Podcast
Questions and Answers
What role does acetylcholinesterase play in muscle fiber excitation?
What role does acetylcholinesterase play in muscle fiber excitation?
- It enhances the action of acetylcholine.
- It stimulates the release of more acetylcholine.
- It increases the duration of acetylcholine presence.
- It breaks down acetylcholine in the synaptic space. (correct)
Why is there a limited duration for acetylcholine action in the synaptic space?
Why is there a limited duration for acetylcholine action in the synaptic space?
- It is predominantly destroyed by acetylcholinesterase. (correct)
- It requires re-synthesis before action can occur.
- It is quickly absorbed by muscle fibers.
- It binds permanently to receptors.
What effect does the rapid removal of acetylcholine have on muscle fibers?
What effect does the rapid removal of acetylcholine have on muscle fibers?
- It increases the muscle's sensitivity to stimulation.
- It prevents over-excitation and facilitates recovery. (correct)
- It prolongs muscle contraction.
- It leads to constant relaxation of the muscle.
What is a consequence of fatigue at the neuromuscular junction?
What is a consequence of fatigue at the neuromuscular junction?
What happens to acetylcholine after it diffuses out of the synaptic space?
What happens to acetylcholine after it diffuses out of the synaptic space?
What could potentially cause a weakened end plate potential?
What could potentially cause a weakened end plate potential?
How long does acetylcholine typically remain active in the synaptic space?
How long does acetylcholine typically remain active in the synaptic space?
What physiological process is similar to fatigue of the neuromuscular junction?
What physiological process is similar to fatigue of the neuromuscular junction?
What is the main role of calcium ions at the neuromuscular junction?
What is the main role of calcium ions at the neuromuscular junction?
Which structure is primarily responsible for insulating the motor end plate?
Which structure is primarily responsible for insulating the motor end plate?
What is the width of the synaptic space at the neuromuscular junction?
What is the width of the synaptic space at the neuromuscular junction?
What is the primary function of the acetylcholine receptors located in the muscle fiber membrane?
What is the primary function of the acetylcholine receptors located in the muscle fiber membrane?
What type of process is involved in the release of acetylcholine from vesicles?
What type of process is involved in the release of acetylcholine from vesicles?
What are the smaller folds at the bottom of the synaptic gutter called?
What are the smaller folds at the bottom of the synaptic gutter called?
Which of the following accurately describes the neuromuscular junction structure?
Which of the following accurately describes the neuromuscular junction structure?
What initiates the opening of voltage-gated calcium channels at the motor end plate?
What initiates the opening of voltage-gated calcium channels at the motor end plate?
What role do mitochondria play in the axon terminal?
What role do mitochondria play in the axon terminal?
What is the function of acetylcholine at the motor end plate?
What is the function of acetylcholine at the motor end plate?
Where are acetylcholine-gated ion channels primarily located?
Where are acetylcholine-gated ion channels primarily located?
What initiates the opening of the acetylcholine-gated ion channel?
What initiates the opening of the acetylcholine-gated ion channel?
What is concentrated in the synaptic vesicles at the axon terminal?
What is concentrated in the synaptic vesicles at the axon terminal?
Which structure is involved in the facilitation of synaptic transmission at the motor end plate?
Which structure is involved in the facilitation of synaptic transmission at the motor end plate?
What happens after acetylcholine is emptied into the synaptic space?
What happens after acetylcholine is emptied into the synaptic space?
What is located immediately below the dense bar areas in the muscle fiber membrane?
What is located immediately below the dense bar areas in the muscle fiber membrane?
What role do calcium ions play when an action potential arrives at the nerve terminal?
What role do calcium ions play when an action potential arrives at the nerve terminal?
Which statement accurately describes the function of acetylcholinesterase?
Which statement accurately describes the function of acetylcholinesterase?
What occurs as a result of D-tubocurarine application at the neuromuscular junction?
What occurs as a result of D-tubocurarine application at the neuromuscular junction?
What happens to acetylcholine after it is released into the synaptic space?
What happens to acetylcholine after it is released into the synaptic space?
What type of drugs can prevent impulses from reaching the muscle at the neuromuscular junction?
What type of drugs can prevent impulses from reaching the muscle at the neuromuscular junction?
What is the primary effect of diisopropyl fluorophosphate on the nervous system?
What is the primary effect of diisopropyl fluorophosphate on the nervous system?
How many acetylcholine molecules are stored in a single vesicle?
