Podcast
Questions and Answers
What is the primary route of excretion of amphotericin B?
What is the primary route of excretion of amphotericin B?
- Lymphatic system
- Kidney
- Bile (correct)
- Liver
Why is hospitalization recommended during the initiation of amphotericin B therapy?
Why is hospitalization recommended during the initiation of amphotericin B therapy?
- To reduce the risk of anemia
- To ensure proper administration technique
- To allow for close observation of infusion-related reactions (correct)
- To monitor for nephrotoxicity
What is the primary goal of administering a test dose of amphotericin B?
What is the primary goal of administering a test dose of amphotericin B?
- To assess the severity of potential allergic reactions (correct)
- To gauge the effectiveness of the therapy
- To monitor for nephrotoxicity
- To determine the optimal dosage regimen
What is the most significant of the slower toxicities associated with amphotericin B therapy?
What is the most significant of the slower toxicities associated with amphotericin B therapy?
How can infusion-related toxicity associated with amphotericin B therapy be diminished?
How can infusion-related toxicity associated with amphotericin B therapy be diminished?
What is the approximate half-life of the terminal phase of elimination of amphotericin B due to its extensive binding to tissues?
What is the approximate half-life of the terminal phase of elimination of amphotericin B due to its extensive binding to tissues?
What is the reason why fluconazole is less toxic than ketoconazole?
What is the reason why fluconazole is less toxic than ketoconazole?
What is the most common side effect of fluconazole?
What is the most common side effect of fluconazole?
What is the mechanism of action of amphotericin B?
What is the mechanism of action of amphotericin B?
What is the mechanism of action of fluconazole?
What is the mechanism of action of fluconazole?
What is the indication for IV administration of miconazole?
What is the indication for IV administration of miconazole?
Why is amphotericin B not recommended as a first-choice treatment for intestinal candidiasis?
Why is amphotericin B not recommended as a first-choice treatment for intestinal candidiasis?
What is the combination of clotrimazole-betamethasone used for?
What is the combination of clotrimazole-betamethasone used for?
What is the primary reason for hospitalizing patients receiving amphotericin B treatment?
What is the primary reason for hospitalizing patients receiving amphotericin B treatment?
What is the effect of fluconazole on the plasma concentration of certain drugs?
What is the effect of fluconazole on the plasma concentration of certain drugs?
How can the risk of nephrotoxicity associated with amphotericin B be minimized?
How can the risk of nephrotoxicity associated with amphotericin B be minimized?
What is the characteristic feature of the structure of amphotericin B?
What is the characteristic feature of the structure of amphotericin B?
Why is liposomal amphotericin B used in some cases?
Why is liposomal amphotericin B used in some cases?
Flashcards are hidden until you start studying
Study Notes
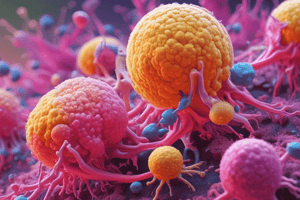
Amphotericin B Pharmacology
- Amphotericin B elimination is unchanged in anephric patients.
- Hepatic or biliary disease has no known effect on the metabolism of the drug in humans.
- The primary route of excretion is through the bile.
- No dose adjustment is required in patients with compromised renal or hepatic function.
- The terminal phase of elimination has a half-life of approximately 15 days due to extensive binding to tissues.
Amphotericin B Untoward Effects
- All patients receiving amphotericin B therapy should be hospitalized, at least during the initiation of therapy.
- A test dose of 1 mg i.v. should be administered to gauge the severity of the reaction and guide the initial dosing regimen and premedication strategy.
- Infusion-related toxicity includes fever, chills, electrolyte imbalance, GI disturbances, and hypotension.
- Slower toxicity includes nephrotoxicity, liver test abnormalities, and anemia due to reduced production of erythropoietin by damaged renal tubular cells.
- Renal damage is the most significant of the slower toxicity, and renal impairment is seen in all patients treated with therapeutic doses of amphotericin B.
Mechanism of Action
- Amphotericin B is a polyene antibiotic that binds to ergosterol, reducing the level of ergosterol in the fungal cell membrane.
- It has the broadest spectrum of activity among all antifungal drugs.
- It is used as a "magic bullet" for systemic fungal infections, but is also the most toxic.
Administration and Precautions
- Intrathecal infusion is used for fungal meningitis.
- Low lipid solubility prevents it from crossing the blood-brain barrier.
- It is not recommended for oral administration due to its ineffectiveness.
- It should be administered IV, but not metabolized by the liver, to avoid toxicity.
- A low amount can cross the placenta, but it is still toxic and should be avoided during pregnancy.
- Hospitalization is necessary to monitor and reverse any toxic effects that may appear.
- Premedication with antihistamines and antipyretics can help alleviate adverse effects.
Interactions and Side Effects
- Rifampin and tetracyclin can enhance the activity of amphotericin B.
- Nephrotoxicity can be reduced by pre-hydration, monitoring plasma levels, and combination therapy with flotazin.
- Liposomal amphotericin B is associated with fewer toxic effects.
- The most common side effect is GI distress, and other possible side effects include allergic rash, eosinophilia, transient abnormalities of hepatic function, and thrombocytopenia.
- It can increase plasma concentrations of phenytoin, sulfonylureas, warfarin, and cyclosporine.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.