Podcast
Questions and Answers
The optimal dosage of amphotericin B can be increased to 2.0 mg/kg/day if toxicity occurs.
The optimal dosage of amphotericin B can be increased to 2.0 mg/kg/day if toxicity occurs.
False (B)
Echinocandins are effective against fluconazole-resistant Candida strains.
Echinocandins are effective against fluconazole-resistant Candida strains.
True (A)
Toxicities associated with amphotericin B in neonates include renal failure and hypokalemia.
Toxicities associated with amphotericin B in neonates include renal failure and hypokalemia.
True (A)
Caspofungin is approved by the FDA for the treatment of invasive candidiasis only.
Caspofungin is approved by the FDA for the treatment of invasive candidiasis only.
Echinocandins can damage human cell walls due to their interference with β-D-glucan synthesis.
Echinocandins can damage human cell walls due to their interference with β-D-glucan synthesis.
5-FC is taken up by susceptible fungal cells by the enzyme adenine permease.
5-FC is taken up by susceptible fungal cells by the enzyme adenine permease.
5-FU is deaminated from 5-FC by the enzyme uridine deaminase.
5-FU is deaminated from 5-FC by the enzyme uridine deaminase.
The first mechanism of 5-FU's antifungal activity involves incorporation of FUTP into fungal RNA.
The first mechanism of 5-FU's antifungal activity involves incorporation of FUTP into fungal RNA.
5-fluorodeoxyuridine monophosphate (FdUMP) inhibits an enzyme vital for DNA synthesis.
5-fluorodeoxyuridine monophosphate (FdUMP) inhibits an enzyme vital for DNA synthesis.
Terbinafine, also known as Lamisil, is effective against viral infections.
Terbinafine, also known as Lamisil, is effective against viral infections.
The mechanisms of action of 5-FU include disturbing the amino acid pool and inhibiting protein synthesis.
The mechanisms of action of 5-FU include disturbing the amino acid pool and inhibiting protein synthesis.
Creams and ointments containing Terbinafine are ineffective against fungal nail infections.
Creams and ointments containing Terbinafine are ineffective against fungal nail infections.
5-FU's conversion ultimately leads to an inhibition of RNA synthesis in fungal cells.
5-FU's conversion ultimately leads to an inhibition of RNA synthesis in fungal cells.
Caspofungin is the first inhibitor of fungal β-1,3-D-glucan synthesis approved by the FDA.
Caspofungin is the first inhibitor of fungal β-1,3-D-glucan synthesis approved by the FDA.
Flucytosine can be effectively administered as a standalone treatment for fungal infections.
Flucytosine can be effectively administered as a standalone treatment for fungal infections.
The dosage of Caspofungin does not need to be adjusted based on liver function.
The dosage of Caspofungin does not need to be adjusted based on liver function.
5-Fluorocytosine is well absorbed from the gastrointestinal tract at 75 to 90%.
5-Fluorocytosine is well absorbed from the gastrointestinal tract at 75 to 90%.
Caspofungin is effective in patients older than 3 months.
Caspofungin is effective in patients older than 3 months.
Flucytosine should be used with caution in pregnant women due to potential risks to the fetus.
Flucytosine should be used with caution in pregnant women due to potential risks to the fetus.
The half-life of Flucytosine is cited as being between 6 to 12 hours.
The half-life of Flucytosine is cited as being between 6 to 12 hours.
In cases of overdose, hemodialysis can help remove Flucytosine from the body.
In cases of overdose, hemodialysis can help remove Flucytosine from the body.
Ivermectin is effective against onchocerciasis and must be taken orally or applied to the skin.
Ivermectin is effective against onchocerciasis and must be taken orally or applied to the skin.
Metronidazole primarily acts on human cells by disrupting their DNA synthesis.
Metronidazole primarily acts on human cells by disrupting their DNA synthesis.
Side effects of Ivermectin include headaches and seizures.
Side effects of Ivermectin include headaches and seizures.
Metronidazole is 80% bioavailable when taken orally.
Metronidazole is 80% bioavailable when taken orally.
Leucopenia and neutropenia are potential side effects of long-term treatment with Ivermectin.
Leucopenia and neutropenia are potential side effects of long-term treatment with Ivermectin.