How many acetylcholine molecules are stored in a single vesicle?
What consequence can occur from excessive stimulation of the muscle by acetylcholine?
What consequence can occur from excessive stimulation of the muscle by acetylcholine?
What role does acetylcholinesterase play in the neuromuscular junction?
What role does acetylcholinesterase play in the neuromuscular junction?
What is the consequence of the antibodies in myasthenia gravis?
What is the consequence of the antibodies in myasthenia gravis?
How does myasthenia gravis primarily affect muscle function?
How does myasthenia gravis primarily affect muscle function?
What are ‘coated pits’ in the context of the neuromuscular junction?
What are ‘coated pits’ in the context of the neuromuscular junction?
What typically triggers the rapid reformation of vesicles at the nerve terminal?
What typically triggers the rapid reformation of vesicles at the nerve terminal?
In myasthenia gravis, how many vesicles are typically available for transmission at the neuromuscular junction?
In myasthenia gravis, how many vesicles are typically available for transmission at the neuromuscular junction?
What is the timeframe for the sequence of events following an action potential in the neuromuscular junction?
What is the timeframe for the sequence of events following an action potential in the neuromuscular junction?
What happens if the disease intensity of myasthenia gravis is severe enough?
What happens if the disease intensity of myasthenia gravis is severe enough?
What role do dihydropyridine receptors play in the excitation-contraction coupling process?
What role do dihydropyridine receptors play in the excitation-contraction coupling process?
How do T tubules interact with the extracellular fluid?
How do T tubules interact with the extracellular fluid?
What initiates the release of calcium ions from the sarcoplasmic reticulum?
What initiates the release of calcium ions from the sarcoplasmic reticulum?
What structural feature facilitates the branching of T tubules among myofibrils?
What structural feature facilitates the branching of T tubules among myofibrils?
What happens to the calcium release channels after they are activated?
What happens to the calcium release channels after they are activated?
What is the primary effect of calcium ions released into the sarcoplasm?
What is the primary effect of calcium ions released into the sarcoplasm?
Why is the calcium pump important after muscle contraction occurs?
Why is the calcium pump important after muscle contraction occurs?
In which location do dihydropyridine receptors initiate the physiological changes leading to muscle contraction?
In which location do dihydropyridine receptors initiate the physiological changes leading to muscle contraction?
What mechanism is primarily responsible for the rapid removal of acetylcholine from the synaptic space?
What mechanism is primarily responsible for the rapid removal of acetylcholine from the synaptic space?
Which of the following effects is associated with the fatigue of the neuromuscular junction?
Which of the following effects is associated with the fatigue of the neuromuscular junction?
What can occur when acetylcholine diffuses out of the synaptic space?
What can occur when acetylcholine diffuses out of the synaptic space?
Which statement best describes the time frame of acetylcholine action in the synaptic space?
Which statement best describes the time frame of acetylcholine action in the synaptic space?
What is one potential outcome of acetylcholine being rapidly removed from the synaptic space?
What is one potential outcome of acetylcholine being rapidly removed from the synaptic space?
What is the main function of synaptic vesicles at the neuromuscular junction?
What is the main function of synaptic vesicles at the neuromuscular junction?
Which of the following structures is primarily identified at the neuromuscular junction?
Which of the following structures is primarily identified at the neuromuscular junction?
How does the presence of acetylcholinesterase in the synaptic space primarily affect neuromuscular transmission?
How does the presence of acetylcholinesterase in the synaptic space primarily affect neuromuscular transmission?
What is the approximate number of acetylcholine vesicles released when a nerve impulse reaches the neuromuscular junction?
What is the approximate number of acetylcholine vesicles released when a nerve impulse reaches the neuromuscular junction?
Which of the following best describes the synaptic space at the neuromuscular junction?
Which of the following best describes the synaptic space at the neuromuscular junction?
What is the role of myelinated nerve fibers in the excitation of skeletal muscle?
What is the role of myelinated nerve fibers in the excitation of skeletal muscle?
What type of motor control do large motoneurons in the anterior horns of the spinal cord provide?
What type of motor control do large motoneurons in the anterior horns of the spinal cord provide?
What causes a conformational change that opens acetylcholine-gated ion channels?
What causes a conformational change that opens acetylcholine-gated ion channels?
Where are mitochondria primarily located in relation to the synaptic space?
Where are mitochondria primarily located in relation to the synaptic space?
