Podcast
Questions and Answers
Which of the following is NOT a cause of secondary peritonitis?
Which of the following is NOT a cause of secondary peritonitis?
- Cirrhosis with ascites (correct)
- Perforated peptic ulcer
- Appendicitis with rupture
- Perforated intestine
What is the primary goal of surgical intervention for peritonitis?
What is the primary goal of surgical intervention for peritonitis?
- Administering antibiotics
- Monitoring vital signs
- Relieving abdominal pain
- Draining purulent fluid and repairing damage (correct)
What is the most common clinical problem experienced by patients with peritonitis?
What is the most common clinical problem experienced by patients with peritonitis?
- Pain (correct)
- Impaired GI function
- Risk for infection
- Fluid imbalance
What is the most prevalent cause of peritonitis?
What is the most prevalent cause of peritonitis?
Which of the following is NOT a component of conservative treatment for peritonitis?
Which of the following is NOT a component of conservative treatment for peritonitis?
Which of the following is NOT a typical symptom of peritonitis?
Which of the following is NOT a typical symptom of peritonitis?
What is the purpose of NG suction in the management of peritonitis?
What is the purpose of NG suction in the management of peritonitis?
What is the primary purpose of peritoneal aspiration in diagnosing peritonitis?
What is the primary purpose of peritoneal aspiration in diagnosing peritonitis?
Which of the following diagnostic assessments is NOT routinely used in the diagnosis of peritonitis?
Which of the following diagnostic assessments is NOT routinely used in the diagnosis of peritonitis?
Which clinical manifestation is a direct result of the body's attempt to isolate the infection in peritonitis?
Which clinical manifestation is a direct result of the body's attempt to isolate the infection in peritonitis?
Which of the following nursing interventions is NOT recommended for patients with peritonitis?
Which of the following nursing interventions is NOT recommended for patients with peritonitis?
How does a perforated ulcer contribute to the development of peritonitis?
How does a perforated ulcer contribute to the development of peritonitis?
What is the primary goal of postoperative care for a patient with peritonitis?
What is the primary goal of postoperative care for a patient with peritonitis?
What laboratory test would be performed to assess the presence of hemoconcentration in a patient with peritonitis?
What laboratory test would be performed to assess the presence of hemoconcentration in a patient with peritonitis?
What is the primary purpose of administering antibiotics to patients with peritonitis?
What is the primary purpose of administering antibiotics to patients with peritonitis?
Which diagnostic imaging modality can visualize ascites and abscesses in a patient with peritonitis?
Which diagnostic imaging modality can visualize ascites and abscesses in a patient with peritonitis?
Which of the following is a potential complication of peritonitis?
Which of the following is a potential complication of peritonitis?
What is the significance of dilated loops of bowel on an abdominal x-ray in a patient with peritonitis?
What is the significance of dilated loops of bowel on an abdominal x-ray in a patient with peritonitis?
Flashcards
Peritonitis
Peritonitis
Inflammation of the peritoneum due to infection or irritation.
Primary peritonitis
Primary peritonitis
Infection occurring from blood-borne organisms entering the peritoneal cavity without other abdominal issues.
Secondary peritonitis
Secondary peritonitis
Inflammation resulting from perforation or rupture of abdominal organs releasing contents into the cavity.