P45014DM is a type of cytochrome P540 enzyme responsible for converting lanosterol to ergosterol.
P45014DM is a type of cytochrome P540 enzyme responsible for converting lanosterol to ergosterol.
Azoles enhance the production of ergosterol, thus decreasing membrane permeability.
Azoles enhance the production of ergosterol, thus decreasing membrane permeability.
Fluconazole is available only in IV form and is poorly absorbed when taken orally.
Fluconazole is available only in IV form and is poorly absorbed when taken orally.
Voriconazole is indicated for invasive aspergillosis, blastomycosis, and serious Fusarium spp. infections.
Voriconazole is indicated for invasive aspergillosis, blastomycosis, and serious Fusarium spp. infections.
Posaconazole is used for the prevention of invasive fungal infections in transplant recipients.
Posaconazole is used for the prevention of invasive fungal infections in transplant recipients.
The serum half-life of fluconazole is approximately 48 hours, allowing for twice-daily dosing.
The serum half-life of fluconazole is approximately 48 hours, allowing for twice-daily dosing.
Topical antifungal drugs are typically used for infections treated directly on the skin, nails, or internally.
Topical antifungal drugs are typically used for infections treated directly on the skin, nails, or internally.
The absorption of fluconazole is significantly affected by the percentage of food consumed.
The absorption of fluconazole is significantly affected by the percentage of food consumed.
Artemether is solely used for the treatment of uncomplicated cases of malaria.
Artemether is solely used for the treatment of uncomplicated cases of malaria.
Suramin is administered only orally for treating African sleeping sickness.
Suramin is administered only orally for treating African sleeping sickness.
The half-life of suramin is estimated to be between 41 to 78 days.
The half-life of suramin is estimated to be between 41 to 78 days.
Artesunate is used for treating complicated cases of P.falciparum.
Artesunate is used for treating complicated cases of P.falciparum.
Metronidazole is used to treat infections such as giardiasis and trichomoniasis.
Metronidazole is used to treat infections such as giardiasis and trichomoniasis.
The exact mechanism of action of suramin is well understood and documented.
The exact mechanism of action of suramin is well understood and documented.
Artemisinin can be neurotoxic at high doses, according to clinical studies.
Artemisinin can be neurotoxic at high doses, according to clinical studies.
Parasites can uptake suramin via receptor-mediated endocytosis when it is bound to low-density lipoproteins.
Parasites can uptake suramin via receptor-mediated endocytosis when it is bound to low-density lipoproteins.
Flashcards
What are echinocandins?
What are echinocandins?
A group of antifungal medications that work by blocking the synthesis of beta-glucan, a crucial component of fungal cell walls.
What is beta-glucan?
What is beta-glucan?
A carbohydrate polymer found in fungal cell walls that helps maintain their structural integrity.
How do echinocandins work?
How do echinocandins work?
Echinocandins disrupt the catalytic subunits of beta-D-glucan synthase, an enzyme responsible for the synthesis of beta-glucan.
What are echinocandins used for?
What are echinocandins used for?
Signup and view all the flashcards
Why are echinocandins unique?
Why are echinocandins unique?
Signup and view all the flashcards
Echinocandins
Echinocandins
Signup and view all the flashcards
Beta-glucan
Beta-glucan
Signup and view all the flashcards
Glucan Synthase
Glucan Synthase
Signup and view all the flashcards
Efflux Pumps
Efflux Pumps
Signup and view all the flashcards
Caspofungin
Caspofungin
Signup and view all the flashcards
Flucytosine (5-FC)
Flucytosine (5-FC)
Signup and view all the flashcards
5-Fluorouracil (5-FU)
5-Fluorouracil (5-FU)
Signup and view all the flashcards
Elevated AST and ALT levels
Elevated AST and ALT levels
Signup and view all the flashcards
What is the role of the 5-fluorocytosine?
What is the role of the 5-fluorocytosine?
Signup and view all the flashcards
How is 5-FC activated inside the fungal cell?
How is 5-FC activated inside the fungal cell?
Signup and view all the flashcards
How does 5-FU affect the first mechanism of antifungal activity of 5-FC?
How does 5-FU affect the first mechanism of antifungal activity of 5-FC?