What is the role of the dense bar in the structure of the neuromuscular junction?
What is the role of the dense bar in the structure of the neuromuscular junction?
What is primarily concentrated in the synaptic vesicles at the axon terminal?
What is primarily concentrated in the synaptic vesicles at the axon terminal?
What specific structural characteristic helps in the facilitation of synaptic transmission?
What specific structural characteristic helps in the facilitation of synaptic transmission?
What triggers the release of acetylcholine from the vesicles at the neuromuscular junction?
What triggers the release of acetylcholine from the vesicles at the neuromuscular junction?
Which type of channel remains constricted until acetylcholine binds to it?
Which type of channel remains constricted until acetylcholine binds to it?
Which component supports the release sites for neurotransmitters at the neuromuscular junction?
Which component supports the release sites for neurotransmitters at the neuromuscular junction?
What immediate effect does acetylcholine have upon binding to its receptors?
What immediate effect does acetylcholine have upon binding to its receptors?
What is the primary result of botulinum toxin's effect at the neuromuscular junction?
What is the primary result of botulinum toxin's effect at the neuromuscular junction?
What physiological effect occurs when stimulation of the nerve fiber exceeds 100 impulses per second for several minutes?
What physiological effect occurs when stimulation of the nerve fiber exceeds 100 impulses per second for several minutes?
What prevents chloride ions from passing through the acetylcholine-gated channel at the neuromuscular junction?
What prevents chloride ions from passing through the acetylcholine-gated channel at the neuromuscular junction?
What happens to acetylcholine once it activates the acetylcholine receptors?
What happens to acetylcholine once it activates the acetylcholine receptors?
What characterizes the safety factor at the neuromuscular junction under normal conditions?
What characterizes the safety factor at the neuromuscular junction under normal conditions?
What is a consequence of the destruction of acetylcholine by acetylcholinesterase in the synaptic space?
What is a consequence of the destruction of acetylcholine by acetylcholinesterase in the synaptic space?
What typically limits the effective stimulation of the neuromuscular junction during extended activity?
What typically limits the effective stimulation of the neuromuscular junction during extended activity?
What typically occurs to the motor end plate during fatigue of the neuromuscular junction?
What typically occurs to the motor end plate during fatigue of the neuromuscular junction?
Why is the safety factor at the neuromuscular junction considered high?
Why is the safety factor at the neuromuscular junction considered high?
How does acetylcholine behave in the synaptic space once it has been released?
How does acetylcholine behave in the synaptic space once it has been released?
What is the primary consequence of the sudden influx of sodium ions into the muscle fiber during neuromuscular transmission?
What is the primary consequence of the sudden influx of sodium ions into the muscle fiber during neuromuscular transmission?
What is the effect of opening acetylcholine-gated channels in the muscle fiber membrane?
What is the effect of opening acetylcholine-gated channels in the muscle fiber membrane?
How does the molecular structure of the acetylcholine receptor contribute to its function?
How does the molecular structure of the acetylcholine receptor contribute to its function?
What is the total molecular weight of the acetylcholine receptor complex?
What is the total molecular weight of the acetylcholine receptor complex?
What initiates the action potential in a muscle fiber following the creation of an end plate potential?
What initiates the action potential in a muscle fiber following the creation of an end plate potential?
Which protein subunits comprise the acetylcholine receptor complex?
Which protein subunits comprise the acetylcholine receptor complex?
What potential change occurs in the muscle fiber when sodium ions enter during neuromuscular transmission?
What potential change occurs in the muscle fiber when sodium ions enter during neuromuscular transmission?
What event follows the creation of the end plate potential in the muscle fiber membrane?
What event follows the creation of the end plate potential in the muscle fiber membrane?
What is not a characteristic of the acetylcholine receptor in muscle fibers?
What is not a characteristic of the acetylcholine receptor in muscle fibers?
What is a significant outcome of the action potential that spreads along the muscle membrane?
What is a significant outcome of the action potential that spreads along the muscle membrane?
What primarily prevents negatively charged ions from passing through the acetylcholine-gated channel?
What primarily prevents negatively charged ions from passing through the acetylcholine-gated channel?
Why do sodium ions predominantly flow through acetylcholine-gated channels in muscle tissues?
Why do sodium ions predominantly flow through acetylcholine-gated channels in muscle tissues?
What characteristic of the acetylcholine-gated channel contributes to ion selectivity?
What characteristic of the acetylcholine-gated channel contributes to ion selectivity?
