Podcast
Questions and Answers
Which of the following best describes the primary function of the perichondrium?
Which of the following best describes the primary function of the perichondrium?
- To facilitate the exchange of gases within bone marrow.
- To supply nutrients to cartilage and aid in its growth and repair. (correct)
- To act as a shock absorber between articulating bones.
- To provide structural support and rigidity to bone tissue.
In long bones, what is the main function of the epiphyseal line?
In long bones, what is the main function of the epiphyseal line?
- It is a source of bone-forming cells during fracture repair.
- It facilitates nutrient exchange within the compact bone.
- It is a remnant of the growth plate and indicates where bone lengthening occurred. (correct)
- It provides structural support to the medullary cavity.
What is the primary role of osteoclasts in bone remodeling?
What is the primary role of osteoclasts in bone remodeling?
- To regulate calcium exchange between bone and blood.
- To differentiate into osteocytes.
- To break down bone tissue and release minerals. (correct)
- To synthesize new bone matrix.
Which of the following is a key difference between compact and spongy bone at the microscopic level?
Which of the following is a key difference between compact and spongy bone at the microscopic level?
Which of the following best describes the role of mechanical stress in bone remodeling?
Which of the following best describes the role of mechanical stress in bone remodeling?
Which type of cartilage is characterized by its high tensile strength and ability to resist compression, making it ideal for locations like the intervertebral discs?
Which type of cartilage is characterized by its high tensile strength and ability to resist compression, making it ideal for locations like the intervertebral discs?
Which of the following best describes the function of canaliculi in bone tissue?
Which of the following best describes the function of canaliculi in bone tissue?
Which of the following is the correct sequence of zones in long bone lengthening?
Which of the following is the correct sequence of zones in long bone lengthening?
What is the primary difference between intramembranous and endochondral ossification?
What is the primary difference between intramembranous and endochondral ossification?
Which of the following hormones primarily lowers blood calcium levels?
Which of the following hormones primarily lowers blood calcium levels?
Flashcards
Structure of Perichondrium
Structure of Perichondrium
Dense irregular connective tissue that surrounds cartilage (except at joints).
Function of Perichondrium
Function of Perichondrium
Provides nutrients to cartilage, resists outward expansion during compression, and aids in growth and repair.
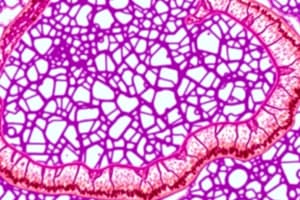
Hyaline Cartilage
Hyaline Cartilage
Smooth, glassy appearance, composed of fine collagen fibers, provides support with some flexibility and reduces friction, located in articular surfaces of bones, nose, trachea, costal cartilage, embryonic skeleton.
Fibrocartilage
Fibrocartilage
Signup and view all the flashcards
Cartilage
Cartilage
Signup and view all the flashcards
Bone
Bone
Signup and view all the flashcards
Axial Skeleton
Axial Skeleton
Signup and view all the flashcards
Appendicular Skeleton
Appendicular Skeleton
Signup and view all the flashcards
Long bones
Long bones
Signup and view all the flashcards
Short bones
Short bones
Signup and view all the flashcards
Study Notes
Structure and Function of the Perichondrium
- The perichondrium is a dense irregular connective tissue that surrounds cartilage, except at joints.
- It provides nutrients to cartilage, resists outward expansion during compression, and aids in growth and repair.
Hyaline Cartilage vs. Fibrocartilage
- Hyaline cartilage has a smooth, glassy appearance and is composed of fine collagen fibers.
- It provides support with some flexibility and reduces friction.
- It is located on articular surfaces of bones, nose, trachea, costal cartilage, and embryonic skeleton.
- Fibrocartilage has thick collagen fibers and is less firm than hyaline cartilage.
- It has high tensile strength, resists compression, and absorbs shock.
- It is located in intervertebral discs, pubic symphysis, and menisci of the knee.
Comparison of Cartilage and Bone
- Cartilage is flexible, avascular, contains chondrocytes in lacunae, and has a matrix of collagen and elastic fibers.
- Bone is rigid, vascularized, contains osteocytes in lacunae, and has a matrix of collagen fibers and calcium salts.
Seven Important Functions of Bone Tissue
- Support
- Protection (e.g., skull, rib cage)
- Movement (levers for muscles)
- Mineral storage (calcium, phosphate)
- Blood cell formation (hematopoiesis in red marrow)
- Triglyceride (fat) storage (yellow marrow)
- Hormone production (osteocalcin for insulin regulation)
Two Major Groups of Bones in the Skeleton
- Axial skeleton: skull, vertebral column, rib cage.
- Appendicular skeleton: limbs and girdles (pectoral & pelvic).