Signup and view all the flashcards
How does 5-FU affect the second mechanism of antifungal activity of 5-FC?
How does 5-FU affect the second mechanism of antifungal activity of 5-FC?
Signup and view all the flashcards
What is terbinafine used for?
What is terbinafine used for?
Signup and view all the flashcards
How does terbinafine work?
How does terbinafine work?
Signup and view all the flashcards
What are some different applications of terbinafine?
What are some different applications of terbinafine?
Signup and view all the flashcards
What types of fungal infections are commonly treated with terbinafine?
What types of fungal infections are commonly treated with terbinafine?
Signup and view all the flashcards
What are topical antifungal drugs used for?
What are topical antifungal drugs used for?
Signup and view all the flashcards
What is Lanosterol-14-alpha-demethylase (P45014DM)?
What is Lanosterol-14-alpha-demethylase (P45014DM)?
Signup and view all the flashcards
How do Azole antifungal drugs work ?
How do Azole antifungal drugs work ?
Signup and view all the flashcards
What is the mechanism of action of Azoles?
What is the mechanism of action of Azoles?
Signup and view all the flashcards
What are azoles?
What are azoles?
Signup and view all the flashcards
Give some examples of Azole drugs.
Give some examples of Azole drugs.
Signup and view all the flashcards
What is Fluconazole used for?
What is Fluconazole used for?
Signup and view all the flashcards
What is Voriconazole used for?
What is Voriconazole used for?
Signup and view all the flashcards
Suramin
Suramin
Signup and view all the flashcards
Artemether
Artemether
Signup and view all the flashcards
Artesunate
Artesunate
Signup and view all the flashcards
Metronidazole
Metronidazole
Signup and view all the flashcards
Selective Toxicity
Selective Toxicity
Signup and view all the flashcards
Heme
Heme
Signup and view all the flashcards
Pharmacokinetics
Pharmacokinetics
Signup and view all the flashcards
Mechanism of Action of Suramin
Mechanism of Action of Suramin
Signup and view all the flashcards
How does Metronidazole work?
How does Metronidazole work?
Signup and view all the flashcards
Why is metronidazole selective?
Why is metronidazole selective?
Signup and view all the flashcards
What is the pharmacokinetic profile of oral metronidazole?
What is the pharmacokinetic profile of oral metronidazole?
Signup and view all the flashcards
What is Ivermectin used for?
What is Ivermectin used for?
Signup and view all the flashcards
How is Ivermectin administered?
How is Ivermectin administered?
Signup and view all the flashcards
Study Notes
Antifungal and Antiparasitic Drugs
-
These drugs treat infections caused by fungi and parasites.
-
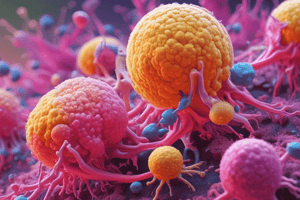
Images show different types of fungal infections.
-
Common fungal diseases: ringworm, athlete's foot, jock itch, ringworm of the scalp, onychomycosis, vaginal candidiasis, oral thrush.
- Ringworm ('tinea corporis'): Affects body skin, caused by Trichophyton, Microsporum, & Epidermophyton.
- Athlete's foot ('tinea pedis'): Affects the feet, often between toes.
- Jock itch ('tinea cruris'): Affects armpits, groin, & thighs.
- Ringworm of the scalp ('tinea capitis'): Affects scalp hair follicles, mostly in children.
- Onychomycosis ('tinea unguium'): Fungal infection of the nails, affecting fingernails and toenails.
- Vaginal candidiasis: Vaginal yeast infection caused by Candida albicans.
- Oral thrush: Candida albicans infection in the mouth, throat, and esophagus.
-
Fungal diseases that affect people with compromised immune systems: aspergillosis, candidiasis, cryptococcosis, invasive candidiasis, pneumocystis pneumonia (PCP).
- Aspergillosis: Caused by molds Aspergillus flavus and Aspergillus fumigatus.
- Candidiasis: Serious infection if grows uncontrollably or enters deep into the body.
- Cryptococcosis: Cryptococcus neoformans infection of the brain causing meningitis.
- Invasive candidiasis: Serious infections affecting blood, brain, eyes, bones, and other body parts (mostly in hospitalized patients).