What is the typical resting membrane potential of a muscle fiber?
What is the typical resting membrane potential of a muscle fiber?
What factors lead to a greater influx of sodium ions relative to potassium ions in muscle fibers?
What factors lead to a greater influx of sodium ions relative to potassium ions in muscle fibers?
Which ions are primarily involved in the acetylcholine-gated channel's activity?
Which ions are primarily involved in the acetylcholine-gated channel's activity?
Why does the acetylcholine-gated channel not allow chloride ions to pass through?
Why does the acetylcholine-gated channel not allow chloride ions to pass through?
What occurs when calcium ion concentration inside the nerve terminal increases?
What occurs when calcium ion concentration inside the nerve terminal increases?
What is the primary action of diisopropyl fluorophosphate on acetylcholinesterase?
What is the primary action of diisopropyl fluorophosphate on acetylcholinesterase?
What is a potential consequence of excessive acetylcholine accumulation at the neuromuscular junction?
What is a potential consequence of excessive acetylcholine accumulation at the neuromuscular junction?
What is the mechanism of action for curariform drugs at the neuromuscular junction?
What is the mechanism of action for curariform drugs at the neuromuscular junction?
What primary function do the small vesicles at the nerve terminal serve?
What primary function do the small vesicles at the nerve terminal serve?
What is the primary impact of opening acetylcholine-gated channels in muscle fibers?
What is the primary impact of opening acetylcholine-gated channels in muscle fibers?
Which proteins are primarily involved in the structure of the receptor complex for acetylcholine?
Which proteins are primarily involved in the structure of the receptor complex for acetylcholine?
What electrical change occurs inside the muscle fiber when sodium ions rush in due to opened acetylcholine-gated channels?
What electrical change occurs inside the muscle fiber when sodium ions rush in due to opened acetylcholine-gated channels?
What is created as a result of the end plate potential within the muscle fiber?
What is created as a result of the end plate potential within the muscle fiber?
What is the primary difference between acetylcholine and drugs like methacholine or nicotine?
What is the primary difference between acetylcholine and drugs like methacholine or nicotine?
What structural configuration do the proteins in the acetylcholine receptor create?
What structural configuration do the proteins in the acetylcholine receptor create?
What triggers a new action potential in muscle fibers after contraction?
What triggers a new action potential in muscle fibers after contraction?
How does the end plate potential contribute to muscle contraction?
How does the end plate potential contribute to muscle contraction?
What substances inactivate acetylcholinesterase, enhancing neuromuscular transmission?
What substances inactivate acetylcholinesterase, enhancing neuromuscular transmission?
Which structure is primarily responsible for the formation of small vesicles in motoneurons?
Which structure is primarily responsible for the formation of small vesicles in motoneurons?
What type of potential is specifically referred to as the result of sodium influx through acetylcholine-gated channels?
What type of potential is specifically referred to as the result of sodium influx through acetylcholine-gated channels?
What is the primary consequence of the positive potential change created by sodium ions in the muscle fiber?
What is the primary consequence of the positive potential change created by sodium ions in the muscle fiber?
What is the impact of drugs that stimulate the muscle fiber by mimicking acetylcholine?
What is the impact of drugs that stimulate the muscle fiber by mimicking acetylcholine?
Under what conditions is measurable fatigue at the neuromuscular junction likely to occur?
Under what conditions is measurable fatigue at the neuromuscular junction likely to occur?
What initiates depolarization of the muscle fiber membrane at the motor end plate?
What initiates depolarization of the muscle fiber membrane at the motor end plate?
Which of the following is NOT a characteristic of drugs that stimulate the neuromuscular junction?
Which of the following is NOT a characteristic of drugs that stimulate the neuromuscular junction?
What role does the neuromuscular junction play in chemical transmission of signals?
What role does the neuromuscular junction play in chemical transmission of signals?
Which process primarily contributes to the rapid elimination of acetylcholine from the synaptic space?
Which process primarily contributes to the rapid elimination of acetylcholine from the synaptic space?
What is the primary location of acetylcholinesterase in relation to the synaptic structure?
What is the primary location of acetylcholinesterase in relation to the synaptic structure?
What effect does acetylcholine diffusion out of the synaptic space have on muscle fibers?
What effect does acetylcholine diffusion out of the synaptic space have on muscle fibers?
Which factor is likely responsible for the cessation of muscle contraction following an action potential?