Four Bone Classes with Examples
- Long bones: longer than wide (e.g., femur, humerus).
- Short bones: cube-shaped (e.g., carpals, tarsals).
- Flat bones: thin, flattened (e.g., skull, ribs, sternum).
- Irregular bones: complex shapes (e.g., vertebrae, hip bones).
What Distinguishes Sesamoid Bones?
- Sesamoid bones develop within tendons and enhance leverage (e.g., patella).
Compact vs. Spongy Bone
- Compact bone is dense, smooth, and forms the outer layer.
- Spongy bone is porous, made of trabeculae, and is found inside bones.
Gross Anatomy of Short, Irregular & Flat Bones
- They lack a diaphysis and epiphysis, and a thin compact bone layer surrounds spongy bone.
Gross Anatomy of Long Bones
- Diaphysis (shaft), epiphyses (ends), medullary cavity (marrow)
Diaphysis (Medullary Cavity & Contents)
- The shaft of a long bone contains yellow marrow (fat storage).
Epiphyses & Epiphyseal Line
- The ends of long bones are covered by articular cartilage, with an epiphyseal line (remnant of growth plate).
Function & Location of Red Marrow
- Function: blood cell formation.
- Location: spongy bone of flat bones, epiphyses of long bones (in adults).
Periosteum Structure & Function
- Structure: Outer fibrous layer, inner osteogenic layer with osteoblasts/osteoclasts.
- Function: bone growth, repair, attachment for tendons/ligaments.
Endosteum vs. Periosteum
- Endosteum: thin membrane lining medullary cavity, contains bone-forming cells.
- Periosteum: outer covering of bone, provides structural support.
Osteon Structure of Compact Bone
- Haversian system: central canal surrounded by concentric lamellae, contains blood vessels & nerves.
Central Canal vs. Perforating Canal
- Central canal runs parallel and contains vessels/nerves.
- Perforating canal runs perpendicular and connects central canals.
Lacunae & Canaliculi Relationship
- Lacunae: small cavities housing osteocytes.
- Canaliculi: tiny canals connecting lacunae for nutrient exchange.
Interstitial vs. Circumferential Lamellae
- Interstitial lamellae are between osteons, remnants of old osteons.
- Circumferential lamellae are outer layers around the entire bone.
Five Bone Cell Types
- Osteogenic cells: stem cells.
- Osteoblasts: bone-forming cells.
- Osteocytes: maintain bone.
- Osteoclasts: break down bone.
- Bone lining cells: regulate calcium exchange.
Structure & Function of Osteoid
- Organic part of bone matrix (collagen & proteins), provides flexibility.
Inorganic Components of Bone
- Hydroxyapatite (calcium phosphate) provides hardness.
Bone Resorption (Cells & Process)
- Osteoclasts secrete enzymes & acids to break down bone.
Microscopic Structure of Spongy Bone vs. Compact Bone
- Similar: both have lamellae, osteocytes.
- Different: no osteons in spongy bone, contains trabeculae.
Osteogenesis vs. Bone Growth
- Osteogenesis is bone formation during embryonic development.
- Bone growth is lengthening & thickening after birth.
Two Osteogenesis Pathways
- Intramembranous: skull & clavicle (bone forms in connective tissue).
- Endochondral: long bones (cartilage template replaced by bone).
Steps in Long Bone Lengthening (Zones)
- Resting Zone → Proliferation Zone → Hypertrophic Zone → Calcification Zone → Ossification Zone.
Appositional Growth (When & How?)
- Thickening occurs throughout life via periosteum.
Growth & Thyroid Hormones in Bone Growth
- GH stimulates growth and TH regulates proportions.
Estrogen & Bone Growth
- Promotes growth spurt and closes growth plates.
Vitamins & Minerals for Bone Growth
- Calcium, phosphate, vitamin D, C, A, K.
Why Bone Remodeling Matters
- Prevents bone from becoming brittle and adapts to stress.
How Mechanical Stress Affects Bone Remodeling
- More stress = more bone deposition.
Blood Calcium Homeostasis (Feedback System & Hormones)
- Hormones: PTH (raises Ca²⁺) and Calcitonin (lowers Ca²⁺).
Types of Fractures
- Open (compound), closed (simple), greenstick, comminuted, spiral, compression, epiphyseal.
Four Stages of Bone Healing
- Hematoma formation → Fibrocartilaginous callus formation → Bony callus formation → Bone remodeling.
Paget's Disease
- Excessive bone remodeling results in weak bones.
Osteoporosis & Risk Factors
- Bone resorption > formation. Risk factors: aging, low estrogen, poor diet.
Osteomalacia vs. Rickets
- Osteomalacia: soft bones (adults).
- Rickets: soft bones (children, vitamin D deficiency).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.