Common causes of secondary peritonitis
Common causes of secondary peritonitis
Signup and view all the flashcards
Clinical manifestations of peritonitis
Clinical manifestations of peritonitis
Signup and view all the flashcards
Complications of peritonitis
Complications of peritonitis
Signup and view all the flashcards
Diagnostic studies for peritonitis
Diagnostic studies for peritonitis
Signup and view all the flashcards
Initial response to peritonitis
Initial response to peritonitis
Signup and view all the flashcards
Primary Peritonitis Causes
Primary Peritonitis Causes
Signup and view all the flashcards
Secondary Peritonitis Causes
Secondary Peritonitis Causes
Signup and view all the flashcards
Diagnostic Assessment for Peritonitis
Diagnostic Assessment for Peritonitis
Signup and view all the flashcards
NPO Status
NPO Status
Signup and view all the flashcards
Drug Therapy for Peritonitis
Drug Therapy for Peritonitis
Signup and view all the flashcards
Fluid Imbalance in Peritonitis
Fluid Imbalance in Peritonitis
Signup and view all the flashcards
Nursing Management Assessment
Nursing Management Assessment
Signup and view all the flashcards
Postoperative Care for Peritonitis
Postoperative Care for Peritonitis
Signup and view all the flashcards
Goals of Peritonitis Care
Goals of Peritonitis Care
Signup and view all the flashcards
Study Notes
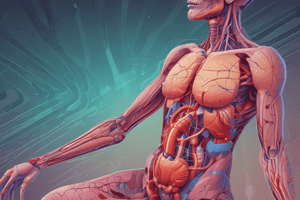
Peritonitis: Etiology and Pathophysiology
- Peritonitis is inflammation of the peritoneum caused by contamination.
- Contamination sources include bacteria, chemicals, or both.
- Common causes are listed in a table [not included].
- Primary peritonitis: blood-borne organisms enter the peritoneal cavity, unrelated to other abdominal problems. Ascites (fluid buildup) from liver cirrhosis creates a bacterial breeding ground.
- Secondary peritonitis: more common, caused by ruptured or perforated abdominal organs. Ruptured appendix, ulcers, diverticulitis, trauma are common causes.
- Released contents (bile, enzymes, bacteria) irritate the sterile peritoneum initially causing chemical peritonitis.
- Bacterial peritonitis follows, causing fluid shifts (edema) and adhesions.
Clinical Manifestations
- Main symptom: severe, continuous abdominal pain.
- Tenderness over the affected area is a universal sign.
- Rebound tenderness, rigidity, and spasm indicate peritoneal irritation.
- Patients often lie still, breathing shallowly.
- Other symptoms: abdominal distention, fever, tachycardia, tachypnea, nausea, vomiting, altered bowel habits.
- Severity of symptoms varies based on the condition's severity and suddenness.
- Potential complications: hypovolemic shock, sepsis, intra-abdominal abscesses, paralytic ileus, and acute respiratory distress syndrome.
- Peritonitis can be fatal if treatment is delayed.
Diagnostic Studies and Interprofessional Care
- Complete Blood Count (CBC): used to assess white blood cell count (WBC) and hemoconcentration.
- Peritoneal aspiration: fluid analysis for blood, bile, pus, bacteria, fungus, and amylase. Allows for examination and biopsy of the peritoneum.
- Abdominal X-ray: assesses bowel dilation (paralytic ileus), free air (perforation), or air/fluid levels (obstruction).
- Ultrasound and CT scans: identify ascites (fluid buildup) and abscesses.
- Peritoneoscopy may help assess patients without ascites.
Management of Peritonitis
- Conservative Care: milder cases or poor surgical candidates. Includes antibiotics, nasogastric (NG) suction, analgesics, and IV fluids.
- Surgical Care: needed to find the cause, drain fluid, and repair damaged organs (e.g., perforated organs).
Nursing Management: Assessment and Clinical Problems
- Assessment focuses on pain location and quality, bowel sounds, abdominal distention, guarding, nausea, fever, and signs of shock.
- Clinical problems include pain, fluid imbalances, impaired GI function, and infection risk.
Nursing Management: Planning and Implementation
- Goals include treating inflammation, easing pain, avoiding complications (sepsis, shock), and achieving normal nutrition.
- IV access is crucial for fluid replacement, antibiotics, and pain management.
- Pain monitoring and response to analgesics. Positioning for patient comfort.
- Sedatives may be used.
- Close monitoring of fluids, electrolytes, and vital signs are essential.
- Antiemetics are used to reduce nausea and vomiting.
- Patients are placed on nothing-by-mouth (NPO) status.
- NG tubes may be needed for suctioning.
- Oxygen therapy as needed.
- Drains are used postoperatively to remove excess fluid.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.