Which factor is likely responsible for the cessation of muscle contraction following an action potential?
What does the phenomenon of fatigue at the neuromuscular junction primarily indicate?
What does the phenomenon of fatigue at the neuromuscular junction primarily indicate?
How does the action of acetylcholinesterase affect muscle fiber recovery time?
How does the action of acetylcholinesterase affect muscle fiber recovery time?
What is the underlying reason for a weakened end plate potential due to botulinum toxin?
What is the underlying reason for a weakened end plate potential due to botulinum toxin?
What role does the brief presence of acetylcholine in the synaptic space play during muscle excitation?
What role does the brief presence of acetylcholine in the synaptic space play during muscle excitation?
In terms of neurotransmitter action, what is a similarity between the neuromuscular junction and synapses in the central nervous system?
In terms of neurotransmitter action, what is a similarity between the neuromuscular junction and synapses in the central nervous system?
What is the typical timeframe within which acetylcholine acts before being cleared from the synaptic space?
What is the typical timeframe within which acetylcholine acts before being cleared from the synaptic space?
Flashcards
Acetylcholine
Acetylcholine
An excitatory neurotransmitter released at the neuromuscular junction.
Motor end plate
Motor end plate
Specialized region of a muscle fiber membrane where nerve impulses are transmitted.
Synaptic vesicles
Synaptic vesicles
Membrane-bound sacs in axon terminals containing neurotransmitters.
Subneural clefts
Subneural clefts
Signup and view all the flashcards
Acetylcholine-gated ion channels
Acetylcholine-gated ion channels
Signup and view all the flashcards
Mitochondria
Mitochondria
Signup and view all the flashcards
ATP
ATP
Signup and view all the flashcards
Synaptic space
Synaptic space
Signup and view all the flashcards
Neuromuscular Junction
Neuromuscular Junction
Signup and view all the flashcards
Acetylcholine breakdown
Acetylcholine breakdown
Signup and view all the flashcards
Acetylcholinesterase location
Acetylcholinesterase location
Signup and view all the flashcards
Synaptic Space/Cleft
Synaptic Space/Cleft
Signup and view all the flashcards
Acetylcholine diffusion
Acetylcholine diffusion
Signup and view all the flashcards
Synaptic space duration
Synaptic space duration
Signup and view all the flashcards
Synaptic Gutter/Trough
Synaptic Gutter/Trough
Signup and view all the flashcards
Neuromuscular junction fatigue
Neuromuscular junction fatigue
Signup and view all the flashcards
Voltage-gated Calcium Channels
Voltage-gated Calcium Channels
Signup and view all the flashcards
Muscle fiber excitation
Muscle fiber excitation
Signup and view all the flashcards
Exocytosis
Exocytosis
Signup and view all the flashcards
Prevent continued stimulation
Prevent continued stimulation
Signup and view all the flashcards
Central nervous system fatigue
Central nervous system fatigue
Signup and view all the flashcards
What causes muscle spasms?
What causes muscle spasms?
Signup and view all the flashcards
How is acetylcholine stored in the nerve terminal?
How is acetylcholine stored in the nerve terminal?
Signup and view all the flashcards
Why is calcium important at the neuromuscular junction?
Why is calcium important at the neuromuscular junction?
Signup and view all the flashcards
How does neostigmine affect acetylcholine?
How does neostigmine affect acetylcholine?
Signup and view all the flashcards
How does D-tubocurarine block nerve transmission?
How does D-tubocurarine block nerve transmission?
Signup and view all the flashcards
What is axoplasm?
What is axoplasm?
Signup and view all the flashcards
What is acetylcholinesterase?
What is acetylcholinesterase?
Signup and view all the flashcards
How does diisopropyl fluorophosphate affect the neuromuscular junction?
How does diisopropyl fluorophosphate affect the neuromuscular junction?
Signup and view all the flashcards
T Tubules
T Tubules
Signup and view all the flashcards
Sarcoplasmic Reticulum
Sarcoplasmic Reticulum
Signup and view all the flashcards
Dihydropyridine Receptors
Dihydropyridine Receptors
Signup and view all the flashcards
Ryanodine Receptor Channels
Ryanodine Receptor Channels
Signup and view all the flashcards
Excitation-Contraction Coupling
Excitation-Contraction Coupling
Signup and view all the flashcards
How do T tubules link to the sarcoplasmic reticulum?
How do T tubules link to the sarcoplasmic reticulum?