- PCP: Serious infection caused by Pneumocystis jirovecii (renamed Pneumocystis carinii).
Common Antifungal Drugs
- Examples of common antifungal drugs are shown.
- Different classes of drugs are shown.
Polyenes
- Polyenes are drugs obtained from Streptomyces species.
- Example drugs: amphotericin B, natamycin, nystatin.
- Polyenes bind to ergosterol in the fungal cell membrane, disrupting it and causing leakage of intracellular ions.
Echinocandins
- Echinocandins are lipopeptide molecules that block the synthesis of β-glucan.
- β-glucans are carbohydrate polymers crucial to fungal cell walls, akin to bacterial peptidoglycans.
- Example drugs: caspofungin, anidulafungin, micafungin.
- Effective against invasive candidiasis and some strains resistant to fluconazole.
Amphotericin B
- Primary antifungal for most pathogenic Candida species.
- Not water-soluble, administered intravenously.
- Optimal dose: 0.5–1.0 mg/kg/day once daily.
- Dose may be increased if no substantial toxicity.
- Immature blood-brain barrier (BBB) in neonates has higher amphotericin B concentrations in cerebrospinal fluid (CSF) compared to adults.
- Toxicities include bone marrow suppression, anemia, thrombocytopenia, renal failure, hypokalemia, abnormal hepatic enzymes, and decreased urine output.
Flucytosine (5-FC)
- Also known as Ancobon.
- Oral and intravenous administration.
- Weak antifungal properties and rapid resistance development.
- Commonly used in combination with other antifungals.
- Distributed in breast milk, so use during pregnancy requires careful consideration.
- Well-absorbed from the gastrointestinal tract (GIT).
Terbinafine
- Also called Lamisil.
- Treats fungal nail infections and skin infections (ringworm, jock itch, athlete's foot).
- Effective in cream/ointment form, but less so for deep nail infections.
- Oral granules and tablets are used for scalp infections and onychomycosis (nail fungus).
- Long elimination half-life (200–400 hours).
- Highly lipophilic, accumulating in hair, skin, nails, and fatty tissues.
- Inhibits the enzyme squalene epoxidase, preventing ergosterol synthesis, which damages the fungal cell walls.
Griseofulvin
- Orally administered for treating ringworm infections, particularly when topical treatments fail.
- Binds to keratin, making it resistant to fungal infection.
- Interferes with fungal cell division by inhibiting microtubule function.
- Absorption is increased with a fatty meal.
Invasive Fungal Infections (IFIs)
- Significantly risky among immunocompromised patients.
- Risk factors include neutropenia, hematological malignancies, bone marrow transplant, prolonged corticosteroid use, prolonged hospitalization, chemotherapy, HIV infection, malnutrition, severe burns, and solid organ transplantation.
- Often requires combination therapy (complementary agents with diverse mechanisms).
Azoles
- Structurally related group of antifungals (e.g. fluconazole, itraconazole, voriconazole, posaconazole, isavuconazole).
- Commonly used to treat systemic mycoses and IFIs.
- Inhibits lanosterol synthesis to ergosterol in the fungal cell (inhibition of cytochrome P450).
Malaria
- Caused by Plasmodium species and transmitted by Anopheles mosquitos.
- Symptoms include fever, chills, flu-like symptoms, headache, vomiting, diarrhea, jaundice, cough, and discharge from eyes.
- Cycles (F-R-C) are repeated every 1-3 days.
- Types of malaria species and complications: P. falciparum (cerebral malaria, black water fever, pregnancy malaria); P. vivax, P. malariae, P. ovale, and P. knowlesi.
Antimalarial Drugs
- Drugs used to prevent and treat malaria.
- Examples are quinine, chloroquine, artemisinin derivatives (artemether, artesunate), suramin, metronidazole.
Other Protozoa and Helminthic Infections
- Non-malarial protozoa infections often treated with suramin, metronidazole, or ivermectin.
- Helminthic (worm) infections often treated with ivermectin, albendazole, pyrantel pamoate, or other drugs.
Topical Antifungal Drugs (TAfDs)
- Drugs applied directly to the skin, nails, or scalp to treat fungal skin conditions.
- Includes clotrimazole, miconazole, terbinafine, ketoconazole as examples.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.