures make up the triad in skeletal muscle fibers?
How does an action potential influence muscle fiber contraction?
How does an action potential influence muscle fiber contraction?
What is the role of the motor end plate in muscle contraction?
What is the role of the motor end plate in muscle contraction?
Which of the following components is NOT found in the structure of troponin?
Which of the following components is NOT found in the structure of troponin?
What is the role of curare in neuromuscular transmission?
What is the role of curare in neuromuscular transmission?
What is the primary effect of anticholinesterase drugs in the treatment of myasthenia gravis?
What is the primary effect of anticholinesterase drugs in the treatment of myasthenia gravis?
What characterizes the progression of myasthenia gravis symptoms?
What characterizes the progression of myasthenia gravis symptoms?
During the pathophysiology of myasthenia gravis, what role do autoantibodies play?
During the pathophysiology of myasthenia gravis, what role do autoantibodies play?
What is a common autoimmune condition associated with myasthenia gravis?
What is a common autoimmune condition associated with myasthenia gravis?
What chest imaging is recommended for newly diagnosed myasthenia gravis patients?
What chest imaging is recommended for newly diagnosed myasthenia gravis patients?
What percentage of myasthenia gravis patients is likely to have thymic abnormalities?
What percentage of myasthenia gravis patients is likely to have thymic abnormalities?
What is the typical age distribution for women diagnosed with myasthenia gravis?
What is the typical age distribution for women diagnosed with myasthenia gravis?
What is the role of acetylcholinesterase in the synaptic cleft?
What is the role of acetylcholinesterase in the synaptic cleft?
During neuromuscular transmission, what triggers the release of ACh from synaptic vesicles?
During neuromuscular transmission, what triggers the release of ACh from synaptic vesicles?
What results from an increase in Na+ conductance during neuromuscular transmission?
What results from an increase in Na+ conductance during neuromuscular transmission?
Why does neuromuscular transmission exhibit unidirectionality?
Why does neuromuscular transmission exhibit unidirectionality?
What occurs during the depolarization of the muscle cell membrane?
What occurs during the depolarization of the muscle cell membrane?
What physiological property makes neuromuscular transmission prone to fatigue?
What physiological property makes neuromuscular transmission prone to fatigue?
Which of the following describes the synaptic cleft?
Which of the following describes the synaptic cleft?
What is contained within each synaptic vesicle released during neuromuscular transmission?
What is contained within each synaptic vesicle released during neuromuscular transmission?
Flashcards are hidden until you start studying
Study Notes
Neuromuscular Transmission
- Neuromuscular transmission is the process of transmitting nerve impulses from alpha motor neurons (αMNs) to skeletal muscle fibers.
- It is a crucial process for voluntary muscle movement.
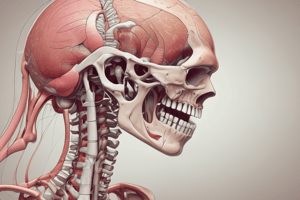
Physiology of Skeletal Muscles
- Skeletal muscles are attached to bones and are responsible for voluntary movement.
- Human bodies contain over 400 skeletal muscles.
- Skeletal muscle functions include:
- Static force production for maintaining posture and stabilizing joints.
- Kinetic force production for locomotion and breathing.
- Heat production.
- Help venous drainage.
Muscle Proteins
-
Myosin protein:
- Contains an actin-binding site, ATP binding site, and a catalytic site for ATP hydrolysis (myosin ATPase).
- The head of the myosin protein extends to the side to form an arm.
- Arms and heads together are called cross-bridges.
- Cross-bridges are flexible at two points called hinges.
-
Thin filament proteins:
- Each thin filament contains 300-400 actin molecules.
- Actin molecules have specific myosin cross-bridge binding sites (active sites), an ATP binding site, and a catalytic site for ATP hydrolysis (actomyosin ATPase).
- Tropomyosin molecules cover the active sites on actin under resting conditions, preventing contraction.
- Troponin is a complex of three globular protein molecules:
- Troponin-I binds actin to inhibit actomyosin ATPase activity.
- Troponin-T binds to tropomyosin.
- Troponin-C binds Ca2+.
Tubular System
-
Transverse (T) Tubules:
- Invaginations of the sarcolemma.
- Located at the junction of A and I bands in mammalian skeletal muscle.
- Propagate action potentials from the sarcolemma into the T tubule network.
- Contain extracellular fluid (ECF).
-
Sarcoplasmic Reticulum (SR):
- ER of the muscle fiber that surrounds each myofibril.
- Contains high levels of calcium ions (Ca2+) used to initiate muscle contraction.
- Expanded ends form terminal cisternae (TC), which make contact with T tubules on either side of the sarcomere at the A and I band junction (triad).
- Foot processes span the space between T tubule and SR membranes.
- The SR membrane contains the ryanodine receptor, which is a Ca2+ release channel.
- The T-tubule membrane contains the dihydropyridine (DHP) receptor, which opens the ryanodine Ca2+ release channel on the SR.
Neuromuscular Junction
- The neuromuscular junction (NMJ) is the site where a motor neuron communicates with a muscle fiber.
- Action potentials in the motor neuron cause the release of acetylcholine (ACh) at the NMJ, triggering muscle contraction.
- Physiologic anatomy of the NMJ:
- Alpha motor neurons (αMNs) branch to innervate multiple muscle fibers.
- Each muscle fiber receives only one axon terminal containing ACh vesicles.
- The nerve ending fits into a depression in the muscle membrane called the motor end plate (MEP).
- MEP is rich in Ach receptors and contains junctional folds.
- The synaptic cleft is the extracellular space between the nerve terminal and muscle membrane, containing basal lamina and the enzyme acetylcholinesterase (AChE).
Neuromuscular Transmission
- The sequence of events during neuromuscular transmission includes:
- Action potential reaches the nerve ending, opening voltage-gated Ca2+ channels.
- Ca2+ influx into the nerve terminal binds to calmodulin and activates CaM kinases.
- ACh vesicles fuse with the membrane and release their contents by exocytosis.
- ACh diffuses across the synaptic cleft and binds to receptors on the MEP, opening ion channels.
- Na+ influx and K+ efflux depolarize the muscle membrane, creating an end-plate potential (EPP).
- EPP triggers action potentials on either side of the MEP, which propagate along the muscle fiber and initiate contraction.
- Acetylcholinesterase (AChE) rapidly degrades ACh in the synaptic cleft to prevent continuous stimulation of the muscle fiber.
Properties of Neuromuscular Transmission
- Unidirectional: transmission occurs from neuron to muscle fiber.
- Delay: a short delay (0.5 msec) between nerve stimulation and muscle contraction.
- Fatiguability: prolonged stimulation leads to fatigue as ACh vesicles become depleted.
- Ionic influences: ion concentrations affect neuromuscular transmission.
- Drug effects: drugs can stimulate or block neuromuscular transmission.
Myasthenia Gravis (MG)
- A serious autoimmune disease characterized by muscle weakness and fatigue.
- Caused by antibodies against ACh receptors, leading to decreased receptor numbers at the NMJ.
- Symptoms worsen with repeated stimulation due to decreased ACh release.
- Can be ocular, bulbar, or generalized.
- Patients may have a family history of autoimmune disorders, and thymic abnormalities are frequently observed.
Treatment of Myasthenia Gravis
- Chest CT scan is indicated to rule out thymoma.
- Anticholinesterase drugs such as physostigmine and neostigmine can ameliorate symptoms by increasing ACh levels.
- Thymectomy is considered, especially when thymoma is suspected.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.