Signup and view all the flashcards
Why is calcium released from the SR?
Why is calcium released from the SR?
Signup and view all the flashcards
How is calcium removed after contraction?
How is calcium removed after contraction?
Signup and view all the flashcards
How many vesicles typically rupture during an action potential?
How many vesicles typically rupture during an action potential?
Signup and view all the flashcards
What enzyme breaks down acetylcholine?
What enzyme breaks down acetylcholine?
Signup and view all the flashcards
What happens to choline after acetylcholine breakdown?
What happens to choline after acetylcholine breakdown?
Signup and view all the flashcards
Why is myasthenia gravis a debilitating disease?
Why is myasthenia gravis a debilitating disease?
Signup and view all the flashcards
What is the role of clathrin in vesicle formation?
What is the role of clathrin in vesicle formation?
Signup and view all the flashcards
How long does it take for new vesicles to form after an action potential?
How long does it take for new vesicles to form after an action potential?
Signup and view all the flashcards
What is the limit of vesicles available in the nerve ending?
What is the limit of vesicles available in the nerve ending?
Signup and view all the flashcards
Why are end plate potentials weak in myasthenia gravis?
Why are end plate potentials weak in myasthenia gravis?
Signup and view all the flashcards
Acetylcholinesterase
Acetylcholinesterase
Signup and view all the flashcards
What happens after acetylcholine is released?
What happens after acetylcholine is released?
Signup and view all the flashcards
What is the role of mitochondria in the nerve terminal?
What is the role of mitochondria in the nerve terminal?
Signup and view all the flashcards
Why are acetylcholine-gated ion channels located near subneural clefts?
Why are acetylcholine-gated ion channels located near subneural clefts?
Signup and view all the flashcards
What happens when two acetylcholine molecules bind to the ion channel?
What happens when two acetylcholine molecules bind to the ion channel?
Signup and view all the flashcards
What is the role of calcium in acetylcholine release?
What is the role of calcium in acetylcholine release?
Signup and view all the flashcards
How is acetylcholine removed from the synaptic space?
How is acetylcholine removed from the synaptic space?
Signup and view all the flashcards
What is the effect of neostigmine on acetylcholine?
What is the effect of neostigmine on acetylcholine?
Signup and view all the flashcards
What is the significance of the dense bar area in the neuromuscular junction?
What is the significance of the dense bar area in the neuromuscular junction?
Signup and view all the flashcards
How does the acetylcholine-gated ion channel open?
How does the acetylcholine-gated ion channel open?
Signup and view all the flashcards
How does acetylcholinesterase work?
How does acetylcholinesterase work?
Signup and view all the flashcards
Why is rapid acetylcholine removal important?
Why is rapid acetylcholine removal important?
Signup and view all the flashcards
What happens if acetylcholinesterase is blocked?
What happens if acetylcholinesterase is blocked?
Signup and view all the flashcards
What is fatigue of the neuromuscular junction?
What is fatigue of the neuromuscular junction?
Signup and view all the flashcards
What triggers the release of acetylcholine?
What triggers the release of acetylcholine?
Signup and view all the flashcards
What happens to acetylcholine in the synaptic cleft?
What happens to acetylcholine in the synaptic cleft?
Signup and view all the flashcards
What happens to sodium ions when acetylcholine binds to receptors?
What happens to sodium ions when acetylcholine binds to receptors?
Signup and view all the flashcards
What is the end plate potential and what does it do?
What is the end plate potential and what does it do?
Signup and view all the flashcards
What are the steps in neuromuscular transmission?
What are the steps in neuromuscular transmission?
Signup and view all the flashcards
Why is acetylcholine broken down?
Why is acetylcholine broken down?
Signup and view all the flashcards
What is the role of calcium in muscle contraction?
What is the role of calcium in muscle contraction?
Signup and view all the flashcards
What are the main steps in excitation-contraction coupling?
What are the main steps in excitation-contraction coupling?
Signup and view all the flashcards
How is muscle contraction terminated?
How is muscle contraction terminated?
Signup and view all the flashcards
Safety Factor
Safety Factor
Signup and view all the flashcards
Botulinum Toxin
Botulinum Toxin
Signup and view all the flashcards
What is the role of calcium in neurotransmitter release?
What is the role of calcium in neurotransmitter release?
Signup and view all the flashcards
Why is acetylcholine rapidly broken down?
Why is acetylcholine rapidly broken down?
Signup and view all the flashcards
How does botulinum toxin affect the neuromuscular junction?
How does botulinum toxin affect the neuromuscular junction?
Signup and view all the flashcards
What is the significance of the safety factor?
What is the significance of the safety factor?
Signup and view all the flashcards
What are the consequences of prolonged muscle stimulation?
What are the consequences of prolonged muscle stimulation?
Signup and view all the flashcards
How does acetylcholinesterase help regulate muscle contraction?
How does acetylcholinesterase help regulate muscle contraction?
Signup and view all the flashcards
Acetylcholine-gated Channel Size
Acetylcholine-gated Channel Size
Signup and view all the flashcards
Sodium Ion Flow
Sodium Ion Flow
Signup and view all the flashcards
Preventing Muscle Fatigue
Preventing Muscle Fatigue
Signup and view all the flashcards
Neostigmine's Effect
Neostigmine's Effect
Signup and view all the flashcards
D-Tubocurarine's Block
D-Tubocurarine's Block
Signup and view all the flashcards
End Plate Potential
End Plate Potential
Signup and view all the flashcards
How does the end plate potential initiate muscle contraction?
How does the end plate potential initiate muscle contraction?
Signup and view all the flashcards
What is the role of sodium ions in the end plate potential?
What is the role of sodium ions in the end plate potential?
Signup and view all the flashcards
What is the effect of opening acetylcholine-gated channels?
What is the effect of opening acetylcholine-gated channels?
Signup and view all the flashcards
How does acetylcholine affect the acetylcholine-gated channels?
How does acetylcholine affect the acetylcholine-gated channels?
Signup and view all the flashcards
What is the significance of the end plate potential?
What is the significance of the end plate potential?
Signup and view all the flashcards
How does a high safety factor benefit muscle function?
How does a high safety factor benefit muscle function?
Signup and view all the flashcards
What is the role of acetylcholinesterase in muscle contraction?
What is the role of acetylcholinesterase in muscle contraction?
Signup and view all the flashcards
What is the consequence of prolonged muscle stimulation?
What is the consequence of prolonged muscle stimulation?
Signup and view all the flashcards
What stores acetylcholine?
What stores acetylcholine?
Signup and view all the flashcards
Why is calcium important at the junction?
Why is calcium important at the junction?
Signup and view all the flashcards
How does D-tubocurarine block transmission?
How does D-tubocurarine block transmission?
Signup and view all the flashcards
What does diisopropyl fluorophosphate do?
What does diisopropyl fluorophosphate do?
Signup and view all the flashcards
What are the stages of acetylcholine formation and release?
What are the stages of acetylcholine formation and release?
Signup and view all the flashcards
How does acetylcholine affect the muscle fiber?
How does acetylcholine affect the muscle fiber?
Signup and view all the flashcards
What are the drugs that stimulate the neuromuscular junction like acetylcholine?
What are the drugs that stimulate the neuromuscular junction like acetylcholine?
Signup and view all the flashcards
How do drugs like neostigmine affect the neuromuscular junction?
How do drugs like neostigmine affect the neuromuscular junction?
Signup and view all the flashcards
What is the safety factor at the neuromuscular junction?
What is the safety factor at the neuromuscular junction?
Signup and view all the flashcards
What is the effect of botulinum toxin?
What is the effect of botulinum toxin?
Signup and view all the flashcards
Why is rapid removal of acetylcholine important?
Why is rapid removal of acetylcholine important?
Signup and view all the flashcards
What is Myasthenia Gravis?
What is Myasthenia Gravis?
Signup and view all the flashcards
How does the neuromuscular junction adapt to repeated stimulation?
How does the neuromuscular junction adapt to repeated stimulation?
Signup and view all the flashcards
Acetylcholinesterase's Role
Acetylcholinesterase's Role
Signup and view all the flashcards
Why is acetylcholine removed?
Why is acetylcholine removed?
Signup and view all the flashcards
What happens to sodium ions?
What happens to sodium ions?
Signup and view all the flashcards
What is the end plate potential?
What is the end plate potential?
Signup and view all the flashcards
Botulinum Toxin Effect
Botulinum Toxin Effect
Signup and view all the flashcards
Safety Factor's Role
Safety Factor's Role
Signup and view all the flashcards
Calcium's Role in Neurotransmitter Release
Calcium's Role in Neurotransmitter Release
Signup and view all the flashcards
Neuromuscular Transmission Steps
Neuromuscular Transmission Steps
Signup and view all the flashcards
Study Notes
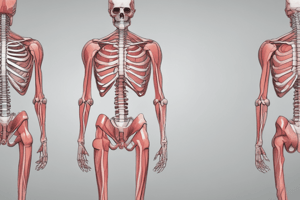
Excitation of Skeletal Muscle: Neuromuscular Transmission and Excitation-Contraction Coupling
- Skeletal muscle fibers are innervated by large myelinated nerve fibers originating from motoneurons in the spinal cord.
- Each nerve fiber branches, typically stimulating 3-hundreds of muscle fibers
- Each nerve ending forms a neuromuscular junction with the muscle fiber near its midpoint.
- Two percent of muscle fibers have more than one junction.
- The neuromuscular junction is also called the motor end plate.
Physiology of the Neuromuscular Junction
- Nerve terminals invaginate into the muscle fiber surface, but remain outside the plasma membrane.
- The motor end plate is insulated by Schwann cells.
- The invaginated muscle membrane is called the synaptic gutter or synaptic trough.
- The space between the terminal and fiber membrane is the synaptic space/cleft (20-30 nanometers).
- Subneural clefts in the gutter increase surface area for transmitter action.
- Mitochondria in the axon terminal supply ATP for acetylcholine synthesis.
- Acetylcholine is rapidly absorbed into synaptic vesicles.
- Acetylcholinesterase in the synaptic space destroys acetylcholine.
Secretion of Acetylcholine
- Nerve impulses trigger the release of about 125 acetylcholine vesicles into the synaptic space.
- Voltage-gated calcium channels open upon action potential arrival.
- Calcium ions diffuse from the space, attracting acetylcholine vesicles to the neural membrane.
- Vesicles fuse with the membrane and release acetylcholine via exocytosis.
- Calcium ion entry is the key stimulus for acetylcholine release.
Effect of Acetylcholine on Postsynaptic Membrane
- Acetylcholine receptors are gated ion channels.
- These receptors are primarily near the mouths of the subneural clefts.
- Acetylcholine binding opens the channels, allowing sodium, potassium, and calcium ions to flow.
- Sodium ions flow inwards due to the negative interior potential.
- This creates a local positive potential change—end-plate potential (EPP).
- EPPs initiate action potentials that spread along the muscle membrane, causing contraction.
Destruction of Acetylcholine
- Acetylcholinesterase rapidly breaks down acetylcholine in the synaptic cleft.
- This prevents continued muscle re-excitation after the initial action potential.
End-Plate Potential and Muscle Fiber Excitation
- Sodium influx creates electrical potential changes near the end plate—end-plate potential (EPP).
- Sufficient EPPs trigger action potential initiation in the muscle cell membrane.
- Curare blocks acetylcholine's effect (weakened EPP).
- Botulinum toxin reduces acetylcholine release. (weakened EPP).
Safety Factor and Fatigue
- The neuromuscular junction has a high safety factor (EPP is stronger than required for muscle excitation).
- Prolonged high-frequency stimulation causes the junctional fatigue (reduced acetylcholine release).
Myasthenia Gravis
- Autoimmune disease where antibodies attack acetylcholine receptors.
- Results in reduced transmission between the nerve and muscle, causing muscle weakness.
Muscle Action Potential
- Skeletal muscle action potential duration: 1-5 milliseconds
- Skeletal muscle resting membrane potential: -80 to -90 mV.
- Conduction velocity: ~3-5 m/s (Significantly slower than nerve fibers).
Spread of Action Potential
- Action potentials along the surface membrane don't penetrate deep into the fiber.
- Transverse tubules (T tubules) conduct the action potential deep into the fiber, where they initiate calcium release from the sarcoplasmic reticulum (SR).
Transverse Tubule-Sarcoplasmic Reticulum System
- T tubules are extensions of the sarcolemma (muscle cell membrane).
- They conduct action potentials deeply into the muscle fiber.
- The SR is a specialized smooth endoplasmic reticulum surrounding myofibrils.
- SR contains terminal cisternae adjacent to T tubules and longitudinal tubules.
- Action potentials in T-tubules cause calcium release (from the SR terminal cisternae) into the cytosol.
Calcium Ions and Muscle Contraction
- Calcium ions initiate muscle contraction.
- Calcium pumps in the SR remove calcium ions from the cytosol.
- This enables muscle relaxation to occur